Immunosuppression is a known risk factor for cervical cancer. Women with rheumatic conditions are immunosuppressed due to the disease and the treatments. One of the main risk factors for this neoplasm is the lack of adherence to early detection programmes for human papillomavirus. The objectives of this study were to evaluate the adherence to the screening programme of patients in the Rheumatology Clinic, as well as to evaluate the prevalence of cervical lesions and their association with the different disease characteristics and the treatments received.
MethodsA descriptive retrospective study. The electronic medical history of patients actively being followed up in a tertiary hospital with rheumatoid arthritis (RA), psoriatic arthritis (PSA) and systemic lupus erythematosus (SLE) were reviewed.
ResultsFinally, 307 patients were included. No data were found for screening programme attendance in up to 42.4% of the patients (39.6% in RA, 43.8% in PSA and 46% in SLE). Among the patients who attended the screening programme at least once (57.6%), the prevalence of cervical dysplasia was 5.1%. No cases of neoplasia were found. In the simple logistic regression analysis, there was no association between attending the screening programme and any variable. The study also showed no association between the variables collected and the presence of infection and dysplasia.
ConclusionThese results are influenced by the absence of screening data in a significant percentage of patients and by the low prevalence of dysplasia found in this series of patients with rheumatic diseases.
Las pacientes con enfermedades reumatológicas presentan un estado de inmunosupresión por la enfermedad de base y los tratamientos utilizados, lo cual es un factor de riesgo para desarrollar neoplasia de cérvix uterino. Uno de los principales factores de riesgo consiste en no acudir al programa de detección precoz del virus del papiloma humano. Los objetivos de este trabajo fueron evaluar la adherencia al programa de cribado de pacientes seguidas en consultas externas de reumatología, así como estudiar la prevalencia de lesiones cervicales y su asociación con distintos aspectos de la enfermedad y los tratamientos recibidos.
Material y métodosEstudio retrospectivo en el que se revisaron las historias clínicas electrónicas de pacientes con seguimiento activo en un hospital terciario con artritis reumatoide (AR), artritis psoriásica (APS) y lupus eritematoso sistémico (LES).
ResultadosSe incluyó 307 pacientes. No se hallaron datos de asistencia al cribado en 42,4% (39,6% en AR, 43,8% en APS y 46% en LES). Entre las pacientes que asistieron al menos una vez (57,6%), la prevalencia de displasia de cérvix fue del 5,1%. No se encontró ningún caso de neoplasia. En el análisis de regresión logística simple no se encontró asociación entre las variables recogidas y la presencia de infección y displasia.
ConclusiónEs remarcable la ausencia de datos de asistencia al cribado de cáncer de cérvix en un porcentaje considerable de las pacientes con enfermedades reumáticas, lo cual dificulta el estudio del papel de la enfermedad y su tratamiento.
The Human Papilloma Virus (HPV) is greatly relevant in the appearance of precursor lesions and the development of cervical cancer.1 There are over 80 genotypes of HPV, of which 25 affect the female genital tract and, in keeping with their oncogenic potential, they are classified into high risk (genotypes 16,18,45,56) or low risk (6,11,40,42,43,44), with HPV 16 and HPV 18 being those involved in approximately 80% of cancer cases.1,2 The most determining factor for the development of cervical cancer is the persistence of infection by HPV.3 Some clinical observations indicate the importance of an appropriate functioning of the immune system for the elimination of infection by HPV. Different cytokines, including the-β transformation growth factor, the -α tumour necrosis factor, interleukine 1 and interferons may contribute to the control of HPV-associated infections and diseases, and support the significant role of T lymphocytes in controlling HPV infection.4 Other associated risk factors for this type of cancer are tobacco, a high number of sexual partners, low socio-educational level, co-infections, immunosuppression and in particular, not attending screening programmes with cytology or molecular biological tests.3,5
Screening through cytology, HPC test (in situ hybridisation, PCR and virus messenger RNA detection methods) or the combination of both (HPV cotest), leads to early diagnosis and treatment of pre-malignant lesions and impedes progression to invasive carcinoma.6 In recent years, screening has been carried out opportunistically using cytology every 3 or every 5 years, depending on the autonomous community, with a moderate coverage.7 Recently the Ministry of Health has introduced changes into national screening programmes. These programme changes were established in July 2019 and consisted in three-yearly cytology for women aged between 25–34 and high risk HPV detection test (HR-HPV) in women aged between 35 and 65. If the HR-HPV test is negative, it will be repeated after 5 years, whilst if it is positive, the patient is referred for a cytology appointment. If cytology tests negative, the HR-HPV test will be repeated one year later.8
