Epithelioid sarcoma represents less than 1% of soft tissue sarcomas and has a high recurrence rate and strong ability to invade the regional lymphatic pathways. Classic epithelioid sarcoma has a predilection for young men and usually affects the distal extremities, while the proximal-type is characterized by different histological features and most commonly occurs in the proximal part of the extremities, trunk and pelvis. Intraosseous tumor development is rare.
We describe a 47-year old patient with sacroiliac pain mimicking sacroiliitis. A computed tomography of the pelvis showed a destructive intraosseous lesion of the upper-right iliac. Percutaneous biopsy of the lesion was obtained and histological findings were typical of classic epithelioid sarcoma. To our knowledge, this is the second case of intraosseous epithelioid sarcoma described in the medical literature.
El sarcoma epitelioide representa menos del 1% de los sarcomas de partes blandas, posee una elevada capacidad para invadir los linfáticos regionales y alta tasa de recurrencias. Las formas clásicas se localizan preferentemente en la porción distal de las extremidades y afectan sobre todo a varones jóvenes, mientras que las formas proximales, además de características histológicas diferentes, tienden a situarse en el tronco, la pelvis y la raíz de las extremidades. El desarrollo intraóseo de este sarcoma es excepcional.
En este artículo describimos a un paciente de 47 años que consultó por dolor en la región sacroilíaca derecha imitando una sacroilitis. La tomografía computarizada pélvica objetivó una lesión osteolítica en la región posterosuperior del ilíaco derecho, de la que se obtuvieron muestras mediante biopsia percutánea. Los hallazgos histológicos fueron típicos de sarcoma epitelioide clásico. En nuestro conocimiento, este es el segundo caso descrito en la literatura en que esta neoplasia se desarrolla primariamente en el tejido óseo.
Epithelioid sarcoma (ES), first described in 1970 by Enzinger,1 expresses immunohistochemical markers characteristic of epithelial cells such as epithelial membrane antigen, vimentin and keratins.2 Despite its relatively indolent course, it has great potential to spread across the lymph nodes and recur after surgical excision.3
Against the classic SE, typically originated in the deep tissue of the extremities and forming nodules, there is a proximal variant, more aggressive, with greater capacity to metastasize, normally found on the trunk, pelvis and axial regions, whose first 18 cases were reported in 1997 by Guillou et al.4 During growth, SE may involve adjacent bony structures,5 but the involvement of the axial skeleton is rare.6 To date, we have located only one description of primary bone7 SE, which is why we considered it of interest to make a new contribution. This is a 47-year old male in whom the tumor caused an osteolytic lesion of the right iliac bone and simulated extended sacroiliitis.
Case ReportA 47-year old male with a history of smoking, appendectomy, vasectomy and osteoporosis treated with risedronate 35mg weekly since 2 years earlier. He was seen in our rheumatology unit for lumbosacral pain radiating to the right, which intensified when he got up from a chair or while climbing or descending stairs, but did not interfere with sleep.
The examination revealed a wide arc dorsal kyphosis, pain on direct pressure over the right sacroiliac joint and the opening and closing the joint. There were no other abnormalities on physical examination.
The hematological tests as well as glucose, urea, creatinine, GOT, AST, ALT, GGT, bilirubin, cholesterol, triglycerides, uric acid, calcium, phosphorus, alkaline phosphatase, lactictate dehydrogenase, sodium, potassium, testosterone, TSH, T4, 25 (OH) 2D3 and PTH were normal. Chest radiographs showed an increased bronchovascular network. The lumbar radiographs visualized incipient degenerative changes. On the frontal radiograph of the pelvis there was a poorly defined radiolucent image of the posterior portion of the right ilium, that projected into the upper third of the sacroiliac joint (Fig. 1A). Computed tomography (CT) visualized thoracoabdominal and pelvic osteolytic geographical lesions with density similar to that of the adjacent soft tissues, involving both cortical and trabecular bone, without expansion and no periosteal reactive neoformation (Fig. 1B). In addition, we found a nodule with irregular borders of about 6mm in diameter in the right upper lung lobe without hilar lymphadenopathy. A bone scan with 99mTc objectified focal uptake of the tracer limited to the affected area on the right ilium (Fig. 1C).
