To describe the frequency and profile of patients with neuro-Behçet’s disease (NBD) at the Central University Hospital of Asturias between 1981 and June 2018.
Patients and methodsRetrospective study including epidemiological, clinical, neuroimaging, cerebrospinal fluid (CSF) study, histopathology, treatment and evolution characteristics. Clinical characteristics are differentiated between patients with Behçet without neurological affectation and NBD.
ResultsWe found 10 cases of NBD (25.6%). The mean age was 29.7 years, and it was more frequent in males. Sixty percent had parenchymal involvement. The non-parenchymal involvement included a case with cerebral venous thrombosis and two cases with isolated aseptic meningitis. Findings of vasculitis were found on cerebral magnetic resonance imaging, and alteration in the biochemistry of the CSF. One patient presented a striking motor disability. Ocular involvement was greater in the group of patients without neurological involvement (P = .009).
ConclusionsNBD is a relatively frequent presentation, especially in males and in the parenchymal form. We did not find a systemic clinical marker of neurological involvement.
Describir frecuencia y perfil de pacientes con neuro-Behçet (NB) del Hospital Universitario Central de Asturias desde 1981 hasta junio del 2018.
Pacientes y métodosEstudio retrospectivo que incluye características: epidemiológicas, clínicas, neuroimagen, estudio de líquido cefalorraquídeo (LCR), histopatología, tratamiento y evolución. Se diferencian características clínicas entre pacientes con Behçet sin afectación neurológica y NB.
ResultadosSe describen 10 casos de NB (25,6%). La edad media a su diagnóstico: 29,7 años, siendo más frecuente en varones. El 60% tienen afectación parenquimatosa. En la afectación no parenquimatosa se incluyen un caso con trombosis venosa cerebral y dos con meningitis aséptica aislada. Se encontraron hallazgos de vasculitis en la Resonancia Magnética Cerebral, y alteración en la bioquímica del LCR. Un paciente presentó discapacidad motora llamativa. La afectación ocular ha sido mayor en el grupo de los pacientes sin afectación neurológica (p = 0,009).
ConclusionesEl NB es relativamente frecuente, sobre todo en varones y en la forma parenquimatosa. No se encuentra un marcador clínico propio de la afectación neurológica.
The neurological manifestations in Behçet's disease (BS) are much less frequent than the more typical manifestations but can be particularly serious, causing long-term morbidity and mortality.1,2
Diagnosis of neuro-Behçet’s disease (NB) involves findings of systemic BD along with the presence of otherwise unexplained neurological symptoms.3 Unfortunately, there is no specific diagnostic test for NB. Diagnosis of the disease requires a high rate of clinical suspicion1,3 which, together with complementary test findings, form the keys to its diagnosis, therapeutic orientation and prognosis,4 which justified undertaking this study.
The aim of our study was to describe the frequency, epidemiological and clinical characteristics, complementary test findings and to compare the clinical characteristics of patients with BD without neurological involvement with those of patients with NB registered up to June 2018 in the Central University Hospital of Asturias (HUCA).
Material and methodsWe conducted a retrospective review of the register of patients diagnosed with BD in the Autoimmune Diseases Unit of HUCA’s Internal Medicine Service, which includes both sexes, over a period of 37 years (1981-June 2018). All patients met the international study group criteria for BD.5
From these patients, we selected those with neurological findings suggestive of nervous system involvement in BD, reviewed epidemiological and clinical characteristics, complementary test findings - neuroimaging, cerebrospinal fluid (CSF), histopathological findings- and treatment and progression.
Patients with headache or vague symptoms such as dizziness, those who showed no abnormality on neurological examination, imaging or CSF studies, and patients who took drugs or presented semiology of other diseases that could potentially induce neurological disturbance were excluded.
Neuroimaging consisted of a cerebral magnetic resonance study (MRI). Depending on the location of the lesions in the central nervous system, two main patterns were distinguished: parenchymal form and non-parenchymal or vascular form.1,3 In parenchymal involvement we include brain stem syndromes, "brain stem plus", brain and spinal cord syndromes. Cerebral venous thrombosis, intracranial aneurysm and extracranial aneurysm/dissection were included in the non-parenchymal form. The presence of isolated aseptic meningitis was considered non-parenchymal.
Clinical features (ocular lesions, skin lesions, erythema nodosum, deep vein thrombosis (DVT), arterial thrombosis, arterial aneurysm and digestive involvement) were compared between patients with BD without neurological involvement and those with neurological involvement.
