To describe patient's characteristics, the activity and patient's satisfaction with a multidisciplinary care unit in patients with psoriasis and psoriatic arthritis (PsA).
MethodsA retrospective medical records review of patients with psoriasis or PsA attended in a multidisciplinary care unit was performed. Included patients were contacted to fulfill a satisfaction questionnaire. A specific electronic database was set up. Data regarding to patients and their baseline characteristics and the activity of the unit were collected. Descriptive analysis were performed.
ResultsA total of 112 patients with 154 visits were included in almost 3 years, 54% women, with a mean age of 51 years, 43.7% presented hyperlipidemia and 30.4% arterial hypertension. Half of patients were referred due to diagnostic doubts and the other half for therapeutic problems. After the evaluation of the patients, 66 patients (58.9%) met diagnostic criteria for PsA, and 13 (11.6%) of an inflammatory disease other than PsA, and 95% came back to their usual physician. The most ordered test were laboratory tests (75.6% of patients), followed by X-rays in 57 patients (51.3%). In general the number of patients with different treatments increased, and 55.4% and 42% of patients changed their topic and systemic treatments respectively. The level of satisfaction was very high and all of patients considered that their disease was better controlled in this multidisciplinary care unit.
ConclusionsThis multidisciplinary care unit has improved the care and satisfaction of patients with psoriasis or PsA, and increased collaboration between rheumatology and dermatology departments.
Describir las características de los pacientes, la actividad registrada, así como la satisfacción percibida, de una consulta de atención multidisciplinar para pacientes con psoriasis o artritis psoriásica (APs).
MétodosEstudio observacional retrospectivo con revisión de historias clínicas de todos los pacientes atendidos en la consulta de atención multidisciplinar. Se contactó con todos ellos para que contestasen una encuesta de satisfacción. Varios investigadores recogieron datos sociodemográficos y clínicos, así como administrativos incluyendo el número de visitas en una base de datos especialmente generada para este proyecto. Se realizó un análisis descriptivo.
ResultadosSe incluyó a 112 pacientes con 154 visitas en casi 3 años, 54% mujeres, y una edad media de 51 años; el 43,7% presentó hiperlipidemia y el 30,4% hipertensión arterial. La mitad fueron referidos por dudas diagnósticas y la otra por problemas terapéuticos. Tras su evaluación, 66 pacientes (58,9%) cumplieron los criterios diagnósticos de APs y 13 (11,6%) de una enfermedad inflamatoria distinta. El 95% regresó a su médico habitual. La pruebas complementarias más solicitadas fueron analíticas (75,6%) y radiografías simples (51,3%). En general, el número de pacientes con nuevos tratamientos aumentó y el 55,4 y el 42% de los pacientes cambiaron sus tratamientos tópico y sistémico, respectivamente. El nivel de satisfacción fue muy alto y todos los pacientes consideraron que su enfermedad estaba mejor controlada en esta unidad.
ConclusionesEsta consulta de atención multidisciplinar ha mejorado el manejo y satisfacción de pacientes con psoriasis o APs y ha incrementado la colaboración entre los servicios de Reumatología y Dermatología.
Psoriasis is a chronic inflammatory skin disease characterized by raised, red scaly plaques. Psoriatic arthritis (PsA) is a heterogeneous chronic inflammatory disease that, apart from the skin may affect the peripheral and axial joints, entheses, skin and nails, and other organs.1–3
Epidemiologic studies have also shown that, in patients with psoriasis, but specially in those with PsA, associated comorbidities may occur more frequently than expected.4,5 Cardiovascular disease, metabolic syndrome, obesity, diabetes, fatty liver disease Crohn's disease, ophthalmic disease, depression and anxiety are common comorbidities in these patients.6
Taking into account all of this, psoriasis and PsA are heterogeneous and potentially severe diseases, that negatively impact patients quality of life.7,8
On the other hand, many of these patients are evaluated and managed by dermatologists and rheumatologist independently. However, in the dermatology clinics, PsA is not always suspected and therefore the diagnosis of the disease may be delayed.9,10 Furthermore, skin involvement sometimes has little or no attention for rheumatologists, even though it may have a considerable impact on the patient's physical and psychological health.11,12
In order to improve patient's outcomes and prognosis, national and international organizations as well as experts and patients recommend multidisciplinary treatment.13 In this context, in recent years, experiences from a few multidisciplinary care units or models for patients with psoriasis and PsA have been published in the literature.14,15 Although data from these units are still poor they suggest that skin and joint improved after the multidisciplinary consultation, were better considered compared with usual care and reported very high satisfaction levels. One of this units also described that after evaluation diagnosis and treatment were modified in 32% and 47% of cases, respectively.15
The aim of this study was to describe the experience of a multidisciplinary care unit where dermatologists and rheumatologists collaborate closely following pre-defined referral criteria and management protocols (see methods section for more information).
