Few studies report the epidemiological profile of RA patients attending clinics for comprehensive care. We describe the clinical, socio-demographic characteristics and comorbidities of a cohort of patients with RA.
MethodsCross-sectional study in a cohort of patients according to ACR criteria/EULAR 2010 classification who have entered to the AR clinic since October 2012 until May 2014, referred from primary care. Frequencies for socio-demographic, comorbidity, state of disease activity, functional status, biomarkers and therapeutic modalities variables are described.
ResultsIn total, 1652 patients were included with a mean age of 58 years and a duration of 9 years. Rheumatoid factor was positive in 80% and anti-citrullinated peptide antibody in 63% of patients. In total, 43.6% of patients had comorbidities: Hypertension (20.4%), osteoporosis (17.3%) and Sjögren's syndrome (10.4%). Fifty percent of the patients had moderate and high disease activity level measured by DAS-28 score, and the mean HAQ score was 0.64 (DS 1.12). Seventy three percent of patients were treated with oral disease modified anti rheumatic treatment and 63.6% of them were with methotrexate. 42.4% of the patients were treated with glucocorticoids (mean dose 6.3mg).
ConclusionsThe epidemiological behavior of a group of RA patients is reported. The presence of comorbidities is significant affecting the risk of morbidity and mortality in these patients. The definition of the epidemiological profile of this population will allow the design of research questions to resolve outstanding problems in the clinical context of this pathology.
Existen pocos estudios que reporten el perfil epidemiológico de pacientes con AR que asisten a clínicas especializadas de atención integral. Nuestro objetivo es describir las características clínicas y sociodemográficas, y las comorbilidades de pacientes con AR en una clínica de atención integral.
MétodosEstudio transversal en una cohorte de pacientes según criterios de clasificación ACR/EULAR-2010 que han ingresado a la clínica de AR desde octubre del 2012 hasta mayo del 2014 remitidos del primer nivel de atención. Se describen las frecuencias para las variables sociodemográficas, comorbilidades, estado de actividad de la enfermedad, estado funcional, biomarcadores y modalidades terapéuticas.
ResultadosSe incluyó a 1.652 pacientes con promedio de edad de 58 años y tiempo de evolución de 9 años. El factor reumatoide fue positivo en el 80% y los anticuerpos antipéptido citrulinados en el 63% de los pacientes. El 43,6% de los pacientes presentaban comorbilidades asociadas: hipertensión arterial (20,4%), osteoporosis (17,3%) y síndrome de Sjögren (10,4%). El 50% de los pacientes se encontraba en moderada y alta actividad de la enfermedad medido por DAS-28 y el promedio±desviación estándar del valor del puntaje HAQ al ingreso fue de 0,64±1,12. El 73% del total de pacientes estaban en tratamiento con modificadores de la enfermedad por vía oral, de los cuales el 63,6% estaba con metotrexato. El 42,4% de los pacientes recibían tratamiento con glucocorticoides (dosis promedio 6,3mg).
ConclusionesSe reporta el comportamiento epidemiológico de un grupo de pacientes con AR. Es significativa la presencia de comorbilidades que influyen en el riesgo de morbimortalidad de estos pacientes. La definición del perfil epidemiológico de esta población permitirá el diseño de preguntas de investigación que permitan resolver problemas relevantes en el contexto clínico de esta patología.
Rheumatoid arthritis (RA) is a common chronic disease that affects approximately 1% of the population, with a peak incidence between the ages of 35 and 50 years.1 It mainly affects women and, although the cause is unknown, different endocrine, environmental and genetic factors have been identified as being involved in its onset, development and progression.2,3 The disease is characterized by inflammation of the synovial membrane, which predominantly compromises small joints of the hands and feet. It is associated with systemic complications that have a negative impact from the biopsychosocial point of view4 and important consequences for public health.5
The rate of morbidity among RA patients is higher than that of the general population, and cardiovascular events and other systemic complications, such as osteoporosis, are a great challenge in the management of these patients.6 Several of these comorbidities are observed more frequently in patients with RA, due to the medical treatment they receive, especially glucocorticoids, and because of the traditional risk factors, like tobacco use.7 In addition, the activity of the inflammatory process constitutes a predisposing factor for the development of these comorbidities.8
The prevalence of RA in northern Europe and North America ranges between 0.5% and 1%, whereas in southern Europe, a prevalence ranging from 0.3% to 0.7% has been reported. On the other hand, in developing countries, the reported prevalence ranges between 0.1% and 0.5%.9 In Colombia, we do not have reliable information on the prevalence and incidence of this condition, although isolated efforts have been made to estimate them. Studies have been published that analyze economic variables in terms of providing care for these patients10 or report variables of disability and loss of healthy life-years.11 According to the 2005 census, in Colombia, there must be approximately 200,000 patients with RA, including the juvenile RA patient population.
