The osteonecrosis has emerged in the last years as a potentially disabling osteoarticular complication in HIV-infected patients. There is a high prevalence of traditional risk factors for osteonecrosis development in these patients, but they also have factors associated to HIV infection in itself and the high activity antiretroviral therapy. The HIV-associated osteonecrosis often affects the hips, with a trend to bilaterally, but concomitant affection of 3 or more locations (multifocal osteonecrosis) has been infrequently reported. We present the case of a 49-year-old male patient, with long duration HIV infection and antiretroviral therapy, who developed osteonecrosis with concomitant affection of hips, knees, heels, and tarsus.
La osteonecrosis ha emergido en los últimos años como una complicación osteoarticular potencialmente discapacitante en pacientes con infección por el VIH. Existe una alta prevalencia de factores de riesgo tradicionales para el desarrollo de osteonecrosis en estos pacientes, pero también factores asociados a la infección por VIH en sí misma y el tratamiento antirretroviral de gran actividad. La osteonecrosis asociada a VIH suele afectar con mayor frecuencia a las caderas, con tendencia a la bilateralidad, pero la afección simultánea de 3 o más localizaciones (osteonecrosis multifocal) ha sido descrita de forma infrecuente. Presentamos el caso de un paciente varón de 49 años, con infección por el VIH de largo tiempo de evolución y tratamiento antirretroviral, que desarrolló osteonecrosis con afección simultánea de caderas, rodillas, tobillos y tarsos.
The occurrence of osteonecrosis (ON) was described in patients infected with the human immunodeficiency virus (HIV) for the first time in 19901 and since then there have been several retrospective studies or case-series2 that seem to indicate that its incidence is increasing in these patients. It is estimated that the annual incidence of symptomatic ON in the general population is approximately 0.003–0.006 cases per 100 person-year,3,4 while retrospective studies of HIV-infected patients found an incidence of 0.03–0.65 cases per 100 person-year.5,6 Miller et al.7 reported an even higher prevalence of asymptomatic ON of the hip (4.4%), objectified through magnetic resonance imaging (MRI) in a cohort of 339 patients with HIV infection.
In most published cases of ON in HIV, authors have been able to identify the presence of 1 or more traditional risk factors for its development, especially dyslipidemia, alcoholism, and use of steroids.8 Despite this, there is a large group of patients in which any of these factors can be identified.9 The ratio of HIV infection itself and antiretroviral therapy (HAART) with the development of ON is controversial, and authors have been unable to establish their role as independent risk factors based on current evidence.5,10
The most common HIV-associated ON is that of the hip, with a tendency toward bilateralism in most cases.11 However, its simultaneous presentation in 3 or more locations (multifocal ON) has been reported infrequently.12 We present a patient with HIV infection and HAART who developed multifocal ON with extensive involvement of the hips, knees, ankles, and tarsi.
Case ReportThe patient, a 49-year-old male was a former opiate addict, and had a history of chronic liver disease due to HCV, with no evidence of fibrosis or specific treatment, and presented stage B3 HIV infection (nadir CD4+: 24cells/ml) diagnosed 15 years prior. He had been poorly compliant to treatment, receiving multiple HAART schemes for 10 years, including zidovudine, stavudine, indinavir, efavirenz, didanosine, lopinavir, lamivudine, saquinavir, tenofovir, emtricitabine, ritonavir, and atazanavir. Currently he was treated with combination of abacavir, lamivudine, and darunavir, maintaining an undetectable viral load and CD4+ levels around 500cells/ml. He was hospitalized in March 2010 with pain in the right leg of 2 months duration, affecting the groin, knee, ankle, and forefoot, with an inflammatory rhythm and associated with functional limitation, which had appeared spontaneously, without previous trauma. The physical examination revealed intense pain on right hip mobilization, without presenting local inflammatory signs. Swelling was also found with increased local heat and pain on movement of both knees, ankles, and tarsi. Blood biochemistry showed a severe deficit of 25 (OH) vitamin D3 (3.23ng/ml), without altering the levels of calcium, phosphorus, alkaline phosphatase or parathormone, urinary calcium or tubular reabsorption of phosphate. Hypertriglyceridemia was also detected (364mg/dl) and hypercholesterolemia (374mg/dl). The CBC showed mild normochromic normocytic anemia (Hb 10.3g/dl), without alterations in white cell and platelet counts. The acute phase reactants and immunological tests, including antiphospholipid antibodies were within normal limits or negative. Although the bleeding time was normal, a study of thrombophilia detected an acquired deficiency of antithrombin III (AT-III] (55U/ml). A right knee arthrocentesis was also performed, obtaining a small volume of liquid, mechanical in appearance and with a negative microbiological study.