MethodsThis project was approved by the Ethics Committee of the Hospital Can Misses and patients gave informed consent.
Multidisciplinary Care UnitA multidisciplinary care unit with specialists with experience and interest in psoriatic disease (2 dermatologists, one rheumatologist) was established to attend routine patients with psoriasis or PsA. Specific referral criteria were generated including: (1) Diagnostic problems (e.g. patients with psoriasis and arthralgia/arthritis); (2) Therapy related issues (e.g. the prescription of a biologic therapy in refractory patients); (3) Comorbidity management; (4) Safety concerns. Before the unit was implemented, a member of this unit followed a trainee program in another multidisciplinary care unit. Patients are referred from the dermatology and rheumatology departments. Visits (once a month) are made in the rheumatology department in order to take advantage of infrastructure (units and nursing staff). When the patient's problems are solved, they return to their reference specialist for standard follow-up. Patients are evaluated and treated using national and international guidelines. Additional tests as laboratory tests, imaging techniques or biopsies are ordered if necessary.
DesignA retrospective observational study was performed. Medical records of patients attended in the multidisciplinary unit from August 2012 to December 2014 were reviewed. Included patients were contacted by telephone to come to the unit and complete the satisfaction questionnaire. However, if the patients was not able to come, the satisfaction questionnaire was completed by telephone. This was anonymous and patients gave informed consent.
Patient's Selection and Data AcquisitionPatients aged 18 or above attended in the unit were included. A specific electronic database was set up for the purpose of this project. The following data were collected: (a) sociodemographics (age, sex), smoking status; (b) clinical variables including comorbidities (cardiovascular disease, hyperlipidemia, arterial hypertension, Diabetes Mellitus, obesity, hyperuricemia, gout, depression, anxiety, uveitis, hepatic disease, others), baseline disease duration; (c) multidisciplinary care unit related variables like number of visits, follow-up, speciality of referral, main referral reason, referral reason by symptoms, final diagnosis (following international diagnostic criteria), final destination, laboratory tests, imaging techniques and others required during the study period, treatment and treatment changes (topical therapy, ultraviolet phototherapy, NSAIDs, systemic steroids, DMARDs, biologics); (d) satisfaction questionnaire. Patients were asked to (1) qualify from 10 (excellent) to 0 (very bad) the general attention in the multidisciplinary care unit, (2) describe the care of the multidisciplinary unit compared with your usual care (much better, better, the same, worse, much worse), (3) describe the quality of the information given in the multidisciplinary unit (very good, good, normal, bad, very bad), and (4) answer the following question: Was your disease better controlled in this multidisciplinary care unit?
Statistical AnalysesTo describe the sample, we used the distribution of frequencies, the mean and standard deviation, or the median and interquartile range, depending on the distribution of the variable.
ResultsA total of 112 patients were analyzed that produced 154 visits (range 1–7, 77% of patients only 1 visit, 16% 2, 7% ≥3 visits) in almost 3 years. There was no waiting list during this period. Mostly women (54%), with a mean age of 51 years±12 years, and 20.5% were smokers (Table 1). Mean psoriasis and PsA duration were 16±15 years and 6±7 years respectively. Interestingly, in our study population, 43.7% of patients presented hyperlipidemia, 30.4% arterial hypertension, and 27.7% anxiety. A total of 88 patients (78.6%) were referred from the rheumatology unit. We found that 95% of patients eventually returned to their responsible physician.
