The esophageal involvement in systemic sclerosis (SSc) causes impact in the morbidity and mortality. High resolution manometry assesses esophageal involvement. Our aim was to categorize esophageal motor disorder in patients with SSc by HRM.
MethodsWe carried out an observational, descriptive and cross-sectional study. All patients underwent HRM as well as semi-structured interviews to assess frequency and severity of upper GI symptoms. Patients also completed the gastroesophageal reflux questionnaire (Carlsson–Dent).
ResultsWe included 19 patients with SSc, 1 with morphea, and 1 with scleroderma sine scleroderma. Dysphagia and heartburn were the most frequent symptoms (61% each). We found an abnormal HRM in 15 (71.4%) patients. We found no statistically significant association between clinical or demographic variables and an abnormal HRM, or between any upper GI symptom and HRM findings.
ConclusionWe observed a high prevalence of esophageal symptoms and of HRM abnormalities. However, there was no clear association between symptomatology and HRM findings. HRM does not seem to accurately predict upper GI symptomatology.
La afectación esofágica en la esclerosis sistémica causa impacto en la morbimortalidad. La manometría de alta resolución evalúa la afectación esofágica. Nuestro objetivo fue categorizar el trastorno motor esofágico en pacientes con esclerosis sistémica por HRM.
MétodosSe realizó un estudio observacional, descriptivo y transversal. Todos los pacientes se sometieron a HRM, así como a entrevistas semiestructuradas para evaluar la frecuencia y la gravedad de los síntomas gastrointestinales. Los pacientes también completaron el cuestionario de reflujo gastroesofágico (Carlsson-Dent).
ResultadosSe incluyeron 19 pacientes con esclerosis sistémica, uno con morfea y uno con esclerodermia seno esclerodermia. La disfagia y la pirosis fueron los síntomas más frecuentes (un 61% cada uno). Encontramos una HRM anormal en 15 (71,4%) pacientes. No se halló ninguna asociación estadísticamente significativa entre las variables clínicas o demográficas y una HRM anormal, o entre cualquier síntoma GI superior y los hallazgos de HRM.
ConclusiónSe observó una alta prevalencia de síntomas esofágicos y de anomalías de la HRM. Sin embargo, no hubo asociación clara entre la sintomatología y los hallazgos de HRM. La HRM no parece predecir con precisión la sintomatología gastrointestinal.
Systemic sclerosis (SSc) is an autoimmune disease of unknown cause characterized by microvasculopathy, fibroblast activation, and excessive production of collagen.1
Involvement of the gastrointestinal (GI) tract in SSc is second in frequency only to the skin, and it is characterized by esophageal dysmotility in 75–90%, stomach involvement in 50%, small bowel involvement in 40–70%, colon involvement in 20–50%, and anorectal involvement in 50–70%.2 The mortality rate attributable to GI involvement is 6–12%.3–7
The great impact of esophageal involvement in the morbi-mortality of SSc is related to its association with interstitial lung disease,8 weight loss and malnutrition, Barrett's esophagus9,10 and its progression to adenocarcinoma.11 Around 18–40% of patients are asymptomatic despite the objective documentation of esophageal disease.10 Esophageal manometry is considered the method of choice for evaluation of esophageal motility in SSc patients, even when they are asymptomatic.
A new technique called high resolution manometry (HRM) in which catheters with 36 pressure sensors separated by 1cm are used to measure intraesophageal pressure from the hypopharynx to the stomach, was introduced recently. The result is a color picture of the topography of esophageal pressure, where the duration, amplitude and velocity of esophageal contractions (including the function of the upper and lower esophageal sphincter) are plotted.12 Traditionally, manometric findings were reported as rated by Spechler and Castell.13 From 2008 onwards (and with the introduction of the HRM) a new classification (The Chicago classification) was described, and is currently the most widely used classification.14,15 The aim of this study was to categorize esophageal motor disorder in patients with SSc by HRM and to describe its association with upper GI symptomatology.
