Neck pain is a common reason for seeking medical attention. It affects at least 15% of the labor force and up to 40% of individuals whose occupation is hazardous. On the other hand, primary bone lymphoma is a very rare disease (less than 1% of all malignant bone tumors), and the relationship between the 2 has rarely been mentioned. We report the case of a patient who had a 1-month history of neck pain. The main symptom was pain on palpation of C2–C6 cervical spinous processes and contracture of the trapezius muscle that did not cease with conventional treatment. Imaging studies indicated an abnormality. He underwent surgery and the results of vertebral biopsy were compatible with diffuse large B-cell lymphoma. He was treated with radiotherapy with a good outcome.
La cervicalgia es un motivo de consulta muy frecuente en la consulta médica. Se sabe que al menos un 15% de la población activa y hasta el 40% de los profesionales de riesgo la presentan. Por otro lado, el linfoma óseo primario es una patología muy poco frecuente (menos del 1% de todos los tumores óseos malignos) y la asociación entre ambos ha sido pocas veces descrita. Presentamos el caso clínico de un paciente con clínica compatible con cervicalgia de un mes de evolución, que al examen físico destacaba dolor a la palpación de apófisis espinosas C2-C6 y contractura trapezoidal que no cedía con tratamiento habitual. Posterior a estudios de imagen patológicos, se interviene quirúrgicamente realizando exéresis de cuerpo vertebral C4 y masa tumoral epidural anterior más biopsia compatible con linfoma difuso de células grandes B. Buena evolución al tratamiento quirúrgico y radioterapia.
Cervicalgia is the pain located between the occipital region and the line that passes through the spinous process of T1. It is a very common symptom in the general population; up to 70%–80% of the adult population can present it at some time in life and, among the musculoskeletal manifestations, it is situated in third place, only after low back pain and backache.1 Bone and medullary tumors, despite their rare incidence, are among the causes of infrequent, nontraumatic neck pain. Primary bone lymphoma (PBL), is an uncommon disease that represents between 0.98% and 5% of all malignant bone tumors. In all, 95% of them correspond to B-cell non-Hodgkin lymphomas (NHL). Bone involvement occupies the sixth place among extranodal sites, after the gastrointestinal tract, skin, central nervous system, lung and salivary gland.2,3
Age at the onset of disease can range from 2 years to up to 86 years, with a mean age of 48 years; the peak of incidence is between 60 and 70 years, and it is more common among men than in women.4 We present the case report of a patient who began with signs of atypical neck pain with stiffness and limited neck rotation due to infiltration of bone and medulla by a B-cell NHL.
The diagnostic suspicion, early detection and interdisciplinary treatment can result in a better prognosis, as occurred in our patient.
Case ReportThe patient was a 73-year-old man, with a history of adenocarcinoma of the prostate. He had undergone radical surgery 10 years ago and had a pacemaker placed 3 years earlier due to bradycardia–tachycardia syndrome. One month before his first visit to the rheumatology department, he began to feel progressive pain, that went from moderate to severe, in the cervical spine and shoulder girdle; it was not radiating. It was associated with progressive hyperkyphosis, that at the time of the visit was practically intractable. In the initial physical examination, we detected pain in response to digital pressure of the spinous processes from C3 to C7, limitation of mobility in flexion extension of the cervical spine, practically intractable due to pain and contraction of the trapezius muscles. While waiting for the results of the tests requested, treatment was begun with nonsteroidal anti-inflammatory drugs and muscle relaxants, although with little improvement. The radiograph of the cervical column revealed degenerative signs and slight radiolucency of the C4 vertebral body. Magnetic resonance (MR) of the cervical spine showed the image of a mass from C2 to C6, with infiltration of the foramina and peridural space in segment C3–C5 and compression of the medullary cord (Fig. 1).
Thoracoabdominal computed tomography (CT) showed right diaphragmatic paralysis and secondary right subsegmental atelectasis. There was a fibrotic lesion in left inferior lobe. Computed tomography of the neck demonstrated involvement of the cervical spine from C3 to C5, with no clear signs of bone destruction. Expansive component of soft tissues with foramina. Blood tests (complete blood count, laboratory tests and tumor markers) and bone marrow aspirate were normal.
