To analyse the current needs of patients with spondyloarthritis (SpA) and psoriatic arthritis (PsA), and the impact of the conditions.
MethodsNational survey in electronic format for patients with SpA and PsA. The survey was launched on April 28, 2021, using the channels of the Coordinadora Española de Asociaciones de Espondiloartritis (Spanish Coordinator of Associations of Spondyloarthritis) to communicate with members and followers, and was closed on June 30, 2021. Sociodemographic and clinical variables were collected (age, sex, disease duration, treatments), and variables related to the objectives. A descriptive analysis was performed.
ResultsA total of 543 patients with SpA and 291 with PsA were included. In the previous month, on a scale from 0 to 10 (0: none; 10: very high) the mean scores of fatigue, morning stiffness, and sleep problems were all >8. Almost 80% of the patients with SpA reported low back pain and 82.5% of the patients with PsA reported involvement of the knees, ankles, feet and/or hands, and 51% dactylitis. The level of satisfaction with the treatment was low, mean 5.5 in SpA and 6.2 in PsA (scale 0–10). It was higher with biological therapies. We found that 70.2% of patients with SpA and 66% with PsA were used to living with pain every day. Finally, 43.8% of participants with SpA and 31.2% of those with PsA reported that they did not set the treatment goals with their doctors.
ConclusionsCurrently the impact of SpA and PsA on multiple aspects of daily life is still very high. There are areas for improvement in the doctor-patient relationship and in treatments.
Analizar las necesidades, el impacto y la perspectiva actual de las personas con espondiloartritis (EspA) incluyendo la artritis psoriásica (APs).
MétodosEncuesta nacional en formato electrónico dirigida a pacientes con EspA y APs. Se abrió en abril de 2021 utilizando los distintos canales de la Coordinadora Española de Asociaciones de Espondiloartritis para comunicarse con sus socios, y se cerró en junio de 2021. Se recogieron variables sociodemográficas y clínicas, y variables relacionadas con los objetivos propuestos. Se realizó un análisis descriptivo.
ResultadosSe incluyeron 834 pacientes: 543 con EspA (sin APs) y 291 con APs. En el último mes, la media de fatiga, rigidez matutina y problemas de sueño fue >8 (0: nada; 10: mucho). Casi el 80% de los pacientes con EspA refieren dolor lumbar bajo, y el 82,5% de los pacientes con APs, afectación de rodillas, tobillos, pies y/o manos, y el 51%, dactilitis. El grado de satisfacción con el tratamiento fue medio-bajo: media 5,5 en las EspA y 6,2 en la APs (escala 0–10), y más alto con las terapias biológicas (medias>6–7). El 70,2% de los pacientes con EspA y el 66% con APs se han acostumbrado a vivir con dolor diario. El 43,8% de los encuestados con EspA y el 31,2% con APs refieren que no marcan los objetivos del tratamiento con el médico.
ConclusionesActualmente el impacto de la EspA y de la APs en múltiples aspectos del día a día sigue siendo muy alto. Existen áreas de mejora en la relación médico-paciente y con los tratamientos.
Spondyloarthritis (SpA) comprises a group of immune-mediated diseases that share a number of clinical symptoms, pathological mechanisms, and treatment response1–3. In Europe, SpA has an estimated prevalence of .3% and 1.8%, which indicates that that there could be half a million patients with SpA in Spain4. Ankylosing spondylitis (AS) and psoriatic arthritis (PsA) are the most common of the SpAs. These are also diseases with major impact on patients’ quality of life, their families, and healthcare systems5.
In recent years we have witnessed a paradigm shift in the management of this group of diseases, based, among others, on advances in imaging techniques, the use of innovative therapies, and a more systematised and comprehensive approach to patients6. This has led to improvements in many parameters, such as mortality and quality of life in SpA, including PsA7. However, there remain unresolved or uncovered issues that require further work8. These include, for example, the identification and management of fatigue, pain, sleep disorders, or work-related problems9,10.
In addition, there has been increased patient involvement in decision-making about their health and disease in recent years. It is therefore essential to consider the patient's perspective regarding their experience, concerns, goals, and expectations with their disease and other aspects such as work9. It has recently become clear that in patients with PsA, the disease often dictates the course of their lives, disrupting family and social roles, and causing them significant limitations due to debilitating and far-reaching symptoms such as fatigue9. Many patients are also demoralised by the ineffectiveness of treatments, and others are disappointed by unmet expectations relating to the benefit of treatments9.