The severity of RA has been established in accordance with the presence or absence of prognostic factors, such as positive tests for rheumatoid factor and anti-cyclic citrullinated peptide antibodies, presence of bone erosions, extraarticular involvement and the existence of comorbidities, among others. These factors influence the recommendations for drug therapy issued in the international guidelines for the treatment of this disease,12 which stress the importance of early diagnosis and appropriate treatment as major objectives in the follow-up of these patients.
Early diagnosis and treatment enable better control of the inflammatory process and delay structural damage, along with its functional implications.13 In this context, the integrated management approach is highly important in stimulating patients’ adherence and adaptation to the treatment,14 requirements that are essential for the achievement of a level of control of the disease that is high enough to delay joint destruction and conserve the functional status.
Very little information has been published on the morbidity burden and/or the description of epidemiological profiles for this disease in Colombia.15 Thus, the objective of this study is to describe the major clinical and epidemiological features and the comorbidities in a cohort of RA patients, in a specialized clinic in which care was provided by a group of professionals from different areas related to the integrated approach to this condition.
Materials and MethodsPatientsWe included all the RA patients who had been admitted to the integrated care clinic for that disease between 1 October 2012 and 31 May 2014. For information gathering, the patient data were retrieved from the electronic health record, the admissions database of the hospitals from which they had been referred, the central authorization office, the institutional registry of disabilities and the follow-up carried out by the nursing staff of the clinic. A database was designed using the aforementioned sources, and was consolidated every 4 weeks in order to identify erroneous and/or missing data and to ensure an adequate quality control method.
Design, Population and Definition of VariablesWe conducted a cross-sectional descriptive study in a cohort of patients with established RA who met the 2010 ACR/EULAR classification criteria.16 A nonprobability convenience sampling method was applied in a cohort of those individuals who were being treated in the RA outpatient clinic in the Centro Médico de Palermo, which is the referral center for individuals covered by the private health care provider, Sanitas, in Bogotá. There they are attended to by a multidisciplinary team composed of 3 rheumatologists, nurses, family medicine physicians, a nutritionist, a psychologist and a physical therapist. The population comprises patients, from all age groups, with a previously established diagnosis of RA or a high index of clinical suspicion for inflammatory arthropathy, referred from all the primary care centers (general practitioners, family medicine physicians and/or internists), which constitute the doorway to the health system.
The patients were consecutively enrolled on the basis of their having met the classification criteria for RA and the opinion of the treating rheumatologist. Clinical measurements were made using variables applied in rheumatology, such as the level of disease activity measured by the Disease Activity Score (DAS28),17 a validated composite index, and the measurement of the functional status using a questionnaire designed for that purpose (Health Assessment Questionnaire [HAQ]).18 Data on the anti-cyclic citrullinated peptide antibody titer, rheumatoid factor and acute-phase reactants—C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)—were included. The comorbidities were evaluated on the basis of diagnoses associated with the underlying disease recorded in the clinical history. These conditions are screened periodically, with the cooperation of family medicine physicians, by means of bone densitometry, chest radiography, electrocardiography and lipid and metabolic profiles in the initial assessment. They included cardiovascular disease (hypertension, cerebrovascular disease), osteoporosis, Sjögren's syndrome, diabetes mellitus, anemia, pulmonary and chronic renal disease, lymphoma and tuberculosis. To obtain information on hospital admissions, we cross-checked the identification data of all the patients with the records of admissions provided by the hospitals in which the patients were being treated.