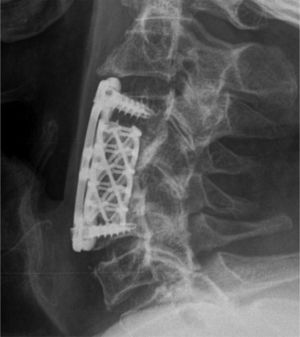
The patient was admitted to the hematology department, where he began treatment with dexamethasone at 15mg/day, with a clinically significant improvement in the pain, although not of the stiffness of his cervical spine. Surgical intervention was subsequently performed with resection of the affected C4 vertebral body, prior resection of the epidural tumor, plus fixation with titanium mesh filled with a bone inducer and C3 to C5 anterior cervical plate (Fig. 2). During the immediate postoperative period he developed atrial fibrillation, with rapid ventricular response. The results of the vertebral biopsy, performed in the pathology department of University Hospital Arnau de Vilanova, were as follows: under microscopy, among the remitted fragments, there were large areas of necrosis, together with small foci with a proliferation of lymphoid elements with a generally small nuclei; however, occasionally, there were also large nuclei. Immunohistochemistry studies showed CD20 and Ki67, compatible with a diagnosis of diffuse large B-cell lymphoma.
A study of the extension was performed, and was negative. The diagnosis was primary bone diffuse large B-cell NHL, limited only by the cervical spine. It was decided to treat the patient with radiotherapy for 4 months. Ten months later, after the initiation of adjuvant therapy, positron emission tomography (PET)-CT was performed, and found no evidence of disease. After 5 years of follow-up, the patient is in complete remission.
DiscussionBone lymphoma is a very infrequent tumor; it represents between 0.98% and 5% of all the primary bone tumors. It was described for the first time in 1928 by Oberling. It is most often diagnosed in patients over the age of 30 years, with a peak incidence between the sixth and seventh decade, with a slight predilection for men.2,5 To be described as a PBL, it is necessary that there be histopathologically confirmed lymphomatous bone involvement, with no evidence of nodal or extranodal disease at another site for 6 months after the diagnosis,6 criteria that our patient fulfilled. Ostrowski et al., in1986, subclassified PBL into 4 groups7; group 1 represented solitary primary bone lymphomas.
The clinical signs are usually nonspecific, as bone pain is insidious and discontinuous, and does not improve with inactivity. It is the most frequent clinical symptom and it seldom presents as asymptomatic. It can be accompanied by a palpable mass, constitutional symptoms and, if vertebral involvement exists, there can be radicular symptoms and medullary compression. The most frequent locations are the metaphyses and diaphyses of the long bones (70%), with the femur, tibia, humerus and the clavicle being the habitual sites.8 Our patient showed the clinical signs of severe neck pain that had begun a month ago, and had spread to the shoulder girdle with progressive hyperkyphosis that was taken to be intractable. We have not found this same presentation in any other clinical description.
In histological terms, the majority of PBL are in the line of diffuse large B-cell lymphoma of the subtype NHL, like that presented by our patient. Only 10% are T-cell lymphomas and primary bone Hodgkin's disease is still much more uncommon.
To diagnose PBL, it is necessary to have a high index of suspicion based on a complete clinical history and laboratory tests, although imaging studies are what actually suggest the tumor.9 Plain radiographs can demonstrate bone lesions with a lytic pattern even in advanced phases. Computed tomography is what best defines the lesion, but it is MR with hypointense images in T1 and hyperintense in T2 where the lesion can be characterized. Positron emission tomography is widely utilized for staging and to follow changes in the lesion.
The definitive diagnosis is based on the pathological study of the biopsy specimen. The age and clinical manifestations of the patient we present made us initially suspect the possibility of bone metastasis as, years before, he had been diagnosed with prostate adenocarcinoma. However, the study of the biopsy made it clear that the diagnosis was PBL.
Primary bone NHL requires treatment as early as possible, with a multidisciplinary view. The majority of the therapeutic regimens include chemotherapy and radiotherapy, reserving surgery for very specific cases.3,10 The patient we present was treated with radical surgery with resection of the tumor and anterior epidural plus cervical fixation. Once the type of the tumor was known, as was its classification and extension limited exclusively by bone in the cervical spine, we decided to continue with local radiotherapy with a mean dose of 40Gy. To evaluate the response to treatment, we performed serial PET, a modality that is seen to be the technique most widely utilized for staging and the evaluation of the therapeutic response of PBL, and in the case of the patient we report, 5 years after the diagnosis, he shows no lesion indicative of activity.
In short, in the presence of an atypical neck pain, it is necessary to accompany the etiological study with ancillary tests, given the possibility of an inflammatory or neoplastic disease. Primary bone NHL is considered an uncommon tumor, and its clinical manifestations are imprecise. It should be included in the differential diagnosis of constant bone pain in individuals ranging in age from 60 to 70 years. Early diagnosis improves the prognosis as it makes it possible to apply better types of treatment, like radical surgery.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Rojas N, Fernandes C, Conde M, Montala N, Fornos X, Rosselló L, et al. Linfoma no Hodgkin y cervicalgia atípica. A propósito de un caso. Reumatol Clin. 2019;15:e44–e46.