Despite the relevance of up-to-date data on the impact and opinion of patients in relation to SpA, including PsA, and their treatments, there is currently little information available in Spain. The ATLAS project survey conducted in 2016 in patients with axial SpA noted the delay in the diagnosis of the disease, and its great impact on patients (physical, psychological, social, occupational, etc.)11. A small qualitative study recently highlighted the ongoing difficulties in reaching a diagnosis of axial SpA and the personal, social, and occupational impact of the disease8, and another published in 2018 exposes the multiple information needs of patients with SpA, including PsA. Other studies outside Spain have also highlighted this situation in patients with this group of diseases12–14.
It is for all these reasons that the CEADE (Spanish Coordination of Spondyloarthritis Associations) proposed conducting a survey to determine the current status on the impact on patients’ quality of life, and expectations and concerns, the doctor-patient relationship, and the sources of information used15. Furthermore, there is no evidence to compare the patient's perspective with that of the rheumatologist, which would enable us to identify areas for improvement in communication between the two that we can work on in the future12.
MethodsThis work was promoted by CEADE, the Spanish Coordination of Spondyloarthritis Associations (www.eaceade.es). A survey was conducted in full compliance with the principles set out in the latest version of the Declaration of Helsinki, concerning medical research involving human subjects; and in accordance with the applicable regulations on good clinical practice. The main objective of this survey was to understand the needs and current impact of people with SpA and PsA in Spain.
Design, survey launch, and data acquisitionA cross-sectional study was conducted by means of an online survey in electronic format (no other formats such as paper were used) aimed at patients with SpA including PsA (**see supplementary material). First, a multidisciplinary working group consisting of a rheumatologist and two patient members of CEADE was created who designed the survey with methodological assistance. Previously published patient surveys16 were evaluated in its design. The survey was generated via the Internet (SurveyMonkey® software), following a closed and structured questionnaire.
The survey included the following sections and variables:
- 1
Sociodemographic data (age, sex, autonomous community of residence).
- 2
Clinical characteristics of SpA or PsA (type of involvement, time to diagnosis, diagnosing specialist, and physician in charge).
- 3
Disease activity (fatigue, pain, arthritis, morning stiffness, sleep problems, affected areas, symptoms in the last month, loss of mobility).
- 4
Impact on quality of life (activities of daily living, work).
- 5
Treatment including type, anti-inflammatory and analgesic drugs, traditional non-specific oral systemic (methotrexate, sulfasalazine, leflunomide, cyclosporine, Dolquine, etc.), new systemic treatments (e.g., anti-inflammatory drugs and analgesics), new specific oral systemic treatments (apremilast, tofacitinib), subcutaneous or intravenous biological therapies (TNFα inhibitors, interleukin [IL] 12/23 inhibitors, IL-23 inhibitors, and IL-17 inhibitors), treatment duration, satisfaction, concerns, pain management, efficacy, preferences.
- 6
Doctor-patient relationship (disease assessment, treatment goals, available treatments, shared decisions, telemedicine).
- 7
Sources of information.
Patients with SpA including PsA were selected. The diagnosis was self-referred by the patient. However, control questions were added to the survey: how the doctor diagnosed the disease, or the type of SpA presented by the patient to improve the validity of the diagnoses. Given the characteristics of the survey and its objectives, convenience sampling was used from the list of CEADE members and supporters, to invite them to answer the survey (an invitation email was sent to them). The survey was launched on 28 April 2021 via the different channels used by CEADE to communicate with its members and supporters (email, Facebook, Instagram, LinkedIn, Twitter) and closed on 30 June 2021. An expert methodologist periodically monitored the response rate, the basic characteristics of the respondents (disease, age, gender, autonomous community of residence) to ensure maximum representativeness of the sample (including geographical representativeness).
Statistical analysisThe statistical programme Stata 12® (Stata Corporation, College Station, TX, USA) was used for data analysis. A descriptive analysis of the data was performed. Quantitative variables were described by means and standard deviation (SD) and qualitative variables by frequencies and percentages. The population was analysed in two subgroups: SpA which included all patients with SpA except with PsA, who were analysed separately.