(A) X ray frontal projection of the pelvis of the patient in which an osteolytic lesion may be seen with lobulated contours and septums in the interior. (B) Computerized tomography. Axial cut of the sacroiliac joints showing a lytic area with no bone growth or reactive sclerosis that destroys the cortex. (C) Bone phase of 99mTc diphosphate methylene marked radionuclide scan, in which an uptake of the posterior portion of the right iliac bone adjacent to the sacroiliac joint may be seen.
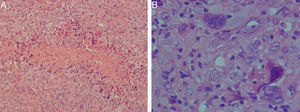
We performed a biopsy of the lesion, which showed necrotic areas surrounded by mononuclear epithelioid cells, which were arranged diffusely in a dense collagenous stroma. The cells were monomorphic, with a vesicular nucleus, prominent nucleoli and a high mitotic rate. In some areas we identified strongly atypical and multinucleated forms (Fig. 2). The tumor cells expressed epithelial membrane antigen, vimentin and cytokeratin. No staining was observed with actin, desmin, S100 protein, CD34, CD31 and CD99.
With the diagnosis of right iliac SE and metastases of the right upper lung lobe, the patient was treated with radical surgery, chemotherapy (ifosfamide and adriamycin) plus radiotherapy with a linear accelerator (total dose of 2000cGy). After 4 years of follow thoracoabdominal and pelvic CT scans showed an increased volume of pulmonary nodules (12mm) and the development of osteolytic metastasis in the right iliopubic branch. A positron emission tomography with fluoride-18 showed deoxyglucose radiotracer uptake in the right lung nodule and in the right iliopubic branch and posterior region of the right iliac crest.
DiscussionAlthough SE is less than 1% of all soft tissue sarcomas, Jawad et al.8 described a progressive increase in annual incidence from 1973 to 2005, reaching 0.41 cases per one million inhabitants. It predominates in males (1.8:1) and more than half of cases are diagnosed before age 45.2
Classic SE tends to occur in a young adult as a poorly defined subcutaneous nodule, which ranges between 3 and 6cm. It can be confused with granulomas, sebaceous cysts, fungal infections, lymphadenitis, nodular fasciitis or other skin injuries.5,9 Proximal SE tends to be localized on the trunk, pelvis, at the root of the limbs, genitals and perineal7 region.
Pain is the presenting symptom in only 20% of patients with SE,2 contributing to the difficulty in diagnosis.2 There have been 4 SE cases of intra-articular origin, which presented severe arthropathy.10 Intraosseous tumor development is outstanding. In 2009, Raoux et al.7 described the first case in a 31-year-old woman with left hip and joint involvement. In our patient, the tumor extended, clinically mimicking sacroiliitis.
Radiological findings in proximal SE are nonspecific and of limited value in diagnosis. Bone involvement is usually by contiguity, with the appearance of erosions or a thinning cortex.2 Peripheral calcifications are rare and may even be heterotopic bone11 formation. CT usually shows one or more soft tissue masses of lobulated contours and poorly defined microcalcifications which can be viewed and present areas of necrosis.
Histological examination usually shows multiple nodules with poorly defined boundaries in which the tumor cells, usually epithelioid, with ovoid nucleus and eosinophilic cytoplasm, are arranged around areas of necrosis.9 In some cases the cells are fusiform or even have a rhabdoid phenotype, a frequent finding in cases of “proximal” sarcoma-like epithelioid. The histologic pattern of SE described, unlike Raoux et al.7 published, was typical of the “classic” or distal variety.
Immunohistochemical positivity is characteristic for cytokeratins, vimentin, epithelial membrane antigen and, in 50% of cases, CD34. In over 80% of the ES there is no activity of the INI1 tumor suppressor gene, located on the long arm of chromosome 22, which exposes DNA to transcription5 factors.
The recommended treatment is radical surgery or excision with the largest perilesional margin possible. Some locations of the tumor, invasion or involvement of regional lymph vessels and nerves,2,9 may preclude these options and sometimes it is necessary to use adjuvant radiotherapy and chemotherapy.
Survival at 5 years of diagnosis is between 60% and 75%. Invasion of the regional nodes and distant metastases are independent factors associated with decreased survival.
In the case presented and, despite radical surgery, radiotherapy and chemotherapy, local recurrence has been observed after a 4-year follow-up, with right iliopubic branch and lung metastases.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that no patient data appears in this article.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
DisclosureThe authors have no disclosures to make.
Please cite this article as: Gómez Rodríguez N, et al. Sarcoma epitelioide del ilíaco derecho imitando una sacroilitis. Reumatol Clin. 2012. http://dx.doi.org/10.1016/j.reuma.2012.03.008.