To collect information about diagnosis, classification and treatment of patients at high risk of fracture in the rheumatologist's practice.
Material and methodsA survey was conducted among Spanish rheumatologists. The survey was aimed at gathering data on the physician's healthcare activity; the osteoporosis (OP) and fracture risk factors were considered as most relevant; the diagnostic used tests and the treatment indication according to the presence of different risk factors.
Results99.5% of rheumatologists felt that there is a group of patients with OP at high risk of fracture. Previous fracture was considered the most important risk factor, particularly in case of multiple fractures, severe fractures, hip fracture, or that occurred during treatment. Glucocorticoid treatment, older age and low bone mineral density were considered, in this order, other important risk factors. The number of vertebral fractures was considered the most relevant radiological data, followed by the fracture's chronology and severity. Most of the respondents selected teriparatide as the first treatment option in high-risk patients.
ConclusionsThe definition of OP patient with high risk of fracture is not uniform in daily practice, although the majority of rheumatologists considered that having a previous fracture is the most important risk factor, followed by glucocorticoid treatment, older age and low BMD. Anabolic treatment was the approach most commonly used in OP patients with high risk of fracture.
Recoger información sobre cómo se realiza el diagnóstico, la clasificación y el tratamiento de los pacientes osteoporóticos con alto riesgo de fractura en las consultas de Reumatología.
Material y métodosSe realizó una encuesta a reumatólogos españoles que atienden de forma habitual a pacientes con osteoporosis (OP), donde se recogieron datos demográficos, clínicos y sobre los factores de riesgo de OP y de fractura considerados más importantes, así como pruebas diagnósticas y tratamiento según el riesgo de fractura de los pacientes.
ResultadosEl 99,5% de los reumatólogos encuestados consideraba que existe un grupo de pacientes con OP con alto riesgo de fractura, siendo la fractura previa el factor de riesgo más importante, riesgo que se incrementaba en caso de fracturas múltiples, severas, de cadera, o si se presentaban en pacientes tratados. Le siguieron en orden decreciente el tratamiento con glucocorticoides, la edad avanzada y la densidad mineral ósea (DMO) baja. El número de fracturas vertebrales fue considerado el dato radiológico más importante, seguido de la cronología y la severidad de las fracturas. En pacientes calificados de alto riesgo, la mayoría de los encuestados seleccionó teriparatida como primera opción de tratamiento.
ConclusionesLa definición de paciente con OP con alto riesgo de fractura en la práctica diaria no es homogénea, aunque la mayoría de reumatólogos consideró que el factor más importante es tener fractura previa, seguido del tratamiento con glucocorticoides, edad avanzada y DMO baja. El tratamiento osteoformador es el más utilizado en pacientes con OP con alto riesgo de fractura.
Osteoporosis (OP) is a skeletal disorder characterized by a decrease in bone strength predisposing an increased risk of fracture.1 The risk of fracture resulting from bone fragility is the most important clinical aspect of the disease.2 In the United States, approximately 10 million individuals suffer from OP or have a low bone mineral density (BMD), which can lead to fractures.3 In Spain, the disease affects approximately 15% of the female population, with a prevalence of 26% in women aged 50.4
Although fractures can occur in different locations, vertebral and hip fractures are of particular clinical importance because of their high prevalence, their impact on the quality of life of patients and their associated morbidity. The presence of one or more vertebral fractures multiplied by 5 the risk of new vertebral fractures in a period of one year5 and also increases the likelihood of suffering a hip fracture.6,7 However, vertebral fractures are not always recognized in time, which reduces the opportunities to identify and properly treat patients.8 Moreover, hip fractures are characterized by slow and often incomplete recovery, so a high proportion of patients require long-term care and ongoing support for walking.2,9 Hip fracture is associated with a high mortality,10 most deaths occurring in the first 3–6 months after the fracture.2
Osteoporotic fractures also have a major impact on healthcare budgets. It is estimated that by 2025 the annual cost of these fractures may rise to 25000 million dollars in United States11 and in 2050 the cost in Europe will be 76700 million euros.12 In Spain, the cost of hospital admissions resulting from hip fracture amounts to 220 million euros a year.13 Therefore, appropriate fracture risk stratification may help identify those patients most at risk and thus facilitate early treatment, with a consequent reduction in the likelihood of future fractures. Unfortunately, there is no universally accepted methodology on how to identify patients at high risk for fracture2,14,15 and there are no well-known criteria used in everyday practice of specialists for the management of these patients. For this reason, we set out to gather information about the Spanish rheumatologist assessment of the risk of fracture and how the diagnosis is made, the disease classified and patients when at high risk of osteoporotic fracture during their practice.
