In the year 2006 the Hospital Complex of Jaén began a new model of attention for consultation of knee osteoarthritis (CMAR), to offer quality treatment to the patient based on clinical practice guidelines. The objective of this study was to analyze the efficiency of the unit, in terms of delaying the time until a knee prostheses is needed.
Patients and methodsAn analysis of a retrospective cohort of patients seen at the CMAR was made, with a minimum available data set, and a Kaplan–Meier analysis carried out in order to evaluate the time until the referral of the patient to surgery, as well as a Cox regression analysis in order to study the factors related with the time until the referral.
Results224 patients were included, with mean age of 65.7 years (95% CI 64–67), 67.9% women. 48.2% had a stage III affection (Kellgren–Lawrence), 27.5% stage 2, 15.3% stage 4, and 9% stage 1. 90.2% (202) received treatment with viscosupplementation (Hialuronic acid NASHA). Single joint affection (P<.0001; OR 0.267, 95% CI 0.130–0.549), a higher degree of osteoarthritis (P=.048; OR 0.410, 95% CI 0.169–0.992), and lower intensity of pain (P<.0001; OR 1.091, 95% CI 1.044–1.141) were the factors related with shorter time until surgery. Treatment with viscosupplementation increased the time until surgery in all patients.
ConclusionsFactors like a lower age of the patient and the involvement of a single joint influenced the referral of the patient to surgery. The administration of viscosupplementation delayed the time until the patient was finally referred to surgery.
En el año 2006 se inició en el Complejo Hospitalario de Jaén un nuevo modelo de consulta monográfica de artrosis de rodilla (CMAR), para ofrecer al paciente un tratamiento de calidad basado en las guías de práctica clínica. El objetivo de este estudio fue analizar el rendimiento de la unidad, en términos de prolongación del tiempo hasta la necesidad de cirugía protésica de rodilla.
Pacientes y métodosSe realizó el análisis de una cohorte retrospectiva de pacientes atendidos en la CMAR y que dispusieran de un conjunto mínimo de datos. Se realizaron un análisis de Kaplan–Meier para evaluar el tiempo hasta la derivación del paciente a cirugía y un análisis de regresión de Cox para estudiar los factores relacionados con el tiempo hasta la derivación.
ResultadosParticiparon 224 pacientes con una edad media de 65,7 años (IC del 95%, 64 a 67), el 67,9% eran mujeres. El 48,2% tenía una afectación de grado 3 (Kellgren–Lawrence), un 27,5% de grado 2, un 15,3% de grado 4, y un 9% de grado 1. El 90,2% (202) recibió tratamiento con viscosuplementación (ácido hialurónico NASHA). La afectación de una sola articulación (p<0,0001; OR=0,267, IC del 95%, 0,130 a 0,549), la mayor gravedad de la artrosis (p=0,048; OR=0,410, IC del 95%, 0,169 a 0,992) y la menor intensidad del dolor (p<0,0001; OR=1,091, IC del 95%, 1,044 a 1,141) fueron los factores relacionados con menor tiempo hasta la cirugía. El tratamiento con viscosuplementación aumentó el tiempo hasta la cirugía en todos los pacientes.
ConclusionesFactores como la menor edad del paciente y la afectación de una sola articulación influyeron en la decisión de derivación del paciente para cirugía. La administración de viscosuplementación prolongó el tiempo hasta que el paciente fue finalmente derivado a cirugía.
Since 2006 the specialty clinic of knee osteoarthritis (SCKO) has functioned, attached to the section of Rheumatology of the Hospital of Jaén.1 The objective of the creation of the unit was to provide quality care, reduce the high costs associated with the use of inadequate diagnostic and therapeutic tests, and optimize available resources. After a period of five years it was decided that the time was right for the evaluation of the results, which were analyzed from three points of view: the effectiveness in controlling the symptoms of the patients, the delay with which patients should be operated for joint replacement facilitated by adequate control of symptoms by the SCKO unit and, finally, the economic benefits of our intervention.
Clinical practice guidelines accept several treatment options that aim to control the symptoms of knee osteoarthritis (OA-R).2–4 Among these treatments one can find viscosupplementation with intraarticular injections of hyaluronic acid, which in addition to relieving pain leads to a delay in the need for knee prosthesis. In a second stage, the patient may be referred for prosthetic knee surgery.