As previously mentioned, immunosuppression is a well-known risk factor for the development of different types of cancer associated with the virus, including cervical neoplasia, as has been reported in patients with chronic kidney disease, those on dialysis and those with transplants.9,10 On consideration of this possible increase in the risk of infection, precursor lesions and invasive cancer, screening strategies appear in the guidelines for immunodeficient patients, recommending annual cytology screening from 21 to 30 years of age and a three-yearly HPV cotest from 30 to 65 years of age.7 The same could occur in patients with rheumatologic diseases and immunosuppressant treatments, who could present with a lower rate of HPV elimination and an increased risk of precursor lesions and cervical malignancies.11 The studies conducted in patients with rheumatologic diseases being treated with immunosuppressants provide contradictory results with regard to the relative risk of suffering form dysplasia, atypia and cervical cancer, depending on the baseline disease or treatments used.12–14 No specific screening recommendations exist for patients with rheumatic diseases and immunosuppressant treatment.
The main aim of this study was to evaluate whether patients with rheumatic diseases and immunosuppressant treatments with follow-up in rheumatology outpatient units fulfilled the screened recommendations of cervical cancer screening for immunodeficient patients. A secondary aim was to study the prevalence of cervical lesions and their associations with the disease characteristics or immunosuppressant treatments received.
Material and methodsAn observational, retrospective and analytical study was conducted, using the electronic medical records of all women with RA, PsA and SLE who were regularly followed up in outpatient rheumatology units from the Health Department of the General University Hospital of Alicante. Inclusion criteria were being aged 18 or above, and being actively followed up in the rheumatology outpatients’ unit. Exclusion criteria were concomittant immunosuppressant disease; having received immunosuppressant treatment for a cause other than RA, SLE or PsA; a personal background of a different neoplasia; hysterectomy prior to diagnosis of RA, SLE or PsA. The diagnosis of SLE was accepted by clinical criteria; diagnosis of PsA by the CASPAR criteria and diagnoses of RA by the ACR/EULAR 2010 criteria.
The following clinical variables were collected: age, years of follow-up and treatment. In RA and PsA duration of treatment with disease-modifying anti-rheumatic drugs (DMARDS) and with biologics was recorded; in SLE the duration of treatment with oral or intravenous glucocorticoids, non biologic immunosuppressants and combination of cyclophosphamide and biologics (not necessary together) was recorded. Time of exposure to the drug with the greatest immunosuppressant was recorded: in RA and PsA this was the time of exposure to biologic treatments and in SLE the time of exposure to any immunosuppressant (from lesser to greater level of immunosuppression: oral or intravenous glucocorticoids and non biologics, biologic drugs and combined cyclophosphamide with biologics). In PsA structural change variables were recorded, together with axial involvement and a personal background of psoriasis. Furthermore, in SLE the presence of kidney involvement was reviewed, chronic kidney disease and central nervous system inflammatory involvement as markers of a higher state of immunosuppression.
Regarding cervical pathology associated risk factors, data was collected on tobacco habit, stable sexual partner and screening. Regarding screening methods when this study was conducted, the regional programme only instigated opportunistic cytology. However, data was actively sought on HPC molecular biology in each patient if applicable, recording whether the result was positive for any of the high risk genotypes (genotypes 16, 18, 45, 56). A diagnosis of dysplasia was at times recorded (degree of the same and treatment received at the time) and a diagnosis of cervical cancer on some occasions (together with immunosuppressant treatment at the time).
Demographic variables, those relating to the baseline disease and to treatment were extracted onto the electronic medical file platform Abucasis. The results from the cytology/molecular biology were sought from the results of each patient within the electronic platform Orion (both digital platforms are those used by the public health systems of the Community of Valencia).