Material and MethodsAs part of the OSTEOPAR project, a group of experts in OP designed a survey that included 27 questions to obtain information on the profile of the surveyed rheumatologists, characteristics of clinical activity, assessment of risk factors (RF), patient assessment, choice of diagnostic tests and circumstances for which they are requested, and the treatment for which they qualify based on the patient's clinical characteristics (see Appendix A).
All responses were obtained by selecting one or more predetermined options in the questionnaire, except the last question, which asked respondents to define patients at high risk of fracture, using up to 200 characters of free text.
Different sections of the questionnaire specifically collected data on:
- (1)
Characteristics of the participating physician. Workplace, years of professional experience in their specialty and Autonomous Community where the respondent was located at.
- (2)
Characteristics of clinical activity. Total number of patients and patients with OP seen per week, percentage of patients with primary OP, origin, percentage with fractures and fracture type.
- (3)
Assessment of the RF and the patient. Questions were made about the importance of several RF and high risk of osteoporotic fracture according to their degree of influence over diagnostic and/or therapeutic decision-making. Respondents made the assessment on a numerical scale from 1 to 5, where: 1=not important, 2=of little importance, 3=moderately important, 4=very important and 5=highest importance. Also, the surveyed were requested to order, by degree of importance, the 3 RF for fracture considered as more relevant. Regarding the assessment of the patient, we asked which option or options they preferred when faced with a patient with OP presenting back pain of recent onset or changes in their usual features, if exploring the spine for the presence of kyphosis or other deformities, and if they commonly used scales for assessing fracture risk and frequency of the use of the FRAX tool.
- (4)
Diagnostic tests. Circumstances in which the respondent requested a lateral spine X-ray, value given to the different characteristics of morphometric vertebral fracture (on the above mentioned scale of 1–5) and whether or not an analysis of bone metabolism was performed.
- (5)
Assessment of fracture risk and treatment options. How respondents rate the risk of fracture in 4 pre-defined patient-profiles (using the terms “high”, “medium” or “low”) and what treatment would be chosen as first, second and third options for each profile. Predefined profiles in the questionnaire were as follows: Profile 1: 65-year-old woman presented vertebral fracture after 5 years of treatment with bisphosphonates. Profile 2: 59-year-old woman in chronic treatment with bisphosphonates and a T-score of −2.5. Profile 3: 70-year-old woman without treatment with a T-score of −2.8 in the femoral neck and presenting 2 vertebral fractures. Profile 4: A 55-year-old man with a T-score of −1.5 in chronic treatment with glucocorticoids. Additionally, respondents were asked to determine whether supplemental calcium and vitamin D should be used for each profile, as well as if treatment for OP should be employed and what would the physician choose among the following: estrogen receptor modulators, oral or intravenous bisphosphonates, strontium ranelate, PTH (1–84) and teriparatide.
Finally, respondents were asked to evaluate whether, from their point of view, there was a group of patients at high risk of fracture and whether their behavior would be different toward these patients.
Descriptive statistics based on the calculation of percentages, means and medians was used and data analysis was carried out using SPSS software version 18.0. When appropriate, the analysis also included the standard deviation, mode, variance and percentiles, as well as maximum and minimum values.
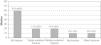
ResultsActivities of the Rheumatologists Surveyed174 surveys were performed and collected from specialists in Rheumatology located throughout the national territory (Fig. 1) and who routinely treat patients with OP.