The monitoring and treatment protocol of the SCKO follow the recommendations of the Spanish Society of Rheumatology2 and international recommendations, as published.3,4
During clinical practice we observed that patients treated in the SCKO unit achieved a greater reduction in pain, the longer the patient with knee arthritis (KA) remained in the unit. Empirically viscosupplementation helped control the symptoms, as patients who were not treated with viscosupplementation not only did not improve, but also worsened. For this reason, viscosupplementation was considered as a factor that should be studied, along with others, as something that could influence the final decision to refer patients for knee replacement surgery in our unit. Because viscosupplementation was not widely administered to all patients until the analysis for this study, there were two differentiated groups of patients available, those who received treatment or those who did not. It became necessary to know the value of viscosupplementation in delaying surgery and the advantages or disadvantages of its administration in economic terms, the subject of future communications.
Patients and MethodsStudy Design and Ethical StandardsWe conducted a retrospective cohort study of patients seen by the SCKO unit, attached to the section of Rheumatology of the Hospital of Jaén. Data were obtained from electronic medical records, which collected homogeneous clinical parameters in all patients being followed. A specialist in rheumatology was trained to complete the survey and entered data into a workbook designed for electronic data collection regarding the study, which had a verification system. Data entered into the database were validated against the source data from the medical records. Patients selected to complete the study had to meet the selection criteria listed below. Included in the analysis were all cases in the database. The ethical review was requested from the Clinical Research Committee of the Hospital of Jaén study and the classification of the study from the Spanish Drug Agency, which called it a postmarketing study with other designs (EPA-OD), directed at gathering information on drugs or medical devices from the survey data. Due to the retrospective and anonymous nature of the study, no consent was obtained from patients in order to include their data in the analysis.
Criteria for the Selection of PatientsThe criteria for selecting patients for the study were: (1) referral to the SCKO; (2) diagnosis of RA was done according to the clinical protocol based on the Consensus recommendations of the Spanish Society of Rheumatology2; (3) no other osteoarthritis mechanical problems in different joints: torsion of cartilage, ligaments affected due to trauma, severe varus or valgus deformity, terminal bone–bone disease; (4) inclusion in the study once for the involvement of the joints; (5) availability of a minimum set of data: age, sex, severity of RA (Kellgren–Lawrence), date of first visit, date of entry into the waiting list for prosthesis, date of prosthetic intervention, last known state of the patient, date of replacement of the prosthesis; (6) the patient should not have had any contraindication to the use of viscosupplementation (hyaluronic acid, NASHA: DUROLANE®) during the follow-up period in the SCKO; (7) viscosupplementation therapy in patients who received it was always with the same product: NASHA hyaluronic acid, DUROLANE®; and (8) the minimum period of follow-up in patients at the SCKO should have been at least one year.
Criteria for Patient Referral due to Knee ProsthesisCriteria for referral of the patient to Trauma for knee prosthesis surgery were homogeneous for all cases: (1) patients with radiographic knee arthritis grade IV, except those that due to disease or treatment were contraindicated concomitant surgery, and patients older than 75 years of age, or (2) patients with knee osteoarthritis radiographic grade III and who had disabling conditions or disease refractory to standard medical treatment (analgesics, NSAIDs, steroid injections or disease modifying drugs for OA e) provided that they were 60 years of age or older.
Sociodemographic and Clinical VariablesWe collected demographic and relevant clinical data that could influence the status and prognosis of the patient as potential comfounders or effect modifiers, and data on the affected joint as potential predictors. We registered the origin of the case as being either from primary care or the trauma consultation, as well as the birth date, gender, physical activity (work, sports or non-working if the patient was unemployed), the presence of some other disease and its relationship with patient outcome or response to treatment of joint pain and medications received for the treatment of these diseases. Regarding clinical data, we recorded the date on which the patient was included in the SCKO unit for monitoring, the date of onset of symptoms of knee OA, the affected joint (left, right or both), the location of the injury (patellofemoral or femorotibial), the presence or absence of traumatic injury of the joint, the date of completion of the last arthroscopy, the presence of other local condition of the joint and the classification of osteoarthritis upon inclusion into the SCKO clinic, as well as the severity criteria of Kellgren–Lawrence (grade 0–4, from lowest to highest radiographic severity). Pain intensity was recorded at the time of incorporation into the SCKO and the last follow-up visit through a visual analog scale (VAS) measuring pain intensity on a scale of 0–100mm, where the value 0 means the absence of pain and the value 100 the worst pain imaginable. We registered the treatment that patients had received before entering the SCKO clinic and the general data of the treatments given to the patient as well as its follow-up until the most recent visit. We collected the patient's condition in his last follow-up visit with regard to vital status, if lost to follow-up, or if derived for knee replacement surgery, and the date on which these events occurred. We also collected the date of entry into the waiting list for prosthesis and the date of the intervention. Clinical data were collected from patients in the final state, in relation to radiographic severity of osteoarthritis (Kellgren–Lawrence criteria), pain intensity measured with a VAS and treatments and recommendations that the patient received at the time. We recorded whether the patient was referred from the SCKO unit for follow up to primary care or trauma if not referred to the waiting list for knee replacement.