Descriptive statistical analysis was made in which the quantitative variables were presented in the form of means and standard deviations and the qualitative data in the form of frequencies and percentages. The main qualitative variable was the frequency of carrying out the cervical pathology screening, for which the confidence incidence (CI) was estimated at 95%. In each disease subgroup secondary analysis was performed using simple logistic regression to study whether any of the secondary variables collected were associated with greater adherence to the screening programmes or to presenting with infection and/or dysplasia. The significance level was established at P < .05. The study was approved by the ethics committee of the General University Hospital of Alicante with number 2017-568.
ResultsFinally, 307 patients were included (144 in the RA group, 89 in the PsA group and 74 in the SLE group). Mean age was 50.7 years (SD 12.8), with mean follow-up of 9.8 years (SD 8.2), and a mean exposure to the drug with the highest immunosuppressant potential of 5. 5 years (SD 5.1). It was not possible to find data on the tobacco habit in 160 revised medical files (52.1%), whilst 57 patients were smokers (18.6%). Neither was any data found for the “stable partner” variable in any of the 307 medical files. Regarding adherence to screening test, data of screening was found for 177 patients (57.7%), whilst 130 women (42.3%) had never had any, 49 (15.9%) had had one once and 128 (41.7%) had had one on two or more occasions. Also, in 61 patients (19.9% of the total) there were data on HPV which was positive for high risk genotypes in 12 patients (19.7%).
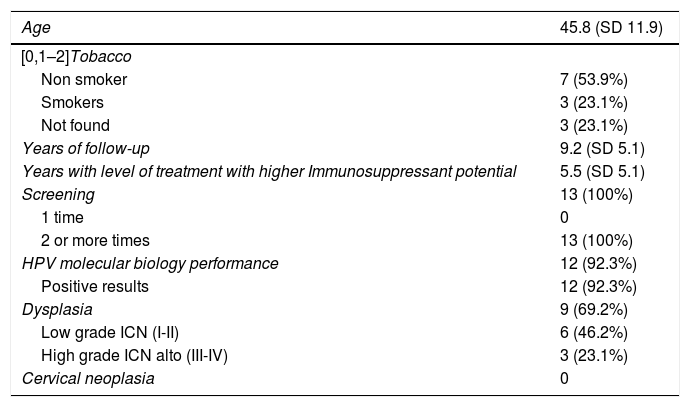
In total, cervical lesions and/or a positive result in the HPV test was found in 13 patients; all had received immunosuppressant treatment. The risk factors of this subgroup are shown in Table 1. All the patients had had screening tests on two or more occasions. Of them, 12 had done an HPV test which was positive. In the clinical file of the remaining case there was no record of a positive HPV test but there were reports of altered cytology. Only 9 patients (5.1% of those who had done at least one test; 2.9% of the total sample) developed some type of dysplasia: 5 from the RA group; 3 from the SLE group and 1 from the PsA group; in 6 cases this was low grade and in 3 high grades. None of the patient presented with cervical neoplasia (Table 1).
Positive results of screening (n = 13). The levels are expressed in absolutes and percentages, or as means and standard deviation.
| Age | 45.8 (SD 11.9) |
|---|---|
| [0,1–2]Tobacco | |
| Non smoker | 7 (53.9%) |
| Smokers | 3 (23.1%) |
| Not found | 3 (23.1%) |
| Years of follow-up | 9.2 (SD 5.1) |
| Years with level of treatment with higher Immunosuppressant potential | 5.5 (SD 5.1) |
| Screening | 13 (100%) |
| 1 time | 0 |
| 2 or more times | 13 (100%) |
| HPV molecular biology performance | 12 (92.3%) |
| Positive results | 12 (92.3%) |
| Dysplasia | 9 (69.2%) |
| Low grade ICN (I-II) | 6 (46.2%) |
| High grade ICN alto (III-IV) | 3 (23.1%) |
| Cervical neoplasia | 0 |
ICN: intraepithelial cervical; HPV: human papilloma virus; SD: standard deviation.