97.2% (N=169) of respondents claimed to work in the public health system, including this hospital and other hospitals, such as specialty and outpatient centers. 26.5% (N=46) had a private practice. Of those who developed their daily work exclusively in public centers, 55.2% (N=96) worked in hospitals, 4.6% (N=8) in non-hospital centers and 13.2% (N=23) both in hospitals and non-hospital centers. 2.9% (N=5) exercised their daily work exclusively in a private practice and 23.6% (N=41) reconciled public work with their private practices.
71.8% had 10 or more years of professional experience in their field, with a range of 0–5 years to more than 20 years. The patients came mostly from primary care (median, 31%–40%), a high percentage of the clinic itself (mean 21%–30%), with a minority referred from other specialties. The number of OP patients seen weekly varied considerably, with a minimum of 5 and maximum of 250 (mean 29.08±25.0), although after grouping the number of patients seen per week in intervals of 10, it was observed that 92% of respondents saw between 5 and 50 patients. 75.2% of those surveyed responded that more than 50% of patients had primary OP.
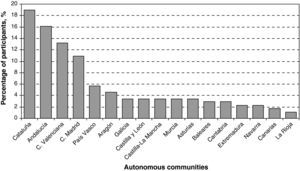
Fracture Types and Their ImpactOver 40% of patients seen by respondents had fractures that were located mainly on the spine and to a lesser extent on the hip (Fig. 2).
Risk FactorsStandard Risk FactorsRespondents believed that the different RF for osteoporotic fracture have a disparate impact when making treatment decisions and/or diagnosis, with a previous fragility fracture, treatment with oral corticosteroids, age, BMD and the presence of secondary OP being the most important RFs in this regard. Instead, alcohol use, sedentary lifestyle, smoking, low intake of calcium rich foods or low exposure to sunlight were considered less relevant and ad a low or moderate importance for diagnostic decisions and/or treatment (Table 1). When choosing the most important 3 RF, previous fragility fracture and age were considered the most important. A previous fragility fracture, treatment with oral corticosteroids, age and BMD were considered second in importance, and treatment with oral corticosteroids, BMD and age were considered in third place of importance. None of the respondents selected smoking, use alcohol, other therapies (anticonvulsants, benzodiazepines, antiaromatase agents, anticoagulants, lithium, thiazolidinediones, etc.), the presence of rheumatoid arthritis, low intake of foods rich in calcium and low sun exposure as the first FR.
Evaluation of Risk Factors for Osteoporotic Fracture in Relation to the Influence It Has on Therapeutic and/or Diagnostic Decision Making.
| Risk Factors to Evaluate | Mean | Percentage of Participants Selecting This Option |
| History of pathologic fracture | 4.7 | 79.9 |
| Treatment with oral steroids | 4.5 | 55.2 |
| Age | 4.1 | 33.9 |
| BMD | 4 | 42.5 |
| Secondary osteoporosis | 4 | 44.8 |
| Early menopause/hypogonadism | 3.9 | 42 |
| Family history of hip fracture | 3.9 | 49.4 |
| Rheumatoid arthritis | 3.8 | 42 |
| Loss of height | 3.7 | 41.4 |
| Tendency to fall | 3.7 | 40.2 |
| Gender | 3.4 | 38.5 |
| Other treatments (antiepileptics, benzodiazepines, thiazolidinediones, etc.) | 3.3 | 40.8 |
| BMI | 3.2 | 36.8 |
| Alcohol consumption | 3.2 | 39.7 |
| Smoking | 3 | 44.8 |
| Sedentarism/immobility | 3.1 | 43.7 |
| Low calcium consumption | 3 | 46 |
Evaluation from 1 to 5 (1=no importance and 5=maximum importance). The mean score and the percentage of those surveyed selecting each factor is shown.
Respondents felt that there are some particularly high importance RF for fracture involving differences in treatment decision-making. Among these risk factors, those considered with a maximum or high importance, and in this order, were: the presence of multiple fractures (vertebral and/or spinal), hip fracture, severe vertebral fracture, fracture despite treatment, vertebral fracture and treatment with glucocorticoids (doses equivalent to >7.5mg/day of prednisone for an extended period) (Table 2).