Materials and methodsSetting and populationThis is an observational, descriptive and cross-sectional study, carried out between May and August 2013 in a Tertiary-care University Hospital. This study was approved by the ethics committee of our Institution. We selected patients >18 years old with SSc according to the American College Classification 1980 with or without esophageal symptoms who accepted to enter to the study with a signed informed consent. Also, we included only two patients other than SSc, one with morphea and other with scleroderma sine scleroderma, both of them with esophageal symptoms.
We evaluated clinical and demographics variables including: age, gender, body mass index (BMI), SSc classification, auto-antibodies, previously use of nonsteroidal anti-inflammatory drug (NSAID), calcium channel blockers (CCB) and proton pump inhibitors (PPIs). We asked about esophageal symptoms using a semi-structured interview and recorded the frequency of: dysphagia, heartburn, regurgitation, cough, chest pain, nausea, vomiting. We also evaluated skin thickening, gastro esophageal reflux symptoms, and dysphagia symptoms.
Modified Rodnan skin score (mRSS)The mRSS is a validated measure of skin thickening in SSc. In the mRSS, skin thickening is assessed at 17 body sites by palpation and rated on a scale with values of 0 (normal), 1 (mild), 2 (moderate) or 3 (severe skin thickening). The total skin score is the sum of the individual skin assessments in the 17 body areas, with a possible range of 0–51; higher scores indicate more severe skin thickening.
Carlsson–Dent questionnaireWe applied a gastroesophageal reflux questionnaire (Carlsson–Dent) to all patients, which has been used in Spanish-speaking Mexican patients previously.16 It is a self-administered questionnaire that focuses on the nature of the sensations experienced by the patient as well as provoking, exacerbating and relieving factors. Scores range from −7 to 20. Scores of −7 to −1 indicate ‘absent’ reflux symptoms, 0–5 ‘mild’, 6–11 ‘moderate’ and >11 ‘severe’ reflux symptoms.
DysphagiaWe classified dysphagia in four stages according to patient self-report: no dysphagia, dysphagia to liquid food, dysphagia to normal solids, dysphagia to soft solids and inability to swallow.
High resolution manometry (HRM)HRM was done by a certified gastroenterologist (GBT) with experience using HRM. Seven days prior to HRM, we withheld the following drugs: prokinetics, narcotics, anticholinergics, antiemetics, and anti-inflammatory drugs. We asked the patient to fast the night before the procedure. The day of the study the patient was placed supine. Subsequently, topical anesthetic is applied in nostril. The manometry catheter was placed in a site that allowed to identify areas of both sphincters, placing about 5 sensors in the stomach and finally the probe was attached to the back of the nose. After a stabilization period of 5min, 10 consecutive shots of 5ml of water were administered every 30s.17 HRM results were reported according to the Chicago classification.14–18 Patients with normal EGJ pressure, normal EGJ relaxation, normal PFV, and a DCI <5000mm Hg s cm were reported as normal or abnormal if the gastroenterologist reported one of the following based in manometric parameters: Peristaltic dysfunction; aperistalsis, hypertensive peristalsis; rapidly propagated pressurization; abnormal LES tone (end expiratory); achalasia or functional obstruction.
Statistical analysisContinuous variables with normal distribution were expressed with mean and standard deviation. Continuous variables without normal distribution were expressed with median and interquartile ranges. We categorized HRM results in two groups: Normal or abnormal HRM (any alteration), then, we used 2×2 contingency tables. In addition, chi-square or Fisher exact tests were used according to their distribution to assess whether there was an association between each variable and the HRM results. A value of p<0.05 was considered statistically significant. All statistical analyses were performed using the SPSS version 20.0 statistical software package. This work has been assessed and approved by the local IRB with registration: RE13-006.