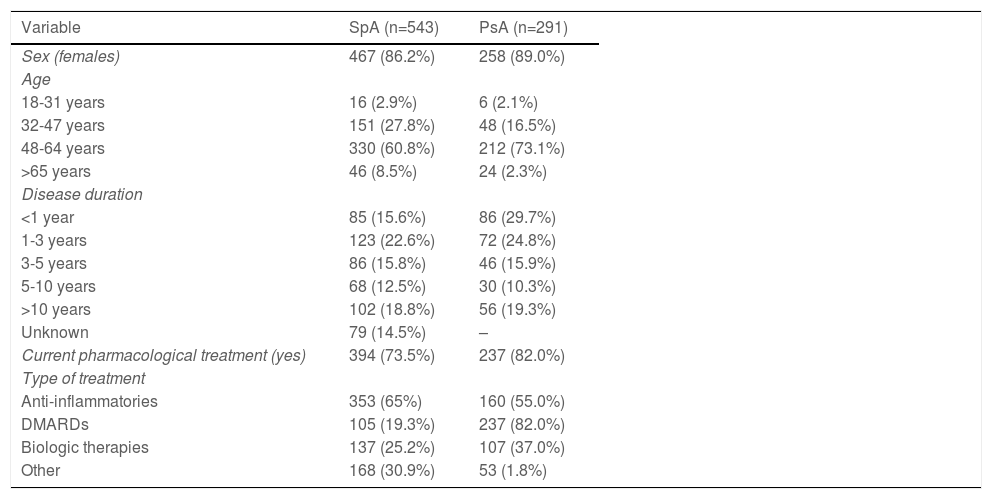
ResultsThe survey collected data from 834 patients (mean response time 10min): 543 with SpA (55% AS, 86% female, 61% aged 48−64 years, 25% with biologic therapies) and 291 with SpA (89% female, 73% aged 48−64 years, 37% with biologic therapies, 81.4% with associated psoriasis); see Table 1 for details. The patients came from all Spain’s autonomous communities and cities; more specifically, for example, 19% from Andalusia, 12% from Catalonia, 10% from the Community of Madrid.
Sociodemographic characteristics of the sample.
| Variable | SpA (n=543) | PsA (n=291) |
|---|---|---|
| Sex (females) | 467 (86.2%) | 258 (89.0%) |
| Age | ||
| 18-31 years | 16 (2.9%) | 6 (2.1%) |
| 32-47 years | 151 (27.8%) | 48 (16.5%) |
| 48-64 years | 330 (60.8%) | 212 (73.1%) |
| >65 years | 46 (8.5%) | 24 (2.3%) |
| Disease duration | ||
| <1 year | 85 (15.6%) | 86 (29.7%) |
| 1-3 years | 123 (22.6%) | 72 (24.8%) |
| 3-5 years | 86 (15.8%) | 46 (15.9%) |
| 5-10 years | 68 (12.5%) | 30 (10.3%) |
| >10 years | 102 (18.8%) | 56 (19.3%) |
| Unknown | 79 (14.5%) | – |
| Current pharmacological treatment (yes) | 394 (73.5%) | 237 (82.0%) |
| Type of treatment | ||
| Anti-inflammatories | 353 (65%) | 160 (55.0%) |
| DMARDs | 105 (19.3%) | 237 (82.0%) |
| Biologic therapies | 137 (25.2%) | 107 (37.0%) |
| Other | 168 (30.9%) | 53 (1.8%) |
DMARDs: Disease-modifying antirheumatic drugs; PsA: Psoriatic Arthritis; SpA: Spondyloarthritis.
In the last month, 78.6% of the SpA patients had pain in the lower back, 63.2% in the hips, and 57.1% in the knees. In addition, 82.5% of the patients with PsA reported involvement (pain, stiffness, redness) of the knees, ankles, feet and/or hands, and 51% reported dactylitis. Moreover, over the past month the degree of fatigue, morning stiffness, and sleep problems, both in the patients with SpA and PsA, reached averages above 8 (scale from 0: none to 10: a lot). Furthermore, 70.2% of the patients with SpA and 66% with PsA have become accustomed to living with pain on a daily basis. The average impact on quality of life on a scale of 1 (none) to 10 (very high) of pain, fatigue, and sleep problems was around 4.