The data were recorded and analysed using the Statistical Package for the Social Sciences (SPSS) version 23. The qualitative variables were summarised by their frequency distribution, the quantitative variables by mean and standard deviation or median and interquartile range. The chi-square test was used for comparisons between NB and non-NB and for the qualitative variables, and the Mann-Whitney U and Student’s t-test for the quantitative variables. A P < .05 was considered statistically significant.
The research protocol was approved by HUCA’s Ethics and Clinical Research Committee.
ResultsThe medical records of 39 patients with BD were reviewed: 20 males and 19 females (M/F = 1.05). The mean age at diagnosis of BD was 31.8 ± 13.9 years and the time from onset of BD manifestations and diagnosis was 1.5 years (IQR: .5–4.2 years).
Neurological involvement was observed in 10 patients (25.6%): 6 males and 4 females (M/F = 1.5). The mean age at diagnosis of NB was 29.7 ± 12.1 years. The time between onset of BD manifestations and neurological manifestations was 3 years (IQR: .7–10.5 years). The follow-up time from diagnosis of NB was 7.5 years (IQR: 4–11 years).
Of the 10 patients with NB, 60% presented parenchymal involvement and 70% different types of lesions on MRI.
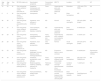
Table 1 shows the clinical characteristics and imaging, CSF and histopathological findings of the patients with NB.
Clinical, imaging, cerebrospinal fluid and anatomopathological characteristics of patients with neuro-Behçet’s disease.
| Age BD | Age BD | Sex | BD ISG criteria (n) | Neurological symptoms | Concomitant symptoms | MRI T2 | Location | CSF | AP |
|---|---|---|---|---|---|---|---|---|---|
| 19 | 22 | M | Oral and genital ulcers, posterior uveitis, folliculitis (4) | Headache, hemiparesis and hemianaesthesia, neck stiffness | Fever | Hyperintensity pons and cerebellar peduncle | Brainstem | 1376 cells (75% PMN) | NA |
| 6 | 6 | M | Oral and genital ulcers, acneiform nodules (3) | Hemiparesis | Acne | ND | Brain hemisphere | ND | NA |
| 36 | 36 | F | Oral and genital ulcers, pseudofolliculitis (3) | Headache, neck stiffness in childhood | ND | Normal | Acute meningitis | 350 cells (98% lymph) | NA |
| 37 | 37 | F | Oral and genital ulcers, bilateral anterior uveitis (3) | Facial paralysis, hemiparesis, diplopia, instability | ND | Hyperintensity pons and cerebellar peduncle | Brain hemisphere | 0 cells20 prot | NA |
| 29 | 29 | M | Oral and genital ulcers, pseudofolliculitis (3) | Hemiparesis, hemiparaesthesia, instability | Fever, arthritis, skin lesions | Hyperintensity pons, midbrain and cerebellar peduncles | Brainstem | 0 cells91 prot | NA |
| 26 | 28 | M | Oral and genital ulcers, folliculitis, erythema nodosum (4) | Headache, neck stiffness, photophobia | Oral aphtha | Normal | Acute meningitis | 204 cells (97% lymph) | NA |
| 53 | 53 | M | Oral and genital ulcers, pustulosis (3) | Dysphonia, dysphagia, hiccups, diplopia, ptosis, hemihypoaesthesia | ND | Expansive lesion in pons and bulb | Brainstem | 0 cells48 prot | Perivascular inflammatory infiltrate |
| 34 | 34 | F | Oral and genital ulcers, retinal vasculitis (3) | Headache, photophobia, neck stiffness | Fever, aphtha | Hyperintensity bilateral frontal white matter | Brain hemisphere | 350 cells (73% PMN)60 prot | NA |
| 27 | 27 | M | Oral and genital ulcers, positive pathergy test (3) | Bilateral papillary oedema, instability, reduced VA, headache | Febricula, otalgia | Transverse and right sphenoparietal sinus thrombosis | Cerebral venous thrombosis | 1 cell23 prot | NA |
| 17 | 25 | F | Oral and genital ulcers, bilateral anterior uveitis, pustulosis (4) | Hand paraesthesia, bilateral optic neuritis | ND | Periventricular and left temporal lobe hyperintensity, cervical plate | Brain hemisphere, medulla | 0 cellsOligoclonal bands | NA |
AP: Anatomopathology; BD: Behçet’s disease; CSF: Cerebrospinal fluid; F: Female; ISG BD: International Study Group criteria for Behçet’s disease; lymph: lymphocytes; M: Male; MRI: cerebral magnetic resonance imaging; NA: Not applicable; NB: Neuro-Behçet’s; ND: Not described; PMN: Polymorphonuclears; prot: proteins (mg/dl); VA: visual acuity.
Three patients were observed to have had brainstem involvement, three hemisphere involvement and one spinal cord and hemisphere involvement.