Evaluation of High Risk Factors for Osteoporotic Fracture in Relation to the Influence Each Has on Therapeutic and/or Diagnostic Decision-Making.
| Mean | Percentage of Patients Who Chose This Option | |
| Multiple fractures | 4.7 | 81.6 |
| Hip fracture | 4.7 | 79.9 |
| Severe vertebral fracture | 4.6 | 75.3 |
| Fracture in spite of treatment | 4.5 | 69.5 |
| Vertebral fracture | 4.4 | 58.6 |
| Chronic steroid treatment (>7.5mg) | 4.2 | 36.2 |
| Baseline BMD<−3.5 | 3.8 | 43.7 |
| Age>70 | 3.8 | 36.3 |
| Secondary osteoporosis | 3.8 | 42 |
| Presenting Colles fracture | 3.6 | 43.1 |
| Loss of bone mass in spite of treatment | 3.6 | 42 |
| Propensity to fall | 3.6 | 39.1 |
| Patient with more than 2 FR | 3.5 | 44.8 |
| Loss of height>2cm in the first year | 3.5 | 36.2 (for scores 3 and 4) |
| BMI<19 | 3.3 | 38.5 |
| Recent dorsolumbar spine pain | 3.3 | 37.9 |
Evaluation from 1 to 5 (1=no importance and 5=maximum importance). The mean score and the percentage of those surveyed selecting each factor is shown.
In a patient with OP presenting back pain, the majority of rheumatologists (56.9%) performed an examination of the patient, request X-rays and also prescribe an analgesic treatment regimen, although it is noteworthy that 95.9% of respondents at least would ask for a radiograph (Fig. 3, panel A). 98.3% of rheumatologists mentioned exploring the spine of their patients seeking deformities, either on the first visit (78.9%) or as a response to the findings mentioned in the examination (18.4%).
51.1% of participants reported using rating scales for fracture risk, with FRAX the most commonly used (97.5%), either alone or combined with other scales. 79.3% of respondents who used FRAX scale, used it routinely or in certain situations (Fig. 3, panel B).
Lateral Radiograph of Spine87.9% of respondents answered that a lateral spine X-ray was requested during the initial patient assessment. This percentage includes those who do so exclusively on the first visit (7.5%), in addition to those who do so if the patient has acute back or lumbar (28.7%) pain and, additionally, for patient follow-up (35.1%). 6.3% only requested it if the patient has acute back or lumbar pain.
Faced with a morphometric vertebral fracture, the number of fractures is the most important piece of information for the survey participants, followed distantly by the timing of the fracture, the degree of deformity of the fracture and its location (Table 3).
Morphometric Evaluation of Vertebral Fracture.
| Mean | Percentage of Participants Choosing This Option | |
| Number of fractures | 4.65 | 75.9 |
| Recent or old | 3.66 | 42.5 |
| Degree of deformity | 3.43 | 34.5%, score 4 and 33.3%, score 3 |
| Localization | 3.22 | 36.2 |
| Radiology report | 2.18 | 27.6%, score 2 |
Evaluation from 1 to 5 (1=no importance and 5=maximum importance). The mean score and percentage of those surveyed that chose each factor are shown.
80.5% of respondents requested an analysis of bone metabolism only in the first visit; a minority only requests it during treatment (10.9%) or does not request it (8.6%). Metabolic parameters frequently determined are serum calcium (29.6%), bone turnover markers (25.2%), vitamin D (21.4%) and PTH (11.3%).
Risk Assessment and Treatment of the Four Different Patient ProfilesIn order to know the assessment of fracture risk in different types of patients, the questionnaire raised four preset profiles of patients to which the respondent assigned one of three possible increased levels of risk (as described in the material and methods section):
The results of this assessment are presented in Table 4.
Evaluation of the Risk of Fracture (High, Medium or Low) in the Four Predefined Profiles of Patients.
| Profile 1 | Profile 2 | Profile 3 | Profile 4 | |
| High risk | 92.5 | 20.7 | 99.4 | 43.7 |
| Medium risk | 6.9 | 51.1 | 0.6 | 47.7 |
| Low risk | 0.6 | 28.2 | – | 8.6 |
Percentage of rheumatologists selecting a determined risk in each profile are shown.
