Antiphospholipid syndrome is defined as a hypercoagulability state with episodic arterial or venous thrombosis and recurrent fetal loss in the presence of antiphospholipid antibodies.1,2 Arterial thrombosis is less common than venous thrombosis and peripheral arteries are only affected in 25% of events.3 Among the peripheral arterial thrombosis, upper limbs are only affected in 2.7% of cases.4
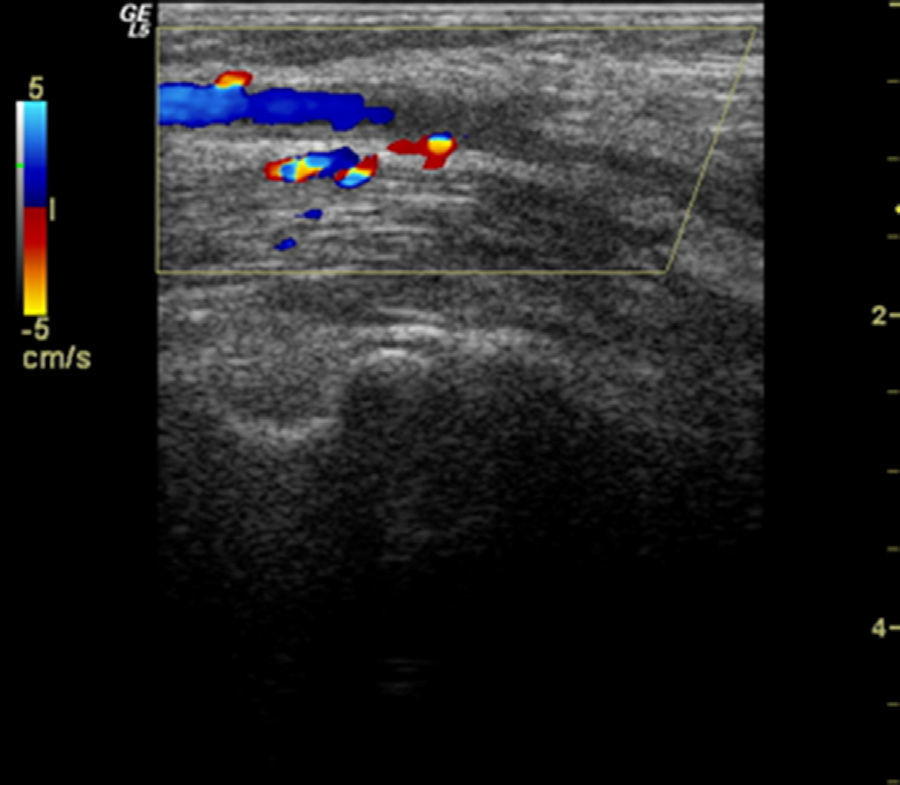
We present the case of a patient with left humeral artery thrombosis and antiphospholipid syndrome, who presented with atypical symptoms. The patient, a 66-year-old woman with a history of smoking (30 packs/year) and with mild hypertriglyceridemia, came to the clinic due to urgent pain, swelling and functional impairment of the left elbow which began acutely seven days prior, associated with a decrease in the hand on the same side, with no fever or other clinical manifestations. Upon examination we found a swollen and functionally limited elbow (flexion 40°) with erythema and increased local temperature. The fingers felt cold and there was a reduction in the radial pulse compared to the contralateral side, but with good capillary flow. Laboratory analysis showed: CRP 115mg/dl; D dimer 469ng/ml; fibrinogen 550mg/dl; leucocytes 13.4×109/l (10.8×109/l). An echographic study was performed ruling out joint affection but showing the existence of a hypoechoic, heterogeneous thickening of the extensor-supinator muscles (Fig. 1). A Doppler study showed an occlusion of the humeral artery at the elbow flexure. Vascular surgeons, who began treatment with cilostazole, low molecular weight heparin and aspirin, confirmed these findings. When searching for the underlying cause we found the presence of positive lupus anticoagulant in two separate determinations 3 months apart, with negative anticardiolipin and anti-b2-glucoprotein 1 antibodies. With the diagnosis of thrombosis of the humeral artery in the context of antiphospholipid syndrome we recommended oral anticoagulation with acenocoumarin, with a good progression.
Acute arterial thrombosis is the sudden interruption of blood supply due to the obstruction of the artery that irrigates a specific territory, due to prior stenosis or the existence of an aneurysm at that level, generally having a precipitating factor (hypercoagulability, low cardiac output, etc.). It is clinically manifested as intense pain, pallor, coldness and loss of distal strength, with abolished distal pulse. In our patient, in addition to the poor frequency with which humeral artery occurs, most of the typical signs of acute arterial thrombosis were absent and rather simulated an acute elbow arthritis. When reviewing the literature we have only found descriptions of pain and impairment of the elbow when humeral artery thrombosis is associated to suprachondileal fractures,5,6 as opposed to our case.
Please cite this article as: Feced Olmos CM, Alegre Sancho JJ, Ivorra Cortés J, Zaragozá García JM. Trombosis de la arteria humeral simulando una monoartritis de codo en una paciente con síndrome antifosfolipídico primario (síndrome de Hughes). Reumatol Clin. 2014;10:135–136.