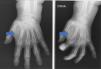
A 78-year-old woman presented with a tumour of 3 months of evolution, with progressive increase in size, on the anterior aspect of the left hand at the level of the index finger, Physical examination showed a soft, painless tumour of over 1cm in size.
Plain radiographs (Fig. 1), ultrasound (Fig. 2), and magnetic resonance imaging (Fig. 3) were requested.
A complete excision of the lesion was performed, after which the pathological anatomy revealed a giant cell tendon sheath tumour (GCTST) (Fig. 4). Currently, the patient has not had any recurrence, with mobility preserved and no complications after the intervention.
Comment/discussionGCTST is the second most common benign neoplasm at this level. It is classified into 2 types, depending on the involvement: localised, more frequent in hands; and diffuse. The mean age of presentation is 35–50 years, with a predominance in women. The most frequently affected location is the 2nd and 3rd fingers, and the extensor tendons, and it is also more frequent in the dominant hand.1–4
Clinically, it manifests as a solitary soft tissue nodule, asymptomatic, and with slow growth. The differential diagnosis is reached mainly with entities such as: ganglion, cyst, lipoma and sarcoma.5,6
The ultrasound description of the GCTST is a hypoechoic, heterogeneous lesion, with Doppler, related to the affected tendon. On MRI it presents as a lobed lesion, of intensity in T1 and T2 which, in STIR, show intense enhancement. Determination of hypointense haemosiderin foci is useful in differentiating these from other lesions.
With respect to histological characteristics, the GCTST presents mononuclear cells such as fibroblasts, epithelioid or foamy macrophages; multinucleated giant cells and inflammatory cells, on collagen stroma. On the other hand, vascularisation can be observed, with hemosiderin deposition in some cases.3,7,8
Treatment is based on the total removal of the lesion, although up to 45% recur.3
Ethical responsibilitiesProtection of people and animals. The authors state that no experiments were carried out on humans or animals for this research.
Data confidentiality. The authors state that they have followed their workplace's protocols as regards the publication of patient data.
Right to privacy and informed consent. The authors obtained informed consent from the patients or subjects referred to in the article. This document is in the possession of the corresponding author.
None.