In parenchymal involvement the most common clinical forms of presentation were hemiparesis (40%), paraesthesia (40%), instability (30%) and diplopia (20%). In the "non-parenchymal" form, we found one case with cerebral venous thrombosis due to transverse sinus involvement, with clinical semiology of intracranial hypertension.
Meningeal involvement was detected in 40% of the cases of NB and in 20% as isolated aseptic meningitis.
The most common symptom of the patients with NB was headache (50%); fever was associated in up to 40%.
The results of CSF analysis of 9 patients showed complete normality in 22.2%, pleocytosis in 44.4%, and elevated protein in 33.3%. Glucose levels were normal in all cases. CSF opening pressure increased (more than 20 cmH2O) in the patient with intracranial hypertension.
The comparison between patients with BD without neurological involvement and those with NB in its different clinical aspects is shown in Table 2.
Comparison of clinical characteristics between patients with Behçet’s disease without neurological involvement and neuro-Behçet’s.
| Characteristics | Behçet’s, n = 29 | Neuro-Behçet’s, n = 10 | Total, n = 39 | P |
|---|---|---|---|---|
| Age at DX BD (age ± SD) | 32 ± 14 | 29.7 ± 12.1 | .54 | |
| Time from clinical onset to DX DB, years (IQR) | 1 (.4−4) | 3.5 (.8−9) | .23 | |
| Male | 13 (44.8%) | 6 (60%) | 19 | .685 |
| Ocular lesions | 15 (51.7%) | 5 (50%) | 20 | .009 |
| Skin lesions | 16 (55.2%) | 5 (50%) | 21 | .08 |
| EN | 8 (27.6%) | 2 (20%) | 10 | .22 |
| DVT | 3 (10.3%) | 3 (30%) | 6 | 2.2 |
| Digestive involvement | 3 (10.3%) | 3 (30%) | 6 | 2.2 |
| Arterial thrombosis | 0 (0%) | 2 (20%) | 2 | 6.1 |
DVT: Deep vein thrombosis; DX BD: Diagnosis of Behçet’s disease; EN: Erythema nodosum; IQR: Interquartile range; SD: Standard Deviation.
Neurological involvement in patients diagnosed with BD in our series, which only includes patients diagnosed and followed up in the Autoimmune Diseases Unit attached to HUCA’s Internal Medicine Service, was 25.6%; in other series it ranges from 10% to 29%. The differences can be attributed to ethnic, geographic, methodological or study type variability. NB is more frequent in males (M/F = 1.5); other studies have shown ratios of 1.3–1.8,4,6,8 similar to that found in our study.
Neurological symptoms usually begin after the diagnosis of BD has been established.1 In our series, the neurological manifestations preceded the diagnosis of BD in one patient.
The mean age and the time between neurological manifestations and diagnosis of BD are similar to those found in other studies.4,6,8
Parenchymal involvement (brainstem and brain hemispheres) was more common in our study, as in most other series.4,6–9
Ischaemic stroke is rare in BD (1%-5% according to descriptions) and is considered parenchymal involvement. In our study one patient presented right hemispheric ischaemic stroke and right internal carotid obstruction.
One of our patients had a unique form of presentation, a "pseudotumour" or "tumour like" form, located in the brainstem; on the MRI it was described as a mass effect with contrast uptake with annular enhancement, a situation already observed in one case in the series by Matsuo et al.10 Most cases were diagnosed after biopsy of the lesion, as in our case, and partially responded to steroid treatment.1 Our patient debuted with progressive bulbar syndrome; after treatment with steroids, imaging controls showed a significant decrease in the size of the lesion.
Thrombophilic status resulting in arterial (pulmonary artery) and venous (peripheral and cerebral) thrombotic episodes is often underlying in patients with BD.1,11 Other series describe venous sinus thrombosis (VST) between 5% and 10%.1,12 Several types of vascular manifestations tend to occur in the same individual, creating statistically significant associations in all patients; for example, cerebral VST and pulmonary artery involvement, which tend to coexist.13 In our series, one patient presented thrombosis in the transverse and sphenoparietal sinus on MRI, and at their two-year follow-up presented bilateral pulmonary arterial thrombosis only attributable to BD.
Lower limb vein-thrombosis (superficial and deep) is the most common form of vascular involvement in BD.13 In our series, one patient with brainstem involvement presented bilateral iliofemoral DVT, and the two patients with isolated aseptic meningitis presented right subclavian/axillary DVT and left popliteal DVT, respectively, with no statistically significant difference between vascular involvement and NB.