For high-risk profiles (profiles 1 and 3) most selected teriparatide as first-line treatment (Table 5). For profile 4, considered by over 90% of respondents from moderate to high risk, the first choice of treatment was oral bisphosphonates, while the first option for profile 2, scored mostly as a medium risk, was oral bisphosphonates or strontium ranelate. Treatment with calcium and vitamin D is always used by the vast majority of respondents and for all profiles (97.1%, 92.0%, 98.9% and 98.3%, respectively), without specialist that never used it.
Treatment Preferences in the 4 Predefined Patient Profiles.
| Calcitonin | Raloxifene | Oral BPP | IV BPP | Ranelate | PTH (1–84) | Teriparatide | |
| Profile 1 | |||||||
| No | 96 | 92 | 90.2 | 55.2 | 33.9 | 38.5 | 6.9 |
| 1st option | 0.6 | – | 2.3 | 2.3 | 11.5 | 9.2 | 77 |
| 2nd option | – | 0.6 | 2.9 | 13.8 | 22.4 | 40.8 | 12.6 |
| 3rd option | 3.4 | 7.5 | 4.6 | 28.7 | 32.2 | 11.5 | 3.4 |
| Profile 2 | |||||||
| No | 98.3 | 62.6 | 46 | 70.1 | 19 | 83.3 | 59.8 |
| 1st option | – | 15.5 | 36.8 | 4 | 31.6 | – | 5.7 |
| 2nd option | – | 14.4 | 9.2 | 15.5 | 27 | 5.2 | 14.9 |
| 3rd option | 1.7 | 7.5 | 8 | 10.3 | 22.4 | 11.5 | 19.5 |
| Profile 3 | |||||||
| No | 96.6 | 97.7 | 53.4 | 44.3 | 60.9 | 47.1 | 9.8 |
| 1st option | 0.6 | – | 14.9 | 6.9 | 0 | 8× | 72.4 |
| 2nd option | 0.6 | – | 14.4 | 22.4 | 13.2 | 37.4 | 12.1 |
| 3rd option | 2.3 | 2.3 | 17.2 | 26.4 | 25.9 | 7.5 | 5.7 |
| Profile 4 | |||||||
| No | 96.6 | 96.6 | 8.6 | 42.5 | 62.6 | 87.4 | 43.1 |
| 1st option | – | – | 82.8 | 5.2 | 1.1 | 0.6 | 5.7 |
| 2nd option | 0.6 | 0.6 | 6.3 | 35.1 | 20.1 | 4 | 22.4 |
| 3rd option | 2.9 | 2.9 | 2.3 | 17.2 | 16.1 | 8 | 28.7 |
Percentages of rheumatologists choosing a certain treatment in each profile is shown.
Facing a high risk patient, 33.3% of respondents chose the option of starting treatment and monitoring more closely, and 21.8% answered that they would also request further diagnostic tests in these patients.
Respondents identified the patient at high risk based on 3 main criteria: presence of RF (47.5%), when two or more RF are present and current or previous fracture (34.4%), and only the presence of osteoporotic fracture without considering other risk factors (14.2%).
DiscussionBecause the clinical significance of osteoporosis lies primarily in the risk of fracture and the morbidity and mortality associated with it, treatment guidelines suggest that it may be more important to identify patients at high risk of fracture than the OP patient properly.2 Therefore, fracture risk stratification is necessary to distinguish between patients with a high probability of presenting them from those in which this probability is lower. Risk assessment helps to identify individuals at higher risk and therefore guides therapeutic decisions as well, and this estimation probably produces a greater awareness on the part of the clinicians who care for these patients and results in a more complete intervention.
Although guidelines recommend14 drug treatment be assigned based on the risks and benefits in individual patients, there are no specific indication about the risks and benefits that should be assessed by the specialist and therefore, in many cases are difficult to apply in the clinical practice.
Through the OSTEOPAR project, using an online survey, we tried to identify the views of rheumatologists in Spain on various RF and especially what they mean by patients at “high risk of fracture” and how the management is carried out in clinical practice.