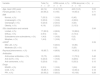
ResultsWe included 21 patients, 19 with SSc, 1 with morphea, and 1 with scleroderma sine scleroderma. Seventeen patients (80.9%) had less than three years of being diagnosed. Most patients were female (95.2%) with mean age of 44.9 (SD 14) years, a mean weight of 61.9kg (SD 14.4) and height of 1.57 (SD 0.8) m; the other clinical and demographic variables are in Table 1. We found 17 (80.9%) patients with limited SSc. The mean mRSS for all patients was 9.7 (SD 7.4). Raynaud's phenomenon was reported in 18 (85.7%) patients.
Clinical and demographic variables compared with HRM results.
| Variable | Total (%) n=21 | HRM normal, n (%) n=6 | HRM abnormal, n (%) n=15 | p |
|---|---|---|---|---|
| Age, mean (SD) years | 44 (14) | 41.2 (10.2) | 44.6 (14.3) | 0.63 |
| Female gender, n (%) | 20 (95.2) | 6 (100) | 14 (93.3) | 0.71 |
| BMI | 0.55 | |||
| Normal, n (%) | 7 (33.3) | 1 (16.6) | 6 (40) | |
| Underweight, n (%) | 5 (23.8) | 1 (16.6) | 4 (26.6) | |
| Overweight, n (%) | 5 (23.8) | 2 (33.3) | 3 (20) | |
| Obesity, n (%) | 4 (19) | 2 (33.3) | 2 (13.3) | |
| SSc classification and variants | 0.94 | |||
| Limited, n (%) | 17 (80.9) | 4 (66.6) | 13 (86.6) | |
| Diffuse, n (%) | 2 (9.5) | 0 (0) | 2 (13.3) | |
| Scleroderma sine scleroderma, n (%) | 1 (4.8) | 1 (16.6) | 0 (0) | |
| Morphea, n (%) | 1 (4.8) | 1 (16.6) | 0 (0) | |
| mRSSa | 0.39 | |||
| Mild <20, n (%) | 5 (83.3) | 12 (80) | ||
| Moderate ≥20, n (%) | 0 (0) | 3 (20) | ||
| Raynaud phenomenon, n (%) | 18 (85.7) | 4 (66.6) | 14 (93.3) | 0.18 |
| Antibodies | ||||
| Antinuclear antibodies, n (%) | 15 (75) | 4 (66.6) | 11 (73.3) | 0.48 |
| Anti-Scl70, n (%) | 5 (23.8) | 1 (16.6) | 4 (26.6) | 0.51 |
| Anti-centromere, n (%) | 5 (23.8) | 0 (0) | 5 (33.3) | 0.15 |
| Drugs | ||||
| NSAID, n (%) | 2 (9.5) | 1 (16.6) | 1 (6.6) | 0.50 |
| CCB, n (%) | 18 (85.7) | 4 (66.6) | 14 (93.3) | 0.18 |
| PPI, n (%) | 20 (95.2) | 5 (83.3) | 15 (100) | 0.28 |
SSc, systemic sclerosis; SD, standard deviation; BMI, body mass index; mRSS, modified Rodnan skin score; NSAID, nonsteroidal anti-inflammatory drug; CCB, calcium channel blockers; PPI, proton pump inhibitors; HRM, high resolution manometry.
We found a normal HRM in 6 (28.5%) patients and an abnormal HRM in 15 (71.4%) patients. Patients with an abnormal HRM were: 1 (6.6%) patient with distal esophageal spasm, 5 (33.3%) patients with absent peristalsis, 4 (26.6%) patients with weak peristalsis with small peristaltic defects, and 3 (20%) patients with frequent failed peristalsis. Only 2 (13.3%) patients in whom an abnormal HRM was found could not be classified.
The association between upper GI symptoms and HRM results is shown in Table 2. Dysphagia and heartburn were the most frequent symptoms reported by the patients, but in general, symptom frequency did not vary between groups with or without HRM abnormalities. Only regurgitation was found to be more frequent in patients with a normal HRM. Additionally, neither the Carlsson–Dent questionnaire nor dysphagia severity was different between groups. Two patients with limited SSc who were asymptomatic (one patient with absent peristalsis and the other with weak peristalsis with small peristaltic defects) showed an abnormal HRM. The two variant SSc patients (scleroderma sine scleroderma and morphea) had a normal HRM.