NB can sometimes present in a similar way to multiple sclerosis, with very similar MRI findings;1,9,14 these patients are usually women, with a higher frequency of neurological recurrences, presence of oligoclonal bands and less pleocytosis.13,15 One of our cases, 7 years following diagnosis of BD, showed vasculitis lesions, considered non-specific, on MRI, and oligoclonal bands in CSF; years later he was to develop bilateral optic neuritis, but he was included as NB in follow-up, since in addition to meeting all the criteria of the 1990 international study group, he did not present Barkhof criteria, which define progression to multiple sclerosis determined by MRI study, but as IL-6 or other cytokines in CSF could not be determined, the coexistence of the two diseases cannot be excluded.
In the comparative analysis of the clinical characteristics between BD without neurological involvement and NB no significant differences were found, except for ocular involvement, which was significantly greater in the group without neurological involvement. In relation to inflammatory ocular involvement, which could present usual BD semiology, we find it of interest to mention that no other cases of ophthalmological involvement were observed in this series. However, we have documented cases with active follow up that have progressed to very aggressive HLA B51+ panuveitis and retinal vasculitis, without fulfilling the clinical criteria for BD to date. There are some comparative studies between BD without neurological involvement and NB, such as the study in Tunisia,8 which showed that patients with NB presented more frequently with DVT and arterial aneurysm (P < .001 and P = .04, respectively), and in a Portuguese study,7 the frequency of gastrointestinal and vascular involvement was higher in the NB group (P = .035 and P = .027, respectively). We did not analyse for the presence of arterial aneurysm as none presented in either of the groups (Table 3).
Demographic characteristics and presentation pattern in patients with neuro-Behçet’s.
| Riera-Mestre,4 2010 | Peño,6 2012 | Houman,8 2013 | Domingos,7 2015 | Our study | |
|---|---|---|---|---|---|
| Country | Spain | Spain | Tunisia | Portugal | Spain |
| Number of patients | 20 | 7 | 121 | 25 | 10 |
| Male | 13 | 3 | 78 | 10 | 6 |
| Female | 7 | 4 | 43 | 15 | 4 |
| Age at presentation, years | 36.3 | 29.0 | 29.7 | 37.5 | 29.7 |
| P-NB | 16 | 4 | 74 | 15 | 6 |
| NP-NB | 4 | 3 | 35 | 2 | 3 |
| CSF abnormality | 16/18 | ― | 29/40 | 15/20 | 7/9 |
| MRI abnormality | 18/19 | 6/7 | 74/92 | 15/23 | 7/9 |
CSF: Cerebrospinal fluid; MRI: Cerebral magnetic resonance imaging; NP-NB: Non-parenchymal form of neuro-Behçet’s; P-NB: Parenchymal form of neuro-Behçet’s.
Treatment in our series, in the parenchymal forms, consisted of methylprednisolone pulses of 500 mg in all patients, followed by cyclophosphamide at doses of 500−750 mg/monthly for 6 months, and oral steroids from 1 mg/kg in a descending regimen, and finally followed by azathioprine (100−150 mg/day) as maintenance; in one case alone with this condition, infliximab was prescribed at doses of 5 mg/kg every 2 weeks for 2 years, and cyclosporine was avoided at all times, due to its known neurotoxicity.
In forms with vascular involvement, anticoagulation was initiated for 6 months and later treatment with azathioprine (100−150 mg/day) for 3 years.
We are not aware of any deaths with these measures, nor have there been any infectious complications. The patient with the pseudotumour form of presentation is the only patient in our series with striking motor disability, defined by a score on the Modified Rankin Scale of 4. One patient with the parenchymal form presented dysaesthesia in the left hemiface as a sequela; the rest of the patients had no significant sequelae.
The retrospective nature of our study and the small number of patients included are its main limitations.
ConclusionsNB is a relatively frequent presentation within a minority and rare disease, it predominates in males with parenchymal involvement: brainstem and hemisphere. Its main clinical manifestations are hemiparesis and paraesthesia, with vasculitis lesions on MRI and abnormal CSF. A certain prevalence of meningeal involvement should be highlighted. Immunosuppressants were used in the treatment of NB: steroids, cyclophosphamide, azathioprine, and in one case an anti-TNF was required. There were no deaths, and one patient had a striking motor disability. Ocular lesions were more frequent in the BD group without neurological involvement, and in our series, we found no systemic clinical marker specific to neurological involvement in BD.
FundingThis research study has received no specific support from public sector agencies, commercial sector or non-profit entities, or grants of any kind.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Charca-Benavente LC, Gómez de la Torre R, Caminal-Montero L, Coto-Hernández R, Colunga-Argüelles D. Enfermedad de neuro-Behçet en el Hospital Universitario Central de Asturias. Reumatol Clin. 2021;17:32–36.