Respondents felt that previous fracture and age were the two most important standard RF, while a single value of BMD was considered of lesser impact. A previous fracture as the best predictor of fracture is consistent with the evaluation of other authors16 and the guidelines published by the SEIOMM,17 although the order of priority established by the respondents to prior fracture and age varies slightly from previous18 guidelines. Other studies have shown that in both men and women, age is an important fracture RF, independent of BMD.2,19 The secondary role assigned to the BMD by the respondents is consistent with the general view of the guidelines and the previous observation that many patients can present fractures despite having a relatively well preserved BMD.2,18,20 Although BMD has traditionally been considered a predictor of fracture, there is no accurate way to identify individuals who will suffer it.21 Indeed, the opinion of respondents agrees with previous analysis, in which it must be considered in conjunction with biochemical indices of remodeling and other laboratory values16,17,22 and that treatment should be considered rather in terms of risk of fracture given by the clinical RF rather than by the isolated value of BMD.2,20 In contrast to other published23 risk assessments, our findings tended to evaluate BMI as a moderate RF, even lower than height loss or a tendency to fall. It is possible to take into account that FRAX computes BMI as a proxy for BMD24 and therefore assigned a lower relevance to this parameter. The majority used FRAX-including scores used as a preventive strategy, a finding that is supported by the guidelines.25
Among other factors, it has been suggested that the presence of vertebral deformities and timing of fractures may be a first sign of weakness that identifies high-risk patients.5,26 In this sense, almost 90% of rheumatologists surveyed said an X-ray of the thoracolumbar spine was useful to assess the presence of vertebral fractures. While the vast majority of reviewers explore the spine in search of kyphosis or other deformities, they felt that both factors are secondary in importance to the number of fractures. This exploratory strategy is consistent with recommendations previously set, according to which physical examination and radiography are indicated for the detection of vertebral alterations.17,27
According to survey results, treatment usually begins in patients with previous osteoporotic fractures, which is consistent with the American (ACP) 14 and the European (NICE) guidelines.9
Teriparatide occupied a prominent position as a treatment option in the profiles of those considered at high risk for fracture (profiles 1 and 3), while oral bisphosphonates were the treatments of choice for the majority of respondents in medium-risk patients (profiles 2 and 4). The choice of teriparatide as a treatment in patients at high risk of fracture is supported by the pivotal trial (Fracture Prevention Trial), in which the drug significantly reduced the risk of new fractures at 18 months in patients with at least one fracture, mild vertebral fractures or two mild vertebral fractures.28 The high cost of treatment could explain a decision to reserve its use for these patients. In contrast, the use of raloxifene and ranelate in the high risk profiles was negligible, although its use is also recommended in these patients.17,27
In conclusion, the definition of OP patients with high risk of fracture in daily practice is not uniform, although the majority of rheumatologists considered the most important factor is a history of previous fragility fractures, followed by treatment with glucocorticoids, advanced age and a low BMD. Early identification of high-risk patients may facilitate the selection of more effective treatments that reduce the risk of future fractures. Among the Spanish rheumatologists, anabolic treatments are the therapeutic option of first choice in patients at high risk of fracture.
Conflict of InterestEnrique Casado, Manuel Caamaño, Jorge Malouf, Enrique Salas, Juan Sánchez-Bursón, Gabriel Herrero-Beaumont have no disclosures to make.
María Luz Rentero belongs to the medical department of Eli Lilly & Co., the company that manufactures teriparatide.
The authors wish to thank Dr. Roy Bheekha who provided medical writing services in representation of InScience Communications, a company of Wolters Kluwer. This work was financed by Lilly.