Association between upper GI symptoms and HRM results.
| Variable | Total (%) n=21 | HRM normal, n (%) n=6 | HRM abnormal, n (%) n=15 | p |
|---|---|---|---|---|
| Esophageal symptoms, n (%) | ||||
| Dysphagia | 13 (61.9) | 4 (66.6) | 9 (60) | 0.59 |
| Heartburn | 13 (61.9) | 3 (50) | 10 (66.6) | 0.41 |
| Regurgitation | 9 (42.9) | 5 (83.3) | 4 (26.6) | 0.02 |
| Cough | 10 (47.6) | 3 (50) | 7 (46.6) | 0.63 |
| Chest pain | 3 (14.3) | 2 (33.3) | 1 (6.6) | 0.18 |
| Nausea | 4 (19) | 2 (33.3) | 2 (13.3) | 0.31 |
| Vomiting | 1 (4.8) | 0 (0) | 1 (6.6) | 0.71 |
| CDQ, mean (SD) | 6.04 (4.4) | 0.59 | ||
| 0–3 score, n (%) | 8 (38) | 3 (50) | 5 (33.3) | |
| 4–15 score, n (%) | 13 (61.9) | 3 (50) | 10 (66.6) | |
| Dysphagia classification, n (%) | 0.37 | |||
| No dysphagia | 9 (42.8) | 4 (66.6) | 5 (33.3) | |
| Dysphagia to normal solidsa | 7 (53.8) | 1 (16.6) | 5 (33.3) | |
| Dysphagia to soft solidsa | 6 (46.1) | 1 (16.6) | 5 (33.3) | |
| 4–15 score, n (%) | 7 (33.3) | |||
CDQ, Carlsson–Dent questionnaire; HRM, high resolution manometry.
In this cohort of SSc patients, an abnormal HRM was found in 71.4%. Dysphagia and heartburn were the most common esophageal symptoms reported, which is similar to other published series.8–10 We did not find any association between clinical-demographic variables and the outcome of the HRM, or between upper GI symptoms and HRM findings, except for regurgitation, which was found to be more frequent in patients with a normal HRM.
There had been a previous study assessing the clinical features of Mexican scleroderma patients; Santos-Navarro et al.19 studied 60 patients and found hypotensive lower esophageal sphincter (LES) in 95%. Aperistalsis (41%), slight hypomotility (30%), and severe hypomotility (27%) with different gastric manifestations as: early satiety 45%, abdominal pain 35%, nausea 20% and vomiting 10%. In contrast with our study they did not intent to correlate the clinical findings with manometry ones. Also they performed standard manometry versus high resolution in our patients. Even tough, they found a high prevalence of manometry alterations, maybe explained by age differences between cohorts, and the established disease by ten years of more.