Statistical AnalysisDescriptive analysis was performed with the results for qualitative variables described as frequencies and percentages. Comparisons between such variables were performed using Fisher's exact test or χ2 test as appropriate. Quantitative variables were analyzed descriptively, obtaining as a result the average, the 95% confidence interval and the mean and median. Comparisons in these variables were performed using Student's t test or by analysis of variance (ANOVA) when comparing various categories.
Due to the very low proportion of missing data, less than 1% in most of the variables collected, an analysis of the application of residuals or data imputation techniques was not considered applicable.
Homogeneity tests were applied to patients upon entry into the SCKO unit for variables that may influence the time until patient referral for knee replacement surgery, for control of potential patient selection bias. We compared the proportions of patients regarding sociodemographic, clinical data and treatment received, by gender, the origin of the case (primary care or trauma), and depending on whether or not the patient received treatment with viscosupplementation during follow up.
In the analysis of time to prosthesis surgery was applied to an analysis of Kaplan–Meier, where time tracking is the time from follow up at the SCKO unit to referral of the patient to surgery for knee prosthesis, or until the last visit at the SCKO, if the patient was not referred to surgery. The main event in the survival analysis was the patient's referral for knee replacement surgery. We applied a multiple regression analysis of Cox to study the variables that may influence the time until the patient's prosthetic surgery. Due to the retrospective nature of the study, multivariate Cox regression was exploratory and should not be interpreted as predictive. Factors analyzed as potential confounders or effect-modifying variables were: patient age at admission to the SCKO, the gender of the patient, the presence of comorbidity, number of joints affected, the severity of involvement of the joint, duration of joint involvement, pain intensity on admission and receiving viscosupplementation treatment during follow up.
Comparison of survival curves was performed using the log rank test (Mantel–Cox). The significance level was set at 0.05. We used SPSS 14.0.
ResultsHomogeneity of the Entry into the Knee Osteoarthritis Clinic and Bias ControlNo differences in demographic data were seen by gender, the origin of the case (primary care or trauma), or depending on whether the patient received viscosupplementation during follow up at the unit.
There were statistically significant differences (P=.005) in the time evolution of joint pain according to patient gender, being significantly higher in women, 5.7 years (95%, 5, 3, 6.2) and 47 years in men (95%, 4, 1–5.2).The mean difference was 1.1 years (95% CI, 0.3–1.9).
Patients receiving viscosupplementation during follow up were classified, in a higher proportion (51.5%), in grade 3 joint involvement according to the Kellgren–Lawrence scale than patients who did not receive viscosupplementation (18.2%), P<.0001.The proportion of patients classified as level 1 of joint involvement was significantly higher (P<.0001) in patients not receiving viscosupplementation during follow-up (36.4%) than those who received this treatment (6%).
No differences by gender or treated with or without viscosupplementation group were seen regarding the proportion of patients who were treated with postural measures (100%), analgesics and/or NSAIDs (100%), SYSADOA (1.8%), arthrocentesis (1.8%), pre-entry viscosupplementation (0.9%), or the proportion of patients referred to primary care (97.3%) or trauma (2.7%).
No significant difference in the proportion of patients in the final stage of function were seen according to whether they did or did not receive viscosupplementation during follow up (P=.258).
General and Sociodemographic DataPatients included in the study began their follow up in the SCKO unit between 5 April 2006 and 29 April 2009. The percentage of missing data was less than 1% for most of the variables studied.
We included 224 patients whose demographic data are shown in Table 1. The mean age of the patients was 65.7 years (95% CI, 64–67) with a median of 66.1 years and a minimum age of 34 years and maximum of 89 years.