Statistical AnalysisThe descriptive analysis of each variable to be studied was performed. Measures of central tendency and of variability were utilized to describe the characteristics of the study population. For continuous variables, the measures of central tendency, mean and median were used, the latter for a dataset including extreme values. The nominal and ordinal variables are expressed as absolute values and proportions. The absolute and relative frequencies were established for the sociodemographic variables and comorbidities, and measures of central tendency and dispersion were calculated for each clinical indicator evaluated with continuous data. The Stata™ software package (version 12) was used for the statistical analysis of the data.
Ethical ConsiderationsAs this is a descriptive study, in which there was no intervention whatsoever involving the patients, it was considered to be low-risk and it was not necessary to obtain written informed consent. There was no intentional intervention in, or modification of, the biological, physiological, psychological or social variables of the participating individuals. The absolute confidentiality of the collected data was ensured. Those data were used only for strictly scientific purposes in accordance with the principles declared in the ethical standards established for research in humans, according to the Nuremberg code, to the Declaration of Helsinki (World Medical Association [Helsinki, 1964]) and to the articles of resolution 008430, dated 1993, of the Ministry of Health and Social Protection of the Republic of Colombia (Scientific, Technical and Administrative Standards for Health Research). The information was stored in the database as provided for in Colombian Law 1582 of 2012, in accordance with the policies of confidentiality, privacy and security.
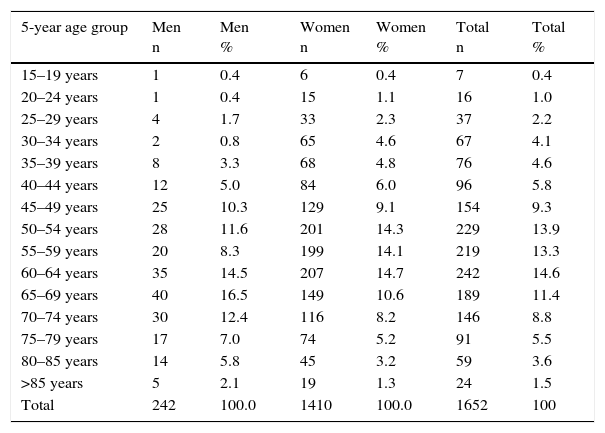
ResultsIn all, 1652 patients were evaluated and included in the analysis. The mean age was 58 years and 85.3% of the patients were women, for a female-to-male ratio of 6:1. Fifty percent of the participants were under 58 years of age. The minimum age was 16 years and the maximum, 93 years. The distribution according to 5-year age groups and the population pyramid of the cohort are shown in Table 1. As can be seen, the largest groups correspond to the 5-year period from age 65 to 69 for men and from age 50 to 54 for women. The serum rheumatoid factor levels were positive in 80% of the patients (n=457/567) and anti-cyclic citrullinated peptide antibodies were detected in 63% (n=363/573). In all, 13.6% of the patients had a family history of RA, and there were no significant gender-related differences between men (13.6%) and women (13.5%).
Distribution of the Population Attended to in the Rheumatoid Arthritis Clinic According to 5-year Age Groups.