This is not the first study to find a lack of an association between esophageal dysmotility evaluated by HRM and upper GI symptomatology in patients with SSc. Roman et al. studied HRM findings in 51 patients with SSc, and found that 67.3% had HRM abnormalities (most commonly hypotensive esophagogastric junction). However, up to 87% of patients had esophageal symptoms that were not predictive of HRM alterations.20 Later, Tang et al. associated HRM findings with phenotypic and GI symptoms in 28 patients with SSc, and could not find a clear association between dysphagia and HRM findings.21 Recently, Raja et al. reported the finding of a study on 31 patients with SSc who underwent HRM.22 They found that upper GI symptoms were absent in the majority of their patients, even when they had severe esophageal involvement according to HRM findings. The same basic results were reported in another recent study involving 79 patients with SSc.23
It has been known for some time that the severity of upper GI symptoms does not always correlate with objective measures of esophageal dysmotility, and this may include HRM. In a retrospective study of over 250 patients who underwent HRM due to upper GI symptoms, these were not found to be related to abnormal motor function defined by HRM during liquid, viscous or solid bolus swallows in the upright position.24 The discordance that we observed in our study might not be limited to patients with SSc. Other studies on populations with systemic diseases that usually involve the esophagus, such as Chagas disease, have similarly found a lack of an association between HRM findings and upper GI symptomatology.25 Additionally, in our study, 95.2% of patients at the time of evaluation were treated with proton pump inhibitors (PPIs). The lack of association between the symptoms and the results of HRM may be also partly explained by the high percentage of patients using PPIs at the time of evaluation, or even the use of other non-prescription medications for heartburn that could mask the symptoms evaluated. This limitation was also seen in other study.21
On the other hand, there are certain features of SSc that have been more consistently associated with HRM alterations. Patients with SSc and Raynaud phenomenon have been found to have lower amplitude of distal esophageal contractions21 as well as with more hypotensive lower esophageal sphincter22 compared to those without. Degree of skin involvement has also been positively correlated with esophageal dysmotility according to HRM as well as with more severe dysphagia.21,23 The latter were not found in our cohort. The presence of pulmonary fibrosis in SSc patients was also found to be associated with more absent contractility in HRM as well as with more symptoms of gastroesophageal reflux.22,23 At least one study found that alterations in HRM were correlated to presence of Scl70 and absence of anti-centromere antibodies,20 but these findings were not replicated in another recent study.23 In our study we did not assess lung function, and neither the severity of skin involvement or presence of Raynaud phenomenon was significantly associated with HRM abnormalities, although there was a trend toward more alterations in patients with Raynaud phenomenon.
The patients with morphea and scleroderma sine scleroderma we included both had a normal HRM. Recently, Arif et al. evaluated SSc and morphea patients with upper gastrointestinal endoscopy, esophageal manometry and 24-h pH monitoring, and found that of the 31 patients with morphea, none had manometric findings, although only four patients had symptoms. The authors concluded that in morphea, an assessment of GI manifestations is not necessary, unlike SSc.26 We also observed two patients with SSc without esophageal symptoms but with an abnormal HRM. Previously, Thonhofer et al. conducted a retrospective study, where they evaluated patients with SSc and Mixed Connective Tissue Disease (MCTD) without GI symptoms. The patients underwent a baseline evaluation and follow-up at three to six months. In all thirteen SSc patients, significant pathology of the upper GI-tract was found. In patients with esophageal abnormalities, starting treatment led to favorable results, which was confirmed in the follow-up study. The authors suggest that the GI evaluation must be performed early in patients diagnosed with SSc, even if they do not report typical symptoms,27 an opinion that we share considering our results.
We consider that the strengths of the study are: a population with a relatively early diagnosis of SSc, the use of HRM and the Chicago classification. The limitations include: cross-sectional study design, small cohort of patients, heterogeneity in the treatment of patients, lack of description of other comorbidities that could affect the outcome of the HRM, as well as lack of further studies to complement the manometry result, such as pH monitoring or endoscopy.
In conclusion, we found a high prevalence of esophageal symptoms but a lack of association between these and the presence of an abnormal HRM, which is in accordance to other published, studies.19–22 This suggests that it is important to perform a systematic approach to GI symptomatology in SSc patients at diagnosis irrespective of objective procedures of motility evaluation. This will identify early GI abnormalities, help alleviate symptoms and thereby lessen the impact on morbidity and mortality generated by this condition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Funding sourcesNone.
Authors’ contributionArana-Guajardo AC: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; obtained funding; administrative, technical, or material support.
Barrera-Torres G: acquisition of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content.
Villarreal-Alarcón MA: study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; study supervision.
Vega-Morales D: study concept and design; acquisition of data; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; statistical analysis; study supervision.
Esquivel-Valerio JA: analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content.
Conflict of interestNone declared.