| 1. Characteristics of the physicianQuestion: Workplace: |
| Hospital |
| Specialty center/peripheral specialty center/outpatient |
| Private practice Response options: All that apply. Question: Years of professional experience in the field. Response options: 0–5; 5–10; 10–15; 15–20; > 20. Question: Autonomous community where you work. Response options: Spanish autonomous communities. |
| 2. Characteristics of clinical activityQuestion: Average number of patients seen per week. Response options: Discrete numeric value. Question: Number of patients with osteoporosis seen per week. Response options: Discrete numeric value. Question: Percentage of patients with primary osteoporosis. Response options: 0%–10%; 11%–20%; 21%–30%; 31%–40%; 41%–50%; 51%–60%; 61%–70%; 71%–80%; 81%–90%; 91%–100%. Question: Percentage of patients from your own practice, from primary care, from orthopedics, from pneumology, from gynecology, from oncology or other departments. Response options: 0%–10%; 11%–20%; 21%–30%; 31%–40%; 41%–50%; 51%–60%; 61%–70%; 71%–80%; 81%–90%; 91%–100%. Question: Of your patients with osteoporosis, What percentage presents osteoporosis and no fracture, single vertebral fracture, multiple vertebral fracture, hip fracture and other fractures? (Total dopes not have to reach 100%). Response options: 0%–10%; 11%–20%; 21%–30%; 31%–40%; 41%–50%; 51%–60%; 61%–70%; 71%–80%; 81%–90%; 91%–100%. |
| 3. Evaluation of the patient/Risk factorsQuestion: According to your opinion evaluate the following risk factors for osteoporotic fracture in relation to the influence they have in therapeutic and/or diagnostic decision making: age, gender, body mass index, height loss, early menopause/hypogonadism, previous fragility fracture, family history of hip fracture, smoking, alcohol consumption, sedentarism/immobility, treatment with oral steroids, treatment with other drugs (antiepileptic, benzodiazepines, antiaromatases, anticoagulants, lithium, thiazides, etc.), tendency to fall, rheumatoid arthritis, BMD, known secondary osteoporosis, low intake of calcium, underexposure to sunlight, others (specify which). Response options: Numeric value from 1 to 5, in relation to the following score: 1. No importance; 2. Little importance; 3. Moderate importance; 4. Very important; 5. Maximum importance. Question: If you had to choose in order the three most important factors to determine what osteoporotic patients have a high risk of fracture, which would they be? Response options: First most important factor to choose among the following: |
| Age, gender, body mass index, height loss, early menopause/hypogonadism, previous fragility fracture, family history of hip fracture, smoking, alcohol consumption, sedentarism/immobility, treatment with oral steroids, treatment with other drugs (antiepileptic, benzodiazepines, antiaromatases, anticoagulants, lithium, thiazides, etc.), tendency to fall, rheumatoid arthritis, BMD, known secondary osteoporosis, low intake of calcium, underexposure to sunlight, others (specify which). Second most important factor to choose among the following: |
| Age, gender, body mass index, height loss, early menopause/hypogonadism, previous fragility fracture, family history of hip fracture, smoking, alcohol consumption, sedentarism/immobility, treatment with oral steroids, treatment with other drugs (antiepileptic, benzodiazepines, antiaromatases, anticoagulants, lithium, thiazides, etc.), tendency to fall, rheumatoid arthritis, BMD, known secondary osteoporosis, low intake of calcium, underexposure to sunlight, others (specify which). Third most important factor to choose among the following: |
| Age, gender, body mass index, height loss, early menopause/hypogonadism, previous fragility fracture, family history of hip fracture, smoking, alcohol consumption, sedentarism/immobility, treatment with oral steroids, treatment with other drugs (antiepileptic, benzodiazepines, antiaromatases, anticoagulants, lithium, thiazides, etc.), tendency to fall, rheumatoid arthritis, BMD, known secondary osteoporosis, low intake of calcium, underexposure to sunlight, others (specify which). Question: In a patient diagnosed with osteoporosis, in your opinion, Which of the following factors supposes a high risk of fracture and involves differences in decision making (therapeutic and/or diagnostic)? |