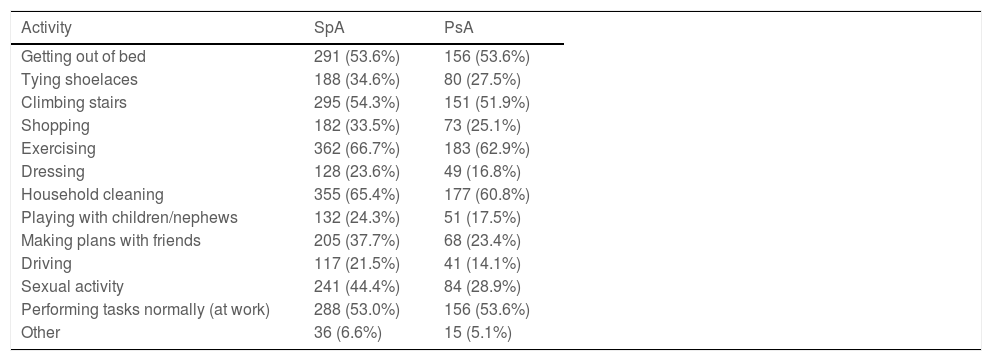
The activities of daily living most affected in both SpA and PsA were exercise (66.7% and 62.9% of patients, respectively) and house cleaning (65.4% and 60.2%) (Table 2).
Activities of daily living most affected by SpA and PsA.
| Activity | SpA | PsA |
|---|---|---|
| Getting out of bed | 291 (53.6%) | 156 (53.6%) |
| Tying shoelaces | 188 (34.6%) | 80 (27.5%) |
| Climbing stairs | 295 (54.3%) | 151 (51.9%) |
| Shopping | 182 (33.5%) | 73 (25.1%) |
| Exercising | 362 (66.7%) | 183 (62.9%) |
| Dressing | 128 (23.6%) | 49 (16.8%) |
| Household cleaning | 355 (65.4%) | 177 (60.8%) |
| Playing with children/nephews | 132 (24.3%) | 51 (17.5%) |
| Making plans with friends | 205 (37.7%) | 68 (23.4%) |
| Driving | 117 (21.5%) | 41 (14.1%) |
| Sexual activity | 241 (44.4%) | 84 (28.9%) |
| Performing tasks normally (at work) | 288 (53.0%) | 156 (53.6%) |
| Other | 36 (6.6%) | 15 (5.1%) |
PsA: Psoriatic Arthritis; SpA: Spondyloarthritis.
The survey included a section to assess concerns related to the disease over the past year. It should be noted that 74% of the patients with SpA and 71% with PsA were concerned about pain, and almost 60% and 66.3%, respectively, about loss of mobility and autonomy. Similarly, their work was affected to a high degree. On a scale of 1 (none) to 10 (very much), the average impact of these diseases on the work environment is close to 8. More specifically, the most frequently described work-related problems in the last two years were absenteeism from work (due to disease activity, tests, medical check-ups, etc.), found in 33.5% of the patients with SpA and 29.2% of those with PsA, and general impairment of working life (31.3% and 28.9%).
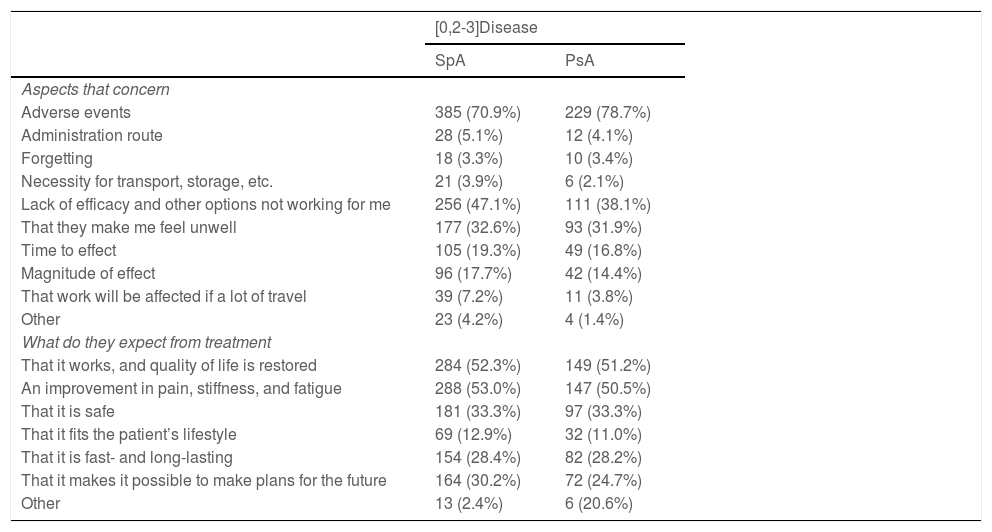
In terms of treatment, the level of satisfaction with treatment (scale 0: none to 10: very high) was low in the SpA patients, mean 5.5, and somewhat higher in PsA, mean 6.2. Satisfaction was higher with biologic therapies (means above 6–7 depending on the biologic) than with disease-modifying drugs (DMARDs) (∼6.5) or anti-inflammatory drugs (∼5), in both disease groups. As shown in Table 3, the onset of adverse events was of most concern to the patients, regardless of the disease, followed by lack of efficacy. Many respondents (just over 50%) expected treatments to help them regain their quality of life and to improve pain, stiffness, and fatigue. However, it should be noted that the symptoms least improved by the treatments used are pain (45.1% and 41.2%) and fatigue (40.3% and 35.0%) in SpA and PsA, respectively. Regarding route of administration preferences, on a scale from 1 (none) to 5 (very high), oral (mean 3.8 in PsA and PsA) was the most preferred route, followed by subcutaneous (mean 3.3 and 3.5) and intravenous (mean 1.8 and 1.6). The majority of the patients also considered the oral route to have the greatest positive influence on adherence to treatment.