Sociodemographic and Clinical Data of Patients Included in the Study.
| No. | % | |
| Sex | ||
| Male | 72 | 32.1 |
| Female | 152 | 67.9 |
| Physical activity | ||
| Not work related | 173 | 77.2 |
| Work related | 51 | 22.8 |
| Sports | 0 | 0 |
| Personal history of disease | ||
| No | 12 | 5.4 |
| Yes | 207 | 92.4 |
| Unrecoverable data | 5 | 2.2 |
| Origin of the patient | ||
| Primary care | 132 | 61.7 |
| Traumatology | 82 | 38.3 |
| Clinical data | ||
| Affected joint | ||
| Right knee | 50 | 22.3 |
| Left knee | 56 | 25.0 |
| Both knees | 118 | 52.7 |
| Lesion location | ||
| Patellofemoral | 0 | 0 |
| Femorotibial | 223 | 100 |
| History of trauma to the joint | ||
| No | 219 | 98.2 |
| Yes | 4 | 1.8 |
| Arthroscopy performed | ||
| No | 217 | 97.7 |
| Yes | 5 | 2.3 |
| Another local joint disease | ||
| No | 221 | 100 |
| Yes | 0 | 0 |
| Classification of osteoarthritis joining the SCKO: Kellgren–Lawrence scale | ||
| Grade 0 | 0 | 0 |
| Grade 1 | 20 | 9.0 |
| Grade 2 | 6 | 27.5 |
| Grade 3 | 107 | 48.2 |
| Grade 4 | Pollution 34 | 15.3 |
90.2% of patients (202 cases) were treated with viscosupplementation (hyaluronic acid, NASHA: DUROLANE®) at some point of SCKO follow up, and 9.8% did not receive this treatment (22 cases).
84.8% (190) of patients was receiving treatment for associated medical conditions.
52.7% of patients had both knees affected and 25% of cases had only the left knee affected.
48.2% of patients were classified as grade 3 Kellgren–Lawrence, 25.5% grade 2 and 15.3% grade 4.
The mean follow-up of patients included in the study was 374 days (95% CI, 323–425), with a median of 279 days, a minimum of 0 days and a maximum of 1547.
Forty patients (17.9%) were referred for knee replacement surgery. The mean follow-up of these patients until prosthetic surgery was performed was 328 days (95% CI, 232–424), with a median of 279 days. Twenty of the 39 patients referred for surgery were operated, with a range from the date they joined the SCKO unit of 584 days (95% CI, 487–680), with a median of 596 days. The average time from patient referral to surgery was 188 days (95% CI, 119–258), with a median of 100 days, with a minimum of 27 days and maximum of 813 days. The mean time spent on the waiting list was 165 days (95% CI, 147–184), with a median of 169 days, minimum 94 days and maximum of 343 days.
9.1% (2 cases of 22) of patients who did not receive viscosupplementation were referred for surgery and 11.9% of patients receiving viscosupplementation during follow-up in the unit were referred for surgery (38 case of 202). In total, 11.6% of patients were referred for knee replacement surgery.
Time Until Referral of Patients to Knee Prosthetic SurgeryWe analyzed the length of stay of patients in the SCKO unit and the factors that influenced the final referral of patients for prosthetic surgery.
The factors examined were patient age at admission into SCKO, gender of the patient, the presence of comorbidity, number of joints affected, the severity of joint involvement, the time evolution of joint involvement, pain intensity on admission and viscosupplementation treatment during follow up.
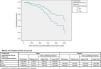
We observed a median survival of 1225 days (95% CI, 942–1507), when 50% of patients were referred to the unit for prosthetic surgery. A differentiated survival curve was observed generally for patients receiving no treatment or viscosupplementation (Fig. 1). The mean time to surgery in patients who did not receive viscosupplementation was 694 days (95% CI, 548–839) and 1093 days (95% CI, 980–1206) if they received treatment with viscosupplementation.
Because the proportion of patients in each radiologic severity group was not homogeneous among patients who received treatment with viscosupplementation compared to the non-treated, further analysis was stratified by radiographic severity of osteoarthritis to determine times until the surgery depending on whether or not they were receiving treatment.
