Kikuchi–Fujimoto's disease (KFD) is a rare, benign and self-limited disease which on rare occasion may be associated with systemic lupus erythematosus (SLE), and may be present before, after or simultaneously. We analyze the case which demonstrates the relationship between both diseases.
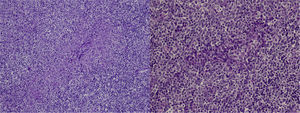
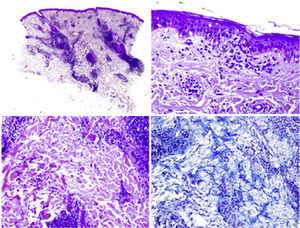
Case DescriptionA 22-year-old woman with no personal history came to the hospital due to fever and cervical lateral adenopathy which started 15 days prior. Laboratory tests show leukopenia 2800 per mm3 (with no lymphopenia), normocytic, normochromic anemia (hemoglobin 11g/dl, hematocrit 34%, mean corpuscular volume 85.9, mean corpuscular hemoglobin 28.6pg) and ESR 85mm/h. The blood chemistry and urine sediment shows no abnormalities. HIV, B and C hepatitis, toxoplasma, rubeola, Epstein–Barr virus and cytomegalovirus were negative. Blood cultures and Mantoux tests were negative. Autoimmunity tests showed positive ANA with a 1/320 titer (homogeneous pattern), negative anti-DNA, negative rheumatoid factor and normal complement levels. Thorax and abdominal CT showed multiple cervical and inguinal adenopathies. A bone marrow aspirate-biopsy was performed, as well as cultures, which were all negative. A cervical lymph node biopsy was performed, showing paracortical necrosis with cell detritus and numerous hystiocytes, compatible with necrotizing lymphadenitis or KFD (Fig. 1). In the following years the patient remained stable, with no further episodes of fever, although she did present self-limited cervical adenopathy. She repeatedly presented painful oral ulcers and further analysis confirmed leukopenia (without lymphopenia). Three years later she presented painful erythematous nodules on the forehead and cheeks (Fig. 2). Laboratory tests revealed positive ANA with a titer of 1/160 with a homogeneous pattern and low complement levels. A skin biopsy was compatible with discoid lupus (Fig. 3). Therefore, considering clinical and laboratory criteria, she presented 4 or 11 classification criteria for SLE (positive ANA, painful, repeated oral ulcers, leukopenia, discoid lupus). She was treated with hydroxicloroquine with a reduction in skin lesions after approximately 2 weeks (Fig. 4).
EKF was described in 1972 and is characterized by the onset of fever and cervical lymphadenopathy.1–3 It affects mainly young women. It is rare (found only in some series of cases1), and was first described in Japan, but is becoming more common in western countries.4 Its etiology is unknown, although the most accepted hypothesis is that the etiology is viral.1,2,5 It may be associated with different connective tissue diseases, such as Still's disease, Sjögren syndrome, polymyositis, rheumatoid arthritis, and above all, SLE.3,6 Common symptoms at presentation are fever, myalgia, weight loss, nausea and vomiting as well as skin lesions.1,3,7 The differential diagnosis includes infections (toxoplasmosis, mononucleosis, tuberculosis, etc.) and lymphoma.1–3,5 Laboratory tests may show leukopenia, mild thrombocytopenia and neutropenia, and increased acute phase reactants, mainly ESR.5,8 Histology reveals paracortical foci of necrosis with abundant nuclear debris, histiocyte infiltrates, with no neutrophils.1–3,7,8 KHD and lupus lymphadenitis may be histologically identical. Only in a few cases where the pathologist can observe hematoxiphillic bodies (aggregates of basophilic material in the lymph node sinuses), accumulation of DNA in the vessel wall, vasculitis or areas outside the area of necrosis which suggest lupus lymphadenitis and KHD.9 The literature contains several case reports of KHD associated with SLE, and EKF may occur before, after or simultaneously with SLE.4,5,7–12 The main difference between them is the prognosis, with the majority of cases of KHD resolving spontaneously in 1–4 months.3,8
ConclusionsIn this case, the patient was initially diagnosed with a histologically confirmed KHD in which we ruled out other possible causes, mainly infectious or hematologic disease, as the origin of lymphadenopathy and fever. We believe this case supports the recommendation that a possible association between KFD and SLE should be always considered, as well as the need to closely monitor the progression of KHD with SLE.
Please cite this article as: Diez-Morrondo C, et al. Inicio de lupus eritematoso sistémico como enfermedad de Kikuchi-Fujimoto. Reumatol Clin. 2012;8:153–5.