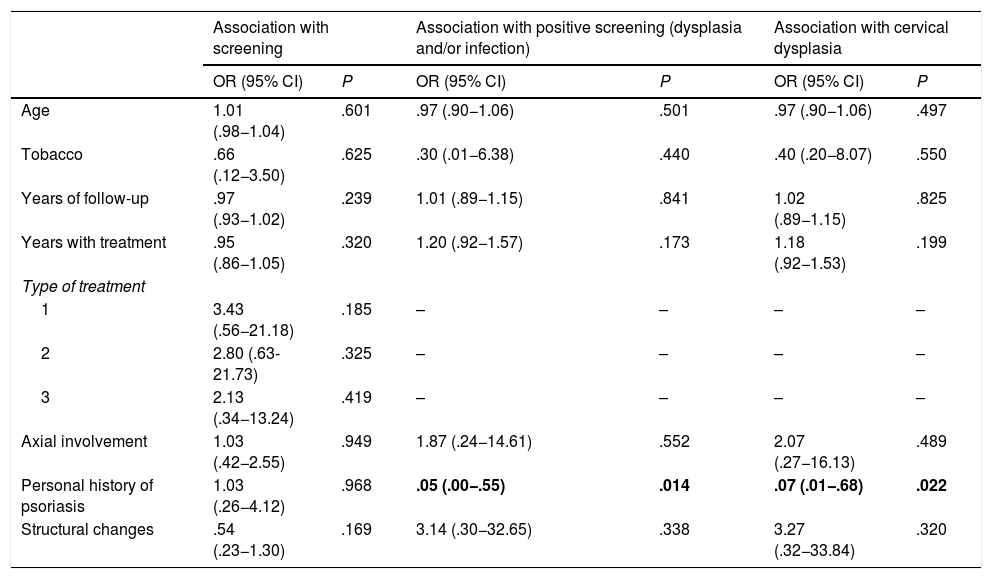
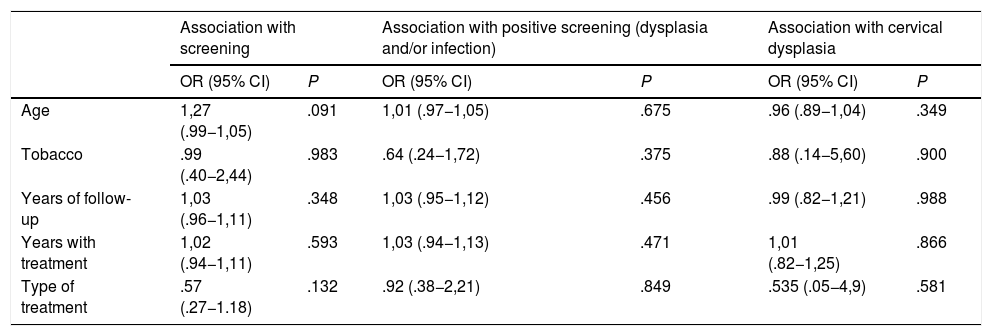
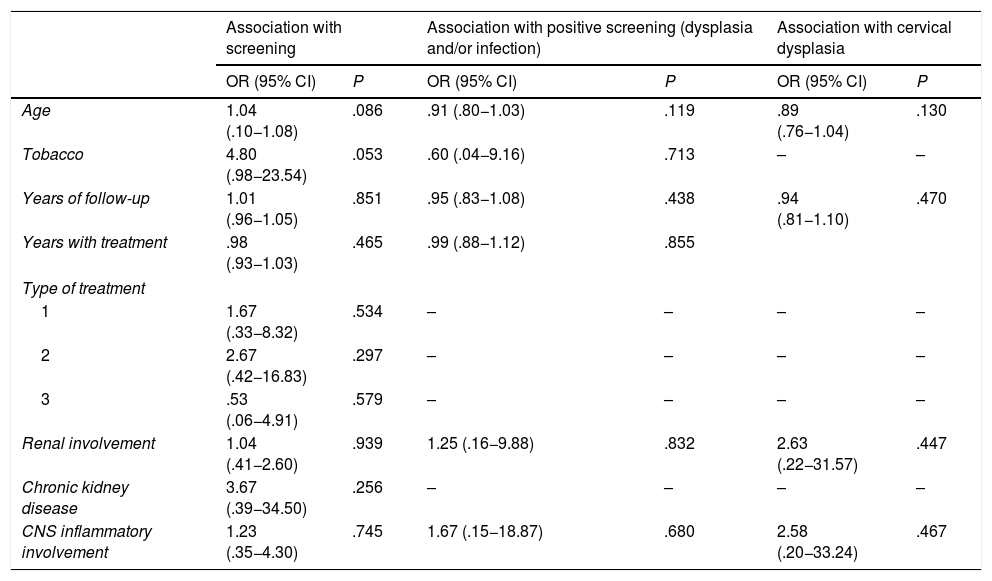
In the simple logistic regression analysis by type of baseline disease, no association was found between attending the screening programme and any variable. In the subgroup of patients with PsA, the presence of infection and cervical lesions was only associated with the presence of skin involvement, which was shown as a protective factor (OR .07 [CI .01−.68]; P = .02) (Table 2). No association was found between the presence of infection and/or dysplasia with any other risk factor or other disease characteristics in the RA and SLE subgroups (Tables 2–4). In view of study results, no multivariate adjustment was required.