Baseline Characteristics of Study Sample.a
| Sex (woman) | 61 (54%) |
| Age (years)b | 51.4±12.8 |
| Psoriasis duration (years)b | 16±15 |
| PsA duration (years)b | 6±7 |
| Smoking status | |
| Yes | 23 (20.5%) |
| No | 82 (73.2%) |
| Former smoker | 7 (6.2%) |
| Comorbidity | |
| Cardiovascular | 4 (3.6%) |
| Hyperlipidemia | 49 (43.7%) |
| Arterial Hypertension | 34 (30.4%) |
| Diabetes Mellitus | 10 (8.9%) |
| Obesity | 24 (21.4%) |
| Hyperuricemia | 12 (10.7%) |
| Gout | 3 (2.7%) |
| Depression | 19 (17.0%) |
| Anxiety | 31 (27.7%) |
| Uveitis | 1 (0.9%) |
| Hepatic disease | 18 (16.1%) |
| Others | 17 (15.2%) |
| Visits to the multidisciplinary care clinicb | 1.4±0.9 |
| Speciality of referral (rheumatology) | 88 (78.6%) |
| Follow-up in the multidisciplinary care clinic (years)b | 0.2±0.5 |
Abbreviation: PsA, psoriatic arthritis.
The main reasons for being referral to the multidisciplinary unit (Table 2) were equally distributed between diagnostic and therapeutic doubts. When the reasons of the referral were analyzed according to the patient's symptoms, most of them were evaluated because of cutaneous symptoms (almost 77%), followed by articular symptoms (17.8%). After the evaluation of the patients, we found that 66 patients (58.9%) met diagnostic criteria for PsA, and 13 (11.6%) presented an inflammatory disease other than PsA.
Referral Reasons and Final Diagnosis of Patients Attended in the Multidisciplinary Care Clinic.
| n (%) | |
|---|---|
| Main referral reason | |
| Diagnostic | 61 (50%) |
| Treatment | 61 (50%) |
| Referral reason by symptoms | |
| Arthralgia | 12 (10.7%) |
| Arthritis | 8 (7.1%) |
| Dactylitis | 2 (1.8%) |
| Axial symptoms | 1 (0.9%) |
| Cutaneous psoriasis | 41 (36.6%) |
| Nail psoriasis | 3 (2.7%) |
| Cutaneous problem | 45 (40.2%) |
| Final diagnosis | |
| PsA | 66 (58.9%) |
| Inflammatory disease other than PsA | 13 (11.6%) |
| Degenerative arthritis | 5 (4.5%) |
| Cutaneous psoriasis | 15 (13.4%) |
| Other articular diseases | 1 (0.9%) |
| Other cutaneous diseases | 12 (10.7%) |
Abbreviation: PsA, psoriatic arthritis.
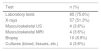
During the study period (see Table 3), the following tests were ordered: laboratory tests in a total of 85 patients (75.6%), X-rays in 57 patients (51.3%), musculoskeletal US in 4 (3.6%), musculoskeletal MRI in another 4 patients (3.6%), biopsies in 10 (8.9%) and cultures (blood, tissues, etc.) in 4 (3.6%) patients.
Patients With Laboratory Tests, Imaging Techniques and Others Required in the Multidisciplinary Care Clinic During the study Period.a
| Test | n (%) |
|---|---|
| Laboratory tests | 85 (75.6%) |
| X-rays | 57 (51.3%) |
| Musculoskeletal US | 4 (3.6%) |
| Musculoskeletal MRI | 4 (3.6%) |
| Biopsy | 10 (8.9%) |
| Cultures (blood, tissues, etc.) | 4 (3.6%) |
Following, after the evaluation of patients, the number of patients with different treatments increased (see Table 4). In the case of topical therapy from 44.6% to 88.4%, the DMARDs from 44% to 54% and biologic treatments from 17% to 29%. The number of patients with systemic steroids slightly increased, from 28.6% to 29.5%. We found that 42% of patients changed their systemic treatment, 33 patients (29.5%) a molecule change and 12 patients (10.7%) a dose change. Only 2 patients stopped their therapy.