| 5-year age group | Men n | Men % | Women n | Women % | Total n | Total % |
|---|---|---|---|---|---|---|
| 15–19 years | 1 | 0.4 | 6 | 0.4 | 7 | 0.4 |
| 20–24 years | 1 | 0.4 | 15 | 1.1 | 16 | 1.0 |
| 25–29 years | 4 | 1.7 | 33 | 2.3 | 37 | 2.2 |
| 30–34 years | 2 | 0.8 | 65 | 4.6 | 67 | 4.1 |
| 35–39 years | 8 | 3.3 | 68 | 4.8 | 76 | 4.6 |
| 40–44 years | 12 | 5.0 | 84 | 6.0 | 96 | 5.8 |
| 45–49 years | 25 | 10.3 | 129 | 9.1 | 154 | 9.3 |
| 50–54 years | 28 | 11.6 | 201 | 14.3 | 229 | 13.9 |
| 55–59 years | 20 | 8.3 | 199 | 14.1 | 219 | 13.3 |
| 60–64 years | 35 | 14.5 | 207 | 14.7 | 242 | 14.6 |
| 65–69 years | 40 | 16.5 | 149 | 10.6 | 189 | 11.4 |
| 70–74 years | 30 | 12.4 | 116 | 8.2 | 146 | 8.8 |
| 75–79 years | 17 | 7.0 | 74 | 5.2 | 91 | 5.5 |
| 80–85 years | 14 | 5.8 | 45 | 3.2 | 59 | 3.6 |
| >85 years | 5 | 2.1 | 19 | 1.3 | 24 | 1.5 |
| Total | 242 | 100.0 | 1410 | 100.0 | 1652 | 100 |
At the moment of enrollment of the patients in the program, we found a mean time since diagnosis of 9.2±9.0 years and a median of 7.0±7.0 years, with a minimum of 0 years (diagnosed at the time of enrollment) and a maximum of 64 years. In all, 25.5% of the patients had a history of RA of less than 24 months at the time they began to be treated at the RA clinic. However, a total of 50% of the patients had a history of the disease of more than 9 years, a fact that illustrates the chronicity of this condition. In all, 11.66% of the patients (n=153) were diagnosed once they had come to the rheumatology clinic, 84.9% (n=130) during their first contact with the rheumatologist and 15% (n=23) at a later visit.
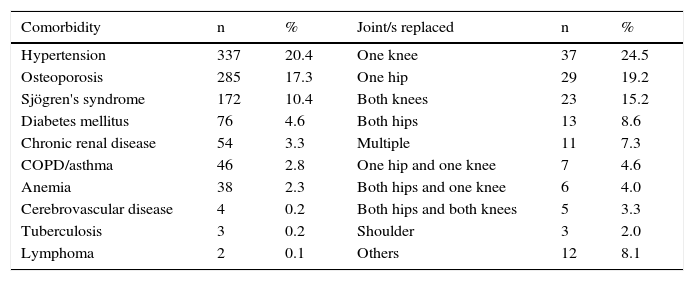
Joint replacement was documented in 151 patients (9.1%). The most frequent intervention was that involving 1 knee (24.5%), followed by 1 hip (19.2%), both knees (15.2%) and both hips (8.9%). The distribution in terms of percentages is shown in Table 2.
Distribution of Comorbidities and Joint Replacements in the Patient Cohort Expressed as Percentages.
| Comorbidity | n | % | Joint/s replaced | n | % |
|---|---|---|---|---|---|
| Hypertension | 337 | 20.4 | One knee | 37 | 24.5 |
| Osteoporosis | 285 | 17.3 | One hip | 29 | 19.2 |
| Sjögren's syndrome | 172 | 10.4 | Both knees | 23 | 15.2 |
| Diabetes mellitus | 76 | 4.6 | Both hips | 13 | 8.6 |
| Chronic renal disease | 54 | 3.3 | Multiple | 11 | 7.3 |
| COPD/asthma | 46 | 2.8 | One hip and one knee | 7 | 4.6 |
| Anemia | 38 | 2.3 | Both hips and one knee | 6 | 4.0 |
| Cerebrovascular disease | 4 | 0.2 | Both hips and both knees | 5 | 3.3 |
| Tuberculosis | 3 | 0.2 | Shoulder | 3 | 2.0 |
| Lymphoma | 2 | 0.1 | Others | 12 | 8.1 |
COPD, chronic obstructive pulmonary disease.
Overall, 4.5% the patients reported being active smokers. On the other hand, 43.6% of them had comorbidities associated with RA, especially hypertension (20.4%), osteoporosis (17.3%) and Sjögren's syndrome (10.4%). Table 2 shows the frequencies of comorbidities of the members of the cohort.
