We wish to report the case of a 69-year-old woman, an ex-smoker, with no known allergies. She had been treated for plantar fasciitis secondary to a calcaneal enthesophyte 4 months earlier by her primary attending physician. She was referred to rheumatology because she had a 2-month history of what appeared to be a mechanical pain in left ankle. She had had no previous injury and had not improved with the treatment prescribed by her primary attending physician, who had begun with an nonsteroidal anti-inflammatory drug and an oral glucocorticoid. The physical examination revealed the pain in her heel and medial malleolus, with no swelling or reddening. There was no pain, swelling or functional limitations in the Achilles region.
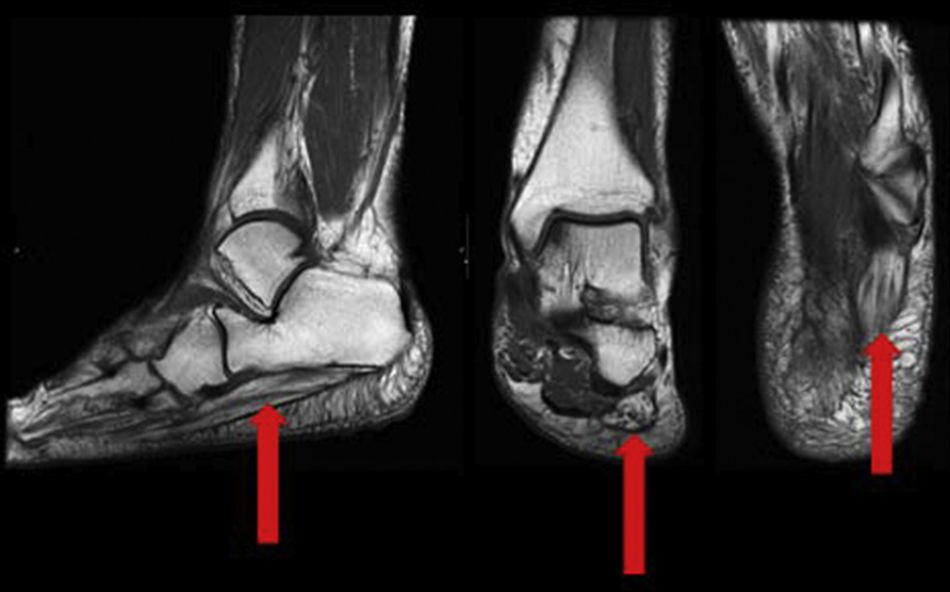
Given the suspicion of noninflammatory involvement, and with the radiograph showing the calcaneal enthesophyte, nuclear magnetic resonance showed substantial atrophy with fat replacement of the abductor muscle of the fifth toe, and several dilated or varicose veins on the inner aspect of the foot along the inferior calcaneal nerve (Fig. 1), compatible with Baxter entrapment neuropathy.
The differential diagnosis involves heel pain, so common in our clinics, which includes a wide range of diagnostic and therapeutic possibilities depending on the cause of the pain. Those of neural origin include tarsal tunnel syndrome which, although is not very frequent, it should always be considered in the differential diagnosis of the person with a painful ankle.1 To understand this syndrome it is necessary to be familiar with our anatomy.2 The posterior tibial nerve has 3 terminal branches: the medial calcaneal nerve, the medial plantar nerve and the lateral plantar nerve.1 The latter is the origin of the so-called Baxter nerve, which innervates the lumbrical muscles, the abductor halluces and the abductor of the fifth toe.
Entrapment of the first branch of the lateral plantar nerve, known as Baxter neuropathy, is the cause of 20% of cases of persistent hindfoot pain.3 It is often difficult to distinguish it from that produced by plantar fasciitis or calcaneal enthesophyte.4,5 The diagnosis is normally based on clinical findings, like the presence of paresthesias or tingling in the medial portion of the foot or the perception of pain while pressuring the course of the nerve.6,7
Thus, a detailed medical history and thorough examination are essential to differentiate Baxter neuropathy from other conditions that affect the heel. With regard to imaging studies, nuclear magnetic resonance is the technique of choice.8 It shows the isolated atrophy of the abductor digiti minimi muscle as a sign of chronic entrapment of the lateral plantar nerve, suggesting the diagnosis of Baxter neuropathy.
Entrapment can be due to biomechanical disorders, such as high arches or flat feet as well as to direct compression, such as plantar fasciitis, masses and/or calcaneal osteophytes.8 Treatment includes conservative therapy and surgical management of the cause if the latter is not effective.
Discomfort produced by peripheral nerve entrapment is common in our clinic. Baxter neuropathy is the entrapment of the first branch of the lateral plantar nerve (Baxter nerve), often difficult to distinguish from that produced by plantar fasciitis. Thus, the management of this disorder requires knowledge of anatomy and of the clinical signs.
Please cite this article as: Moreno García MS, del Río-Martínez PS, Yanguas Barea N, Baltanás Rubio P. Dolor en retropié: neuropatía de Baxter, a propósito de un caso. Reumatol Clin. 2017;13:123.