Treatment Changes in the Multidisciplinary Care Clinic.a
| Treatment | Prior | After visit |
|---|---|---|
| Topical therapy | 51 (44.6%) | 99 (88.4%) |
| Ultraviolet phototherapy | 1 (0.9%) | 1 (0.9%) |
| NSAID | 74 (68.7%) | 83 (74.1%) |
| Systemic steroids | 31 (28.6%) | 33 (29.5%) |
| DMARD | ||
| Methotrexate | 34 (30.4%) | 44 (39.3%) |
| Leflunomide | 9 (8%) | 9 (8%) |
| Cyclosporine | – | 1 (0.9%) |
| Sulfasalazine | 4 (3.6%) | 3 (2.7%) |
| Others | 4 (3.6%) | 3 (2.7%) |
| Biologic therapy | ||
| Etanercept | 7 (6.2%) | 9 (8%) |
| Adalimumab | 5 (4.5%) | 13 (11.6%) |
| Infliximab | 4 (3.6%) | 4 (3.6%) |
| Golimumab | 1 (0.9%) | 3 (2.7%) |
| Ustekinumab | 1 (0.9%) | 2 (1.8%) |
| Others | 1 (0.9%) | 1 (0.9%) |
| Changes in topic treatments | ||
| Without changes | 50 (44.6%) | |
| Molecule change | 59 (52.7%) | |
| Doses change | 2 (1.8%) | |
| Treatment cessation | 1 (0.9%) | |
| Changes in systemic treatments | ||
| Without changes | 65 (58.0%) | |
| Molecule change | 33 (29.5%) | |
| Doses change | 12 (10.7%) | |
| Treatment cessation | 2 (1.8%) | |
Abbreviations: NSAID, non-steroidal anti-inflammatory drugs; DMARD, disease modifying antirheumatic drugs.
Finally, all but 10 patients answered the satisfaction survey (92% response rate). The level of satisfaction was in general very high (Table 5).
Satisfaction Questionnaire Results.a
| Question | Result |
|---|---|
| Qualify from 10 (excellent) to 0 (very bad) the general attention in the multidisciplinary care unitb | 9±1.2 |
| Describe the care of the multidisciplinary unit compared with your usual care | |
| Much better | 52 (46.8%) |
| Better | 51 (45.9%) |
| The same | 8 (7.2%) |
| Worse | 0 (0%) |
| Much worse | 0 (0%) |
| Quality of the information given in the multidisciplinary care unit | |
| Very good | 58 (52.2%) |
| Good | 48 (43.2%) |
| Normal | 4 (3.6%) |
| Bad | 1 (0.9%) |
| Very bad | 0 (0%) |
| ¿Was your disease better controlled in this multidisciplinary care unit? YES | 112 (100%) |
The care of the multidisciplinary unit compared with your their care was considered much better of better for 103 patients (almost 93% of the study sample). The same way, the quality of the information given in the multidisciplinary care unit was good or very good for 106 patients (95.4%). All of patients considered that their disease was better controlled in this multidisciplinary care unit.
DiscussionWe have shown the experience of a multidisciplinary care unit for patients with psoriasis or PsA. The main objectives of this unit are to facilitate an early diagnosis of PsA, improve management of patients with psoriasis and PsA, and increase cooperation between the rheumatology and dermatology departments. Referred patients are attended (at the same by a dermatologist and a rheumatologist) in a few days (maximum 1 month), are carefully evaluated including the assessment of comorbidities and the treatment is agreed by the specialists following national and international guidelines.