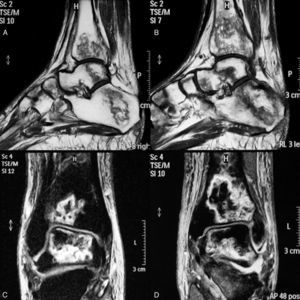
The hip X-ray showed no relevant findings, so we requested a bone scan which showed hypoperfusion of the right femoral head and increased uptake in both ankles suggestive of ON. On MRI we could see multiple bone infarcts of the femoral heads (Fig. 1), proximal regions of both femurs and distal right tibia, astragalus, calcaneus, navicular bone, wedges, cuboid, and metatarsals of both feet (Fig. 2). We indicated a reduction in the weight borne by the lower limbs, but despite this measure the patient developed a major collapse of both femoral heads in a period of 6 months, and is currently awaiting placement of prostheses.
MRI of the ankles and tarsi. In the longitudinal sections of the T1 sequence there are extensive bone infarcts affecting the distal tibia, calcaneus, talus and foot elements, both on the right (A) or left side (B). In coronal sections, the STIR sequence also shows extensive infarcts of the distal region of the tibia and talus, more on the left than the right (D and C, respectively) and joint interline efussion.
Although the incidence of ON in patients with HIV appears to be increased,5 multifocal ON has been reported infrequently, mainly through isolated case reports.12,13 In a Spanish series of 54 HIV-infected patients with associated ON, only 3 cases (5.7%) of multifocal8 ON were described. ON occurs as a result of partial or complete reduction of bone vascularity, having multiple involved mechanisms,14 but the pathophysiology of HIV-associated ON15 remains unknown. Patients infected with HIV have an increased incidence of traditional risk factors for ON, such as steroids, thrombophilia states, alcohol, and smoking, as well as others belonging to HIV, such as duration of infection, nadir CD4+, HAART, abnormal lipid metabolism and lypodystrophia.8 Recently, Mazzotta et al.11 described, in a multicenter study of 26 patients with HIV associated ON, increased serum levels of IgE and prior work disability as additional risk factors.
Our patient had traditional risk factors such as alcoholism, smoking, and a state of acquired thrombophilia (AT-III deficiency). Within the states of thrombophilia associated with HIV, the most common is the presence of antiphospholipid antibodies, but acquired deficiencies of protein C, S, and AT-III, elevated levels of factor VIII and hyperhomocistein15 have been described also. There is a published a case of congenital deficiency of AT-III associated with multifocal16 ON, but not HIV, so this is the first report.
Among the risk factors associated with HIV, our patient had a history of long-term infection, nadir CD4+ low, immunosuppression, and HAART. Various patients had received HAART for a period of 10 years before developing the ON, which differs from the published cases in which the average duration of treatment is 2 years or less.8,12,13 The role of HAART in the appearance of ON remains controversial due to the lack of control groups in the series.8,9 A possible involvement of some antiretrovirals, such as didanosine and stavudine has been suggested, due to induction of mitochondrial dysfunction and lactic acidosis. Protease inhibitors such as lopinavir and ritonavir have also been implicated due to their association with dyslipidemia and lypodistrophia.8
Regarding the distribution of the locations affected in published cases of multifocal ON in HIV, the Spanish series described 3 cases, of which 2 had 4 locations (+ hips knees and hips shoulders +, respectively) and the other, 3 (hips+shoulder).8 There are 2 additional individual cases, 1 published by Akinyoola, which describes a patient with bilateral involvement of shoulders and knees13, and another by Mullan, who describes a patient with 8 affected joints (hips, shoulders, knees, and ankles bilaterally), the latter was the case of HIV-associated ON with the highest number of affected locations 12. In our case, in addition to bilateral involvement of hips, knees, and ankles, there was affection of nearly all skeletal elements of both tarsi, another fact that has not been reported in patients with HIV infection.
ConclusionsON has emerged in recent years as a potentially disabling osteoarticular complication in HIV patients receiving HAART. This has led a growing interest in early diagnosis and identification of risk factors, both traditional and associated to HIV. It is important to consider the possibility of ON in HIV patients who complain of pain in large joints, especially with a trend towards bilateralism. Although a rare presentation, this condition may be multifocal, so a thorough examination should be performed to identify other affected locations, including imaging tests, such as scintigraphy and MRI.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestThe authors declare no conflict of interest.
Please cite this article as: González García A, et al. Osteonecrosis multifocal asociada a infección por el virus de la inmunodeficiencia humana. Reumatol Clin. 2012;8:361–4.