In the stratified analysis, treatment with viscosupplementation extended time until surgery in the group of patients with grade 3 joint involvement upon joining SCKO, close to statistical significance (P=.064). The median survival of patients with grade 3 lesions and viscosupplementation was 1278 days (95%, 474–2081) and for those not receiving treatment it was 596 days (95% CI, 14–1179).
No differences in time to referral to surgery were overall associated to gender (P=.741). When performing a stratified analysis according to the severity of the joint involved and the gender of the patient, we observed that the time until surgery was significantly higher in women with grade 3 lesions who received viscosupplementation (P=.029). There were no significant differences between genders in the other degrees of joint involvement.
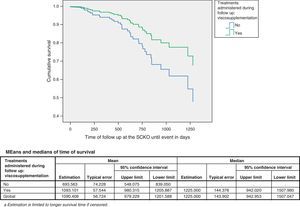
We explored whether age at admission influenced the time to patient referral for surgery and to that end we divided the patients into higher or equal to 65 and less than 65 years of age groups. There was a longer time to surgery in patients older than 65 years (P=.024), with a median survival in this group of 1278 days (95% CI, 600–1956), and, in patients younger than 65 years, of 945 days (95% CI, 769–1121). See the survival curves in Fig. 2. No differences between patients in the different strata were seen based on whether they were receiving treatment with viscosupplementation or not.
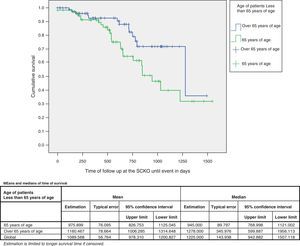
We analyzed if patients with one or both affected joints were derived earlier to surgery and found that patients with one affected joint (47.3%) were derived earlier than those with 2 joints affected (P<.0001). The median survival of patients with only one joint affected was 778 days (95% CI, 622–934), and patients with two affected joints did not reach the median survival (Fig. 3).
When performing an analysis stratified by the two previous variables, we found that the time until surgery was higher in patients with two affected joints, whether the patients were younger than 65 years (P=.002) or if they were over 65 years (P=.008).
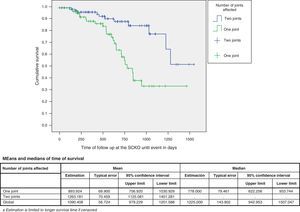
Multivariate analysis was performed using Cox regression to assess the variables related to the time before referring the patient to surgery jointly (Table 2). The gender of the patient, the presence of comorbidity, number of joints affected, the age at which the patient was admitted to the SCKO unit, the severity of joint involvement at the last follow-up visit, the time of disease progression, the intensity of pain at the last follow up visit and treatment with viscosupplementation into the equation were included. The following were statistically significant: (a) the number of affected joints (P<.0001), with less time to surgery if only one joint was affected (OR=0.267, 95% CI, 0.130–0.549), (b) the severity of osteoarthritis (P=.048), higher severity, shorter time to surgery (OR=0.410, 95%, 0.169–0.992), and (c) pain intensity measured on the visual analog scale (P<.0001), with an OR of 1.091 (95% CI, 1.044–1.141), higher pain intensity, longer time to surgery.
Factors That Influence the Time Until the Patient Undergoes Surgery.
| Sig. | Odds ratio | 95.0% CI for odds ratio | ||
| Inferior | Advanced | |||
| Gender | .859 | .933 | .432 | 2.012 |
| Comorbidity | .115 | 5.215 | .670 | 40.566 |
| Number of joints affected | .000 | .267 | .130 | .549 |
| Age at admission to the SCKO | .395 | 1.021 | .973 | 1.070 |
| Severity of OA (Kellgren–Lawrence) | .048 | .410 | .169 | .992 |
| Viscosupplementation | .376 | .511 | .116 | 2.257 |
| Duration of osteoarthritis in years | .104 | .816 | .639 | 1.043 |
| VAS score at the end of the monitoring | .000 | 1.091 | 1.044 | 1.141 |
Sig, statistical significance of the variable.
Factors included in the Cox regression analysis, exploratory factor that may be related to the time until the patient was sent for knee replacement surgery.
A value of 0 for the variable gender refers to males, 1 to females.
The odds ratio for non-significant variables is valid only on the direction of the relationship.
