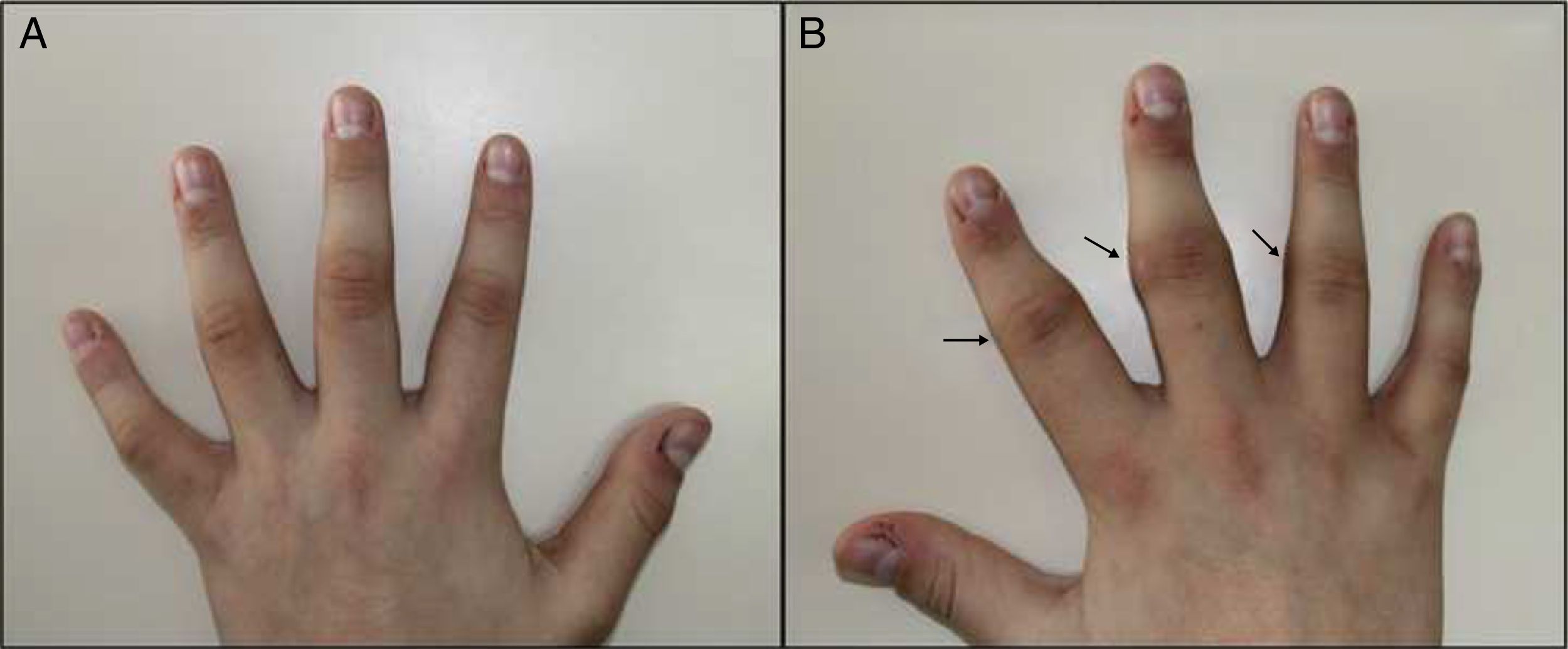
A 14-year-old male, with no history of interest, consulting with a year's history of deformity and symmetrical pattern swelling on the lateral face of the proximal interphalangeal joints (IPJ) of the second, third and fourth fingers, with predominance in the right hand (Fig. 1A and B). He reported no pain, limitation or other associated skin or systemic manifestations.
Analysis, which included complete blood count, biochemistry, coagulation, erythrocyte sedimentation rate, C reactive protein, HLA-B27, rheumatoid factor and antinuclear antibodies, was normal or negative. Plain X-ray showed an increase in soft tissue on the second, third and fourth IPJ of the right hand, with no signs of associated joint or bone involvement (Fig. 2). Magnetic resonance imaging showed oedema and increased soft tissue on the second, third and fourth fingers of the right hand. There were no signs of synovitis or associated collections (Fig. 3). A skin biopsy was performed that revealed compact hyperkeratosis and thickening of the dermis, with an increase in the number of collagen fibres and fibroblasts.
This led to a diagnosis of classical pachydermodactyly; given the benign nature of this entity and the absence of associated clinical symptoms a wait-and-see approach was decided. After 18 months of six-monthly follow-up in the paediatric dermatology and rheumatology clinic, the patient remains asymptomatic, without pain, functional limitation or other associated clinical manifestations.
DiscussionPaquidermodactyly, initially described in 19731 and later in 1975,2 is an acquired and under-diagnosed form of digital fibromatosis, of benign course and predominantly affects young males. It is characterised by the presence of progressive, asymptomatic and bilateral swelling of the IP joints of both hands.1–3 The cause is unknown, although the possible implication of repeated micro trauma, genetic and hormonal factors has been postulated.4,5 Diagnosis of this entity is essentially clinical, and must be differentiated from juvenile idiopathic arthritis, with characteristic clinical, analytical and radiological findings.4–6 Clinical treatment measures are preferred, although intralesional glucocorticoids could be used, and surgery as an alternative in some subgroups of patients.3–6
Ethical responsibilitiesProtection of people and animalsThe authors declare that neither human nor animal testing has been carried out under this research.
Data confidentialityThe authors declare that they have complied with their work centre protocols for the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article. This document is held by the corresponding author.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Agudo-Mena JL, Buedo-Rubio MI, García-Atienza EM, Escario-Travesedo E. Paquidermodactilia: la gran simuladora. Reumatol Clin. 2019;15:e156–e157.