Association study for psoriatic arthritis (simple logistic regression).
| Association with screening | Association with positive screening (dysplasia and/or infection) | Association with cervical dysplasia | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1.01 (.98−1.04) | .601 | .97 (.90−1.06) | .501 | .97 (.90−1.06) | .497 |
| Tobacco | .66 (.12−3.50) | .625 | .30 (.01−6.38) | .440 | .40 (.20−8.07) | .550 |
| Years of follow-up | .97 (.93−1.02) | .239 | 1.01 (.89−1.15) | .841 | 1.02 (.89−1.15) | .825 |
| Years with treatment | .95 (.86−1.05) | .320 | 1.20 (.92−1.57) | .173 | 1.18 (.92−1.53) | .199 |
| Type of treatment | ||||||
| 1 | 3.43 (.56−21.18) | .185 | – | – | – | – |
| 2 | 2.80 (.63-21.73) | .325 | – | – | – | – |
| 3 | 2.13 (.34−13.24) | .419 | – | – | – | – |
| Axial involvement | 1.03 (.42−2.55) | .949 | 1.87 (.24−14.61) | .552 | 2.07 (.27−16.13) | .489 |
| Personal history of psoriasis | 1.03 (.26−4.12) | .968 | .05 (.00−.55) | .014 | .07 (.01−.68) | .022 |
| Structural changes | .54 (.23−1.30) | .169 | 3.14 (.30−32.65) | .338 | 3.27 (.32−33.84) | .320 |
Treatment levels: 1 DMARD, 2 biologic and 3 sometimes DMARD + biologic.
IC: confidence interval; OR: odds ratio; P: P value. In bold: statistically significant values.
Association study for rheumatoid arthritis (simple logistic regression).
| Association with screening | Association with positive screening (dysplasia and/or infection) | Association with cervical dysplasia | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1,27 (.99−1,05) | .091 | 1,01 (.97−1,05) | .675 | .96 (.89−1,04) | .349 |
| Tobacco | .99 (.40−2,44) | .983 | .64 (.24−1,72) | .375 | .88 (.14−5,60) | .900 |
| Years of follow-up | 1,03 (.96−1,11) | .348 | 1,03 (.95−1,12) | .456 | .99 (.82−1,21) | .988 |
| Years with treatment | 1,02 (.94−1,11) | .593 | 1,03 (.94−1,13) | .471 | 1,01 (.82−1,25) | .866 |
| Type of treatment | .57 (.27−1.18) | .132 | .92 (.38−2,21) | .849 | .535 (.05−4,9) | .581 |
CI: confidence interval; OR: odds ratio; P: P value.