One of the positive contributions and target of this unit is an early diagnosis of PsA. This is especially relevant since a diagnostic delay of more than 6 months might contribute to poor radiographic and functional outcome in PsA patients.10 According to our data, an important rate of patients eventually met PsA criteria. Although we cannot demonstrate this, it is possible that since the unit was set up dermatologist feel more comfortable and referral patients earlier with any kind of diagnostic doubts. In fact, it has been shown that traditional care, where patients are attended by rheumatologists and dermatologist independently, might lead to diagnosis delay.9,10 In the literature other multidisciplinary care units have shown their ability to make at least an earlier diagnosis in these patients, and have shown that there were many discrepancies with the previous diagnosis.14–16 Moreover, like in our cohort, this multidisciplinary approach facilitate a differential diagnosis for cutaneous and joint problems as well.14,15
The same way, we also expected changes in the patient's treatments. Around half of patients changed their topic or systemic treatment (molecule or dose). We could not demonstrate neither that all of these changes improved patients outcomes and prognosis, but we would like to highlight that we increased the percentage of topic and systemic drugs, probably optimizing the previous ones. Only the rate of patients on corticosteroids slightly increased after the multidisciplinary evaluation. The same results have been described in other multidisciplinary care units.14–16 Another positive point of these multidisciplinary care units is the sharing decision making between two specialists with different but complementary visions. This way, discrepancies between specialists that can led to medical errors or compliance problems, for example, could be avoided.17,18
On the other hand, we would like to point out that apart from labs and X-ray, just a few of patients required MRI or biopsies probably reflecting that clinical evaluation made by the experts in psoriasis and PsA (who follow national and international guidelines) solved most of the referred problems.
Regarding to comorbidity, we have exposed that more than a half of patients evaluated in the unit presented comorbidities. Patients with psoriasis and PsA show a high prevalence of comorbidities and risk factors, among which the most important are cardiovascular disease and metabolic syndrome.19–21 Other frequent comorbidities are hyperuricemia and gout.22 We found the same results in our patients. An adequate management of comorbidities is of great importance for the specialists, as comorbidity influences diagnosis, prognosis, and treatment decisions, and has a great impact on health care resources.23–26 Therefore, in a multidisciplinary care approach, a proper evaluation and management of comorbidities could be facilitated in order to improve outcomes in complex patients.
One of the main outcomes of our study is the great level of satisfaction in our patients. In their opinion, for most of patients this multidisciplinary unit compared with their usual care was better or much better. Interestingly, all of them considered that the disease was better controlled in this multidisciplinary care unit. Data from a case series of patients with psoriasis and PsA followed following a multidisciplinary care model was also very high.14 This is very important because in chronic diseases the adherence and compliance with treatments and visits is vital and is very influenced with the overall level of satisfaction of patients with the care they receive.27
Following, this study has some limitations. First, we have no control group. Ideally our results should have been compared with traditional care. However, the rate of diagnosis confirmation and treatment changes suggest that, to some extent, we are making earlier diagnosis of PsA and probably optimizing patient's treatments. On the other hand, we did not used a generic or specific questionnaire to assess patient's satisfaction and this was retrospectively evaluated. But taking into account the very high level of satisfaction reported we are confident that this multidisciplinary care unit really meant a good option for patients with psoriasis or PsA.
In summary, collaboration between expert rheumatologists and dermatologists in a multidisciplinary care unit facilitates a proper and overall evaluation of the skin and musculoskeletal burden, subsequently leading to an earlier diagnosis of PsA, comorbidities and risk factors and to a more comprehensive treatment approach. As a consequence the disease outcomes could improve as well as patient's satisfaction.
Ethical DisclosuresProtection of human and animal subjectsThe authors state that for this investigation the procedures followed conformed to the ethical standards of the responsible human experimentation committee (Hospital Can Misses, Ibiza), and in agreement with the World Medical Association and the Declaration of Helsinki.
Confidentiality of dataThe authors declare that the confidentiality of the data has been guaranteed.
Right to privacy and informed consentThe authors state that the patient's informed consent was requested.
FundingThis manuscript was developed by an unrestricted grant from Pfizer.
Conflict of InterestDr. Loza reports grants from Pfizer, during the conduct of the study; grants from Pfizer, grants from Abbvie, grants from Roche, grants from MSD, grants from BMS, grants from Novartis, grants from UCB, outside the submitted work. The rest of authors refer no conflicts of interest.