It is interesting to analyze the behavior of the SCKO unit in its operation. It was possible to verify whether the action protocol is followed properly and when patients are referred for prosthetic intervention. The compliance of the action protocol has been shown to have nearly 100% of the patient data on the history of their disease, its treatment, and pain evolution which supports proper operation of the unit. Unquestionably, there are individual patient factors such as the degree of functional disability and desire of each patient to return to a more active life, which influence the final decision of the surgery involved, beyond the action protocol defined by the SCKO unit. The “cost effectiveness” also intervenes in terms of patients who may eventually recover their physical activity. Thus, for example, it has been observed that patients with a single affected joint were operated before those with 2 affected joints. Thus, recovery was achieved by more patients with the same number of interventions performed than if two separate interventions were performed in patient with both joints affected.
In this sense, the decision was made to refer to surgery in less time if the patient was younger (under 65), or in a patient with longer life expectancy and, therefore, more years of an active lifestyle, free from affectation. In published studies with similar objectives we also found that patient age was a deciding factor for those who were selected for surgery and the conduct for patients with similar ages to those of our study was also comparable.6,7
Among the medical interventions that were applied to patients, we observed that viscosupplementation (NASHA hyaluronic acid: DUROLANE®) prolonged the time until patients were finally operated on up to 1.5 times (Fig. 1). Although statistical comparison between the two survival curves was not significant (P=0.064), there was a clear difference between them in favor of patients treated with viscosupplementation. Specifically, women with grade 3 joint involvement treated with viscosupplementation achieved a significant prolongation of the time to surgery (P=.029). It is possible that this difference has been observed only in women because this gender was predominant (67.9%) and patients with stage 3 lesions were more numerous (48.2%), the male group was much lower and, therefore, it is possible that the sample size for this layer did not allow us to find significant differences.
Something paradoxical observed in the multivariate analysis was the relationship between a longer follow-up of patients in the unit until they were referred for surgery and pain intensity in the last assessment. It was expected that patients with greater intensity of pain would be referred for prosthetic surgery before patients with less intensity, regardless of the other factors studied; however, we found that patients with less pain were derived before for surgery (P<.0001). Although this result was statistically significant, the magnitude of pain intensity varied only in the order of about 5 VAS points for each year of tracking. It could also explain the delay in surgery in patients with more pain through the presence of other factors that prevented the patient from being operated, something not included in the study.
Due to the retrospective nature of the study, multivariate Cox regression was exploratory and, therefore, should not be interpreted as predictive of the above findings; we should extract factors that may influence the time to surgery. In any case, the value of multivariate analysis results should always be taken into consideration over the results of univariate analysis, even if we were able to perform a stratified analysis by one or more confounding variables, as in the case of gender and severity of joint involvement.
Data from this study could be considered comparative for workgroups with action protocols that match the methods described in this study and populations with similar demographic characteristics.
In total, 11.6% of patients were referred finally for knee replacement surgery, 11.9% did receive viscosupplementation, a figure significantly lower than that observed in other studies (19%) in which surgery after administration of viscosupplementation is studied.5
Time to surgery in patients treated in our unit, 1225 days (95% CI, 942–1507), is a factor to consider in the study of the effectiveness of the unit.We also observed that the median survival to surgery in our unit was of 1093 days (95% CI, 980–1206) if patients received treatment with viscosupplementation (hyaluronic acid, NASHA: DUROLANE®), 1.7 times greater than that described in the scientific literature, and 638 days in patients treated with other types of viscosupplementation, which could be the result of closer monitoring of patients in our specialized unit.3,5,8–10
In summary, we observed that non-modifiable factors such as patient age and involvement of a single joint, influenced the decision of referring the patient to surgery for joint replacement. Viscosupplementation administration showed a tendency to prolong the time until the patient was ultimately derived for a knee prosthesis. It will be, therefore, useful to analyze the economic impact of increasing the time until patients are finally operated on and quantify the savings that could be achieved with interventions such as viscosupplementation.
Ethical ResponsibilitiesProtection of People and AnimalsThe authors declare that procedures conformed to the ethical standards of the committee responsible for human experimentation and were in accordance with the World Medical Association Declaration of Helsinki.
Data ConfidentialityThe authors declare that they have followed the protocols of their workplace on the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to Privacy and Informed ConsentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Romero Jurado M, et al. Factores que influyen sobre el tiempo hasta la necesidad de intervenir un paciente en la lista de espera para prótesis de rodilla. Reumatol Clin. 2013. http://dx.doi.org/10.1016/j.reuma.2012.09.003.