Association study for systemic lupus erythematosus (simple logistic regression).
| Association with screening | Association with positive screening (dysplasia and/or infection) | Association with cervical dysplasia | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | |
| Age | 1.04 (.10−1.08) | .086 | .91 (.80−1.03) | .119 | .89 (.76−1.04) | .130 |
| Tobacco | 4.80 (.98−23.54) | .053 | .60 (.04−9.16) | .713 | – | – |
| Years of follow-up | 1.01 (.96−1.05) | .851 | .95 (.83−1.08) | .438 | .94 (.81−1.10) | .470 |
| Years with treatment | .98 (.93−1.03) | .465 | .99 (.88−1.12) | .855 | ||
| Type of treatment | ||||||
| 1 | 1.67 (.33−8.32) | .534 | – | – | – | – |
| 2 | 2.67 (.42−16.83) | .297 | – | – | – | – |
| 3 | .53 (.06−4.91) | .579 | – | – | – | – |
| Renal involvement | 1.04 (.41−2.60) | .939 | 1.25 (.16−9.88) | .832 | 2.63 (.22−31.57) | .447 |
| Chronic kidney disease | 3.67 (.39−34.50) | .256 | – | – | – | – |
| CNS inflammatory involvement | 1.23 (.35−4.30) | .745 | 1.67 (.15−18.87) | .680 | 2.58 (.20−33.24) | .467 |
Treatment levels: 1 oral or intravenous glucocorticoids and non biologic immunosuppressants, 2 biologics and 3 cyclophosphamide + biologics (not necessarily at the same time).
CI: confidence interval; CNS: central nervous system; OR: odds ratio; P: P value.
Rheumatologic diseases and their treatments may imply systemic involvement and an immunosuppression status which has been associated with a greater rate of infections, malignant tumours and the need for organ transplants.15 Among the latest recommendations from the Spanish Society of Rheumatology on risk management of treatment with biologic therapies in patients with rheumatic diseases (2011), are to be found surveillance of neoplasias and infections before and during treatment, but with no inclusion of specific recommendations on screening for infection, dysplasia and neoplasia caused by HPV.16 In our series we found no information relating to surveillance of cervical lesions in 42.3% of patients reviewed during their years of follow-up in the public health service.
These data of low adherence to screening contrast with those published in the latest National Health Survey (ENSE 2017), where 75.3% of women aged ≥15 years had had a pap smear test at some time in their life whilst 24,7% had never received a pap smear test.17
There are potential explanations for this absence of data referring to screening in our patients. In Spain, screening recommendations began in 2006, with each autonomous community establishing its own programme. On the one hand, there are patients who came to our province, who could have been assessed in other communities, but the dispersion of medical records amongst different communities did not encompass suitable healthcare follow-up. On the other hand, the patients could have gone for private healthcare gynaecological consultations, and we would therefore lack these data as they would not be recorded on the electronic programmes used by the public health authorities. Regarding socio-educational level, adherence to screening programmes varies depending on factors such as the women’s professions or their educational level. It is lower amongst unskilled workers and in the group of women with a basic educational level. In this sense, in our community, no major differences existed in the age group of women aged between 25–65 years from the rest of Spain. In our region percentages were of 39.4%, 24.3% and 36.3% of women with primary, secondary and further educational levels, respectively, compared with 38.3%, 22.7% and 38.9% of the national levels.18 In any event, it is remarkable that the rheumatologists in our area do not perform directed anamnesis regarding risk factors of cervical neoplasia in a large proportion of our patients. However, this was a retrospective study using reviews of electronic medical records and several patients were followed up in outpatient rhaumatology units years before the development of the electronic platforms like Orion or Abacuses. This means there were possible losses of cytology reports, HPV tests and precursor lesion treatment and invasive carcinoma in some of them, with the possible under-estimation of adherence to screening tests by our patients.
In Spain a rate of cervical neoplasia of 10.2/100,000 patients per year has been reported.19 With regard to the prevalence of infection, dysplasia and cervical neoplasia in our patients, as this was a retrospective study we were unable to compare the incidence with those of sexually active women in the general population. The prevalence of dysplasia was greater in the group of patients with SLE, followed by the RA group and then the PsA group. No cases of cervical neoplasia were found. We found few studies which specifically analysed the risk of cervical lesions in different types of rheumatologic disease with unequal results. One cohort study with a national Swedish register showed that patients with RA had, compared with the general population, a higher risk of developing cervical dysplasia, regardless of the treatment used. However, the rate of grade I–II intraepithelial cervical neoplasia and invasive cervical cancer increased in patients who used anti-TNF therapy compared with those who were diagnosed with RA but without biologic therapy.12 In one meta-analysis which included observational studies published between 2008 and 2014, no increase in the relative risk of cervical cancer in patients with RA was observed, compared with the general population.13 Other studies performed in patients with RA, myositis, polymyositis, systemic sclerosis and SLE only reported an increase in the risk of cancer in patients with SLE.14 No studies were found with patients with PsA.