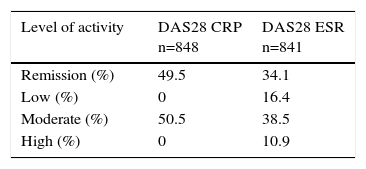
Level of Disease Activity and Functional Status of the PatientsThe level of RA activity (DAS28/CRP and DAS28/ESR) in the cohort patients when they began coming to the clinic can be observed in Table 3. We included only the data of those patients for whom we had complete information in order to be able to calculate the DAS. When DAS28/CRP was used to evaluate the level of activity, we found that half of the population was capable of performing moderate activity. Likewise, according to DAS28/ESR, half of the population was capable of moderate and vigorous activity. The mean±standard deviation of the HAQ score at the time of enrollment was 0.64±1.12 (95% confidence interval, 0.57–0.71) (Table 4).
Distribution of the Level of Disease Activity Measured by the Disease Activity Score 28 (DAS28) Calculated With C-reactive protein (CRP) and With the Erythrocyte Sedimentation Rate (ESR) and Expressed as Percentages.
| Level of activity | DAS28 CRP n=848 | DAS28 ESR n=841 |
|---|---|---|
| Remission (%) | 49.5 | 34.1 |
| Low (%) | 0 | 16.4 |
| Moderate (%) | 50.5 | 38.5 |
| High (%) | 0 | 10.9 |
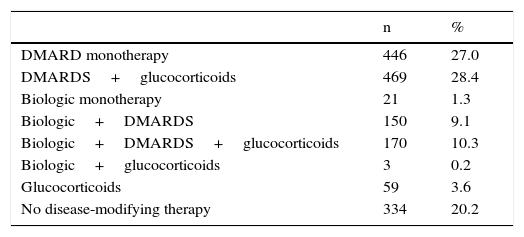
Distribution of the Therapeutic Strategies Utilized in the Patient Cohort Expressed as Percentages.
| n | % | |
|---|---|---|
| DMARD monotherapy | 446 | 27.0 |
| DMARDS+glucocorticoids | 469 | 28.4 |
| Biologic monotherapy | 21 | 1.3 |
| Biologic+DMARDS | 150 | 9.1 |
| Biologic+DMARDS+glucocorticoids | 170 | 10.3 |
| Biologic+glucocorticoids | 3 | 0.2 |
| Glucocorticoids | 59 | 3.6 |
| No disease-modifying therapy | 334 | 20.2 |
DMARDS, synthetic disease-modifying antirheumatic drugs.
Oral disease-modifying antirheumatic drugs (DMARDS) were being used to treat 73% of the total patient cohort, 63.6% of whom were being treated with methotrexate (MTX), 35% with chloroquine (CQ) and 32% with leflunomide. The mean dose of MTX was 12.1mg. The combination most widely used was MTX+CQ, which was being received by 9.6%. Finally, 42.4% of the patients were being treated with glucocorticoids (n=701) at a mean dose of 6.3mg. Of this subgroup, 8.4% (n=59) were taking glucocorticoids alone, 66.9% (n=469) in combination with oral DMARDS and 24.2% (n=170) in combination with oral DMARDS plus biologic DMARDS.
DiscussionIn the present study, we describe the epidemiological profile and comorbidities of a group of 1652 patients with a diagnosis of RA who are being treated in an outpatient clinic with a multidisciplinary approach to this disease. The characteristics described coincide with those reported in previous studies, with a similar disease burden and a marked preponderance of cardiovascular and metabolic complications, typical of a degenerative chronic disease.
In the analysis of the distribution according to gender in the cohort, we observe a greater preponderance of the female gender than in other population groups (ratio of 6:1), in agreement with reports in the Latin American literature.19 Potential contributing factors are the lower proportion of men who visit their physicians and/or the fact that men take the joint symptoms too lightly, and the higher proportion of men who self-medicate (anti-inflammatory agents). Another factor could be the approach in primary care to the onset of joint symptoms in men, which are frequently interpreted as being associated with crystal arthropathy or osteoarthritis. These circumstances lend emphasis to the importance of educational activities in these aspects. These gender-related differences in behavior should be studied in greater detail in future research.
