Hemarthrosis refers to the presence of intraarticular blood and its usual presentation is acute monoarthritis, generally of the knee. The differential diagnosis of spontaneous hemarthrosis includes coagulation disorders, pigmented villonodular synovitis, vasculitis, rheumatoid arthritis and calcium pyrophosphate or hydroxyapatite crystal deposition diseases, among other causes.1
On the other hand, scurvy is a disease provoked by deficiency of vitamin C or ascorbic acid, a water-soluble vitamin involved in collagen synthesis through the hydroxylation of lysine and proline in precollagen.2 The diagnosis of scurvy is clinical and it is necessary to consider an extensive differential diagnosis with a number of diseases, especially vasculitides, as cutaneous purpura is one of its most characteristic clinical manifestations.3
We report the case of a 42-year-old man with a history of paranoid schizophrenia, who came to the emergency department with pain and progressive swelling of his left knee that had begun 2 weeks earlier. He had experienced no previous injury. Physical examination revealed gingivitis, purpuric cutaneous lesions and arthritis in his left knee.
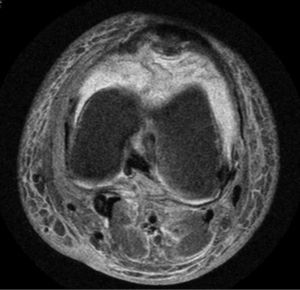
He underwent arthrocentesis had yielded a blood-stained fluid (940,000μL red blood cells, 24,550μL nucleated cells—11% lymphocytes and 89% neutrophils—and 56g/L proteins). A plain radiograph of the knee was normal and magnetic resonance imaging (MRI) revealed marked joint effusion and substantial intra-articular circumferential edematous infiltration, which was reported to be compatible with hemarthrosis, with no other pathologic findings (Fig. 1). On the other hand, a biopsy of the purpuric skin lesions showed extravasation of blood and siderophages, with no inflammatory infiltrate.
Antinuclear antibodies (ANA), antineutrophil cytoplasmic antibodies (ANCA), cultures of joint fluid, serological tests for hepatitis B or C virus and human immunodeficiency virus, as well as coagulation tests, routine analyses, and determination of acute-phase reactants were negative or normal. The medical history referred to a restrictive diet, in which the patient ate only milk and yogurt, as well as previous episodes of gingival bleeding.
The serum vitamin C levels were <0.10mg/dL (normal values: 0.4–2mg/dL).
After the diagnosis of scurvy, treatment was begun with vitamin C supplements and a supervised diet. The outcome was positive, with a rapid improvement of the skin lesions and resolution of the hemarthrosis.
At present, scurvy is a rare finding in developed countries,4 but rheumatologists should consider this possibility in the case of spontaneous hemarthrosis, especially if it is accompanied by other hemorrhagic manifestations or eating disorders, taking into account that the definitive diagnosis is usually confirmed a posteriori, as vitamin C levels are not routinely determined.
In short, scurvy is a very rare deficiency disease in western countries, although it can be observed in some psychiatric patients and alcoholics with eating disorders. With this case, we would like to remind professionals of this condition as the cause of rheumatic disease and, although not very frequent, it must be taken into account in the differential diagnosis of hemarthrosis. The key to the diagnosis is still in the physical examination and the medical history, although the usual ancillary tests are exclusively a help to rule out other processes.
Please cite this article as: Brandy-García AM, Cabezas-Rodríguez I, Caravia-Durán D, Caminal-Montero L. Hemartrosis por escorbuto. Reumatol Clin. 2017;13:364–365.