The low prevalence of infection by HPV, dysplasia and neoplasia obtained in our study could be impacted by the low adherence to screening, the possible loss of cytology and molecular biology reports in private medicine and the loss of information not included in the computerised clinical report. Also, the sample size of our series was lower than that used in other published studies, with most of them being multicentre or populational.12–14 It is of note that in this study patients with a background of neoplasia and immunosuppressant treatment receptors from causes other than RA, PsA and SLE were excluded, and therefore in some cases we could be underestimating the role of the association of these diseases with the appearance of infection, precursor lesions and cervical neoplasias.
The study did not show there was any association between a higher prevalence of infection and/or dysplasia and risk factors (age, tobacco, presence or absence of stable partner, years with the type of treatment associated with a higher degree of immunosuppression or with certain disease characteristics), with the exception of the personal background of psoriasis in patients with PsA, where an association was observed with a lower prevalence of infection and/or dysplasia. However, it should be remembered that we were unable to collect information regarding HPV infection risk factors in a considerable percentage of cases. No data were able to be obtained on the presence or absence of a stable partner in any case. Regarding a tobacco habit, no data were found in over half of the records observed. Neither were we able to obtain data on other possible factors which could have had an impact on the screening programmes, such as the socio-economic level of these patients. In the subgroup of patients with PsA we were unable to explain the association of HPV infection and/or dysplasia with a background of psoriasis, nor were we able to find literature which described this association. However, the low frequency of infection and/of dysplasia in this group and the absence of differences in the treatment of these patients, suggested that this result could have been randomized.
In no diseases were we able to assess the association between the different levels of immunosuppressant treatment and the adherence to screening, infection or the presence of cervical lesions, since all women were undergoing treatment for their disease. Regrouping of these different types of treatment could have been considered, which made sense from a statistical viewpoint but it was not considered useful in this study, since the same level of immunosuppression was not presented.
Previously mentioned limitations point to the need to conduct new prospective studies with a larger patient sample. Also, the difficulty in finding information in the electronic medical records on some risk factors for cervical neoplasia, which are common to the development of other malignancies, should serve as reflection on certain aspects of daily clinical practice in the consulting practices of any speciality. Despite the absence of specific recommendations of the early detection of HPV aimed at women with rheumatologic diseases in the new population screening proposals in Spain and in the consensus regarding biologics management, it is the job of all healthcare professionals to be aware of the screening recommendation for the whole general population and for immunodeficient patients so that they are screened with appropriate frequency.
To conclude, the anamnesis of risk factors of cervical dysplasia is insufficient in the medical records of patients in our area with RA, PsA and SLE, in treatment with immunosuppressants. According to the data from the electronic medical records, these patients do not follow general or specific recommendations for cervical cancer screening tests. Despite this, the frequency of precursor lesions and cervical neoplasia in patients where data is available, do not appear to be greater than that of the general population. No association of the type of disease and the treatment received was able to be established with the risk of developing these lesions.
Authorship/collaboratorsAll the authors participated equally in the undertaking of this study and the redaction of the article:
Blanca Vidal Alejandre, Ernesto Tovar Sugrañes and Raquel López Poza: data acquisition, data analysis and drafting of the article.
Mariano Andrés: critical review of the intellectual content and final approval of the view presented.
M. Paz Martínez-Vidal: study conception and design; critical review of the intellectual content and final approval of the version presented.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Vidal Alejandre B, Tovar Sugrañes E, López Poza R, Andrés M, Martínez-Vidal MP. Cribado del virus de papiloma humano: evaluación de grado de vigilancia en artritis reumatoide, artritis psoriásica y lupus eritematoso sistémico. Reumatol Clin. 2021;17:494–498.