Moreover, this population has a high rate of chronicity and, given the time since diagnosis (9 years) and the number of joint replacements (n=151), it also meets a greater number of the criteria for severe disease. In addition, there is a correlation with the presence of factors associated with a poor prognosis reported in the literature,20 such as the percentage of patients with positive tests for rheumatoid factor (80%) and anti-cyclic citrullinated peptide antibodies (63%). These findings agree with those previously documented in an urban mestizo population in Peru21 and in Mexico.22 The therapeutic strategies and prognosis in this clinical setting differ significantly from other cohorts, in which getting individuals to visit their physician and identifying those with RA in early stages, before structural damage can develop, would result in better intermediate and long-term clinical outcomes.23 Likewise, the high percentage of patients capable of performing moderate-to-vigorous activity (50%), the use of glucocorticoids (43%) and the lack of treatment with DMARDS in 25% of the patients reflect the need for and the importance that patients to be evaluated directly by a rheumatologist, in an integrated care setting to ensure their proper follow-up, comorbidity assessment and treatment.
Taking the mean age into account, we detect chronic diseases that are characteristic of the age group, which probably have an effect on the risk of morbidity in these patients (for example, cardiovascular, metabolic). This is correlated with previous data from the region, which estimate the importance of the identification of risk factors, especially cardiovascular, for patients with this condition.24 Thus, the design of additional interventions focusing on the strict control and follow-up of these comorbidities is of great importance for achieving a positive impact on clinical outcomes. The application of scoring systems like the Framingham score25 to evaluate cardiovascular risk and the collaboration of specialists in family medicine will enable early intervention to achieve a positive impact on these patients.
One of the main objectives of RA clinics is periodical and regular follow-up of patients, in accordance with the aims for the management and follow-up of these patients established in international guidelines.26 However, it is important to point out that the periodicity of follow-up should be individualized according to the features of the disease of each patient.
The objectives and results of our report are in accordance with the mission of PANLAR to promote and harmonize minimum standards for quality of life through the documentation of the level of disease activity, comorbidities and treatment in RA patients.27 In addition, it provides additional, complementary information from a referral center for clinical practice in Latin America that contributes to previous efforts aimed at providing real-world data and improving care for these patients.28
Our study has a number of limitations. First, the inclusion of patients from a single national referral center in Colombia and the cross-sectional study design impede it from being completely representative at the national level. Moreover, the registry of the case histories used as an information source was not designed for use in the research project, that is, it is intended merely for health care purposes, not for academic ends. Secondly, the radiological examination was not included and, thus, it was not possible to evaluate structural damage or progression through the reading and scoring of images as an outcome measure. Furthermore, there was no active search for comorbidities, a circumstance that could lead to the underestimation of their frequency. However, in future studies, in addition to radiologic follow-up, we plan to include other important outcome measures, such as the evaluation of quality of life, depression and adherence to treatment, using validated questionnaires.
The clear definition of the epidemiological profile of this population would enable the design and implementation of better care processes based on the information gathered and analyzed. This study contributes useful information with respect to the epidemiological and clinical behavior of a cohort of RA patients, and will aid in the design and implementation of better care processes, which is much needed in Colombia, where there is little available information. Moreover, it will enable the generation of hypotheses and will set down the bases of future population-based research projects, for the purpose of designing strategies to deal with relevant problems associated with this disease in the clinical setting. Finally, it will enable the establishment a strong baseline for the follow-up of the tracking variables of the clinical and preventive interventions of the program.
ConclusionsIn conclusion, we describe the epidemiological behavior of a cohort of patients with RA in Colombia. This report will serve as the basis for conducting local prevalence studies that enable the design of strategies to achieve an early positive impact on patients with this disease. Moreover, this study becomes the baseline for posing new research questions and hypotheses that will aid in resolving relevant problems associated with this disease in the clinical setting.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors declare that they have no source of funding for the performance of this study.
Conflicts of InterestThe authors declare they have no conflicts of interest.
We especially thank the patients for allowing us to study them for this report. Likewise, we thank the group of collaborators that formed the interdisciplinary team, who contributed their knowledge and support for the integrated management of and approach to these patients.
Please cite this article as: Bautista-Molano W, Fernández-Avila D, Jiménez R, Cardozo R, Marín A, Soler MP, et al. Perfil epidemiológico de pacientes colombianos con artritis reumatoide evaluados en una clínica especializada de atención integral. Reumatol Clin. 2016;12:313–318.