| That a vertebral fracture is present, that a severe vertebral fracture is present, that a hip fracture is present, that a Colles fracture is present, that multiple fractures are present, that fracture presents in spite of treatment, baseline BMD<−3.5, patient with more than 2 risk factors, increase or appearance of recent pain in the dorsolumbar spine, relevant bone mass loss, loss of more than 2cm of height in the past year, treatment with more than 7.5mg of steroids for a prolonged period, age>70 years, BMI<19, propensity to fall, secondary osteoporosis. Response options: Numeric values 1–5, in relation to the following score: 1. No importance; 2. Little importance; 3. Moderate importance; 4. Very important; 5. Maximum importance. Question: In a patient with osteoporosis presenting incident low back pain, what actions would you carry out? Response options: Among the following, all that apply: |
| None, examination, X-ray, MRI, bone scan, analgesic treatment. Question: Do you examine the spine to detect kyphosis or other deformities? Response options: |
| Yes, in all patients at least in their first visit. |
| Yes, depending on the clinical data. |
| Normally, no. Question: Do you employ fracture risk evaluation scores commonly? Indicate which. Response options: |
| I do not employ them. |
| I employ them. I commonly employ… (The surveyed fill out a space with the tool of their choice). Question: With respect to the FRAX tool: Response options: |
| I do not know it. |
| It is of little use. |
| I use it in some patients when there is diagnostic doubt. |
| I use it in all patients. |
| 4. Diagnostic testQuestion: In a patient with osteoporosis, When would you ask for a lateral spine X-ray? Response options: Among the following, all that apply: |
| Never or almost never. |
| At the moment of the initial visit. |
| If there is dorsal or acute lumbar pain. |
| During follow up. |
| Always. Question: Faced with a morphometric vertebral fracture, what score do you give the following characteristics? |
| Number of fractures. |
| Localization. |
| Recent or old. |
| Degree of deformity. Response options: Numerical value from 1 to 5, in relation to the following scale: 1. No importance; 2. Little importance; 3. Moderate importance; 4. Very important; 5. Maximum importance. Question: Do you perform a bone metabolism analysis in your patients? Response options: |
| No. |
| Yes, for diagnosis. |
| Yes, but only for treatment. Question: If yes, which? Response options: |
| Calcium. |
| Phosphorus. |
| Vitamin D. |
| PTH. |
| Alkaline phosphatase. |
| Protein gram. |
| Bone remodeling markers. |
| Others: ______________ |
| 5. TreatmentQuestion: In the following patient profiles classify the risk of fracture (high, medium, low) of each and mark the treatment that you would indicate as 1st, 2nd and 3rd options: |
| Profile 1: 65-year-old woman presenting vertebral fracture after 5 years of bisphosphonate treatment. |
| Profile 2: 59-year-old woman in treatment with bisphosphonates for 7 years and a T-score of −2.5. |
| Profile 3: 70-year-old woman with no treatment and a T score of −2.8 on the hip and with 2 vertebral fractures. |
| Profile 4: 55-year-old male with a T score of −1.5 treated with 10mg/day of steroids for 1 year. Response options to the classification of the risk for fracture: |
| High. |
| Medium. |
| Low. Response options for 1st choice of treatment: |
| Calcitonin, raloxifene, oral iv biphosphonate, strontium ranelate, PTH (1–84), teriparatide. Response options for 2nd choice of treatment: |
| Calcitonin, raloxifene, oral iv biphosphonate, strontium ranelate, PTH (1–84), teriparatide. Response options for 3rd choice of treatment: |
| Calcitonin, raloxifene, oral iv biphosphonate, strontium ranelate, PTH (1–84), teriparatide. Response options to when do you prescribe the use of calcium and vitamin D? Always. If consumption is low. Never. |
| 6. Conclusion Question: In your experience, Do you consider there is a group of patients at high risk for fracture? Response options: |
| Yes. |
| No. Question: In your daily practice, when a patient is considered as having a high risk for fracture, does this lead to any differences in your conduct? Response options: Among the following, all that apply: |
| No. |
| Yes, I ask for more tests. |
| Yes, I start medical treatment. |
| Yes, I change the treatment. |
| Yes, I start a second drug. |
| Yes, I perform a closer follow up. Question: what do you consider a patient at high risk for fracture? Response option: free text, maximum 200 characters. |
Please cite this article as: Casado E, et al. Manejo del paciente con alto riesgo de fractura en la práctica clínica. Resultados de una encuesta a 174 reumatólogos españoles (proyecto OSTEOPAR). Reumatol Clin. 2011. doi:10.1016/j.reuma.2010.12.008.