Aspects that most concern patients with SpA and PsA about treatments and what they expect from treatments.
| [0,2-3]Disease | ||
|---|---|---|
| SpA | PsA | |
| Aspects that concern | ||
| Adverse events | 385 (70.9%) | 229 (78.7%) |
| Administration route | 28 (5.1%) | 12 (4.1%) |
| Forgetting | 18 (3.3%) | 10 (3.4%) |
| Necessity for transport, storage, etc. | 21 (3.9%) | 6 (2.1%) |
| Lack of efficacy and other options not working for me | 256 (47.1%) | 111 (38.1%) |
| That they make me feel unwell | 177 (32.6%) | 93 (31.9%) |
| Time to effect | 105 (19.3%) | 49 (16.8%) |
| Magnitude of effect | 96 (17.7%) | 42 (14.4%) |
| That work will be affected if a lot of travel | 39 (7.2%) | 11 (3.8%) |
| Other | 23 (4.2%) | 4 (1.4%) |
| What do they expect from treatment | ||
| That it works, and quality of life is restored | 284 (52.3%) | 149 (51.2%) |
| An improvement in pain, stiffness, and fatigue | 288 (53.0%) | 147 (50.5%) |
| That it is safe | 181 (33.3%) | 97 (33.3%) |
| That it fits the patient’s lifestyle | 69 (12.9%) | 32 (11.0%) |
| That it is fast- and long-lasting | 154 (28.4%) | 82 (28.2%) |
| That it makes it possible to make plans for the future | 164 (30.2%) | 72 (24.7%) |
| Other | 13 (2.4%) | 6 (20.6%) |
PsA: Psoriatic Arthritis; SpA: Spondyloarthritis.
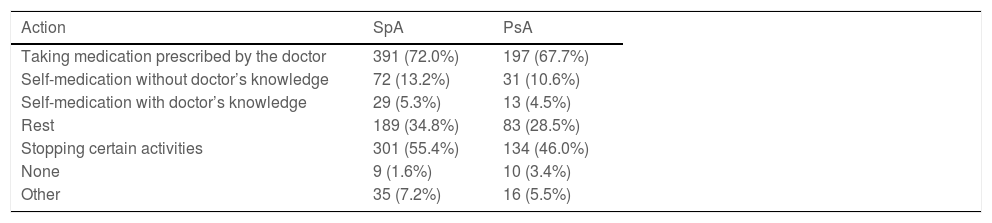
In terms of pain management (Table 4), the strategies most frequently followed by the patients were taking the medication as prescribed by the doctor (72.0% in the SpA and 67.7% in the PsA patients), followed by stopping certain activities (55.4% and 46.0%, respectively).
Pain management (control) of patients with SpA and PsA.
| Action | SpA | PsA |
|---|---|---|
| Taking medication prescribed by the doctor | 391 (72.0%) | 197 (67.7%) |
| Self-medication without doctor’s knowledge | 72 (13.2%) | 31 (10.6%) |
| Self-medication with doctor’s knowledge | 29 (5.3%) | 13 (4.5%) |
| Rest | 189 (34.8%) | 83 (28.5%) |
| Stopping certain activities | 301 (55.4%) | 134 (46.0%) |
| None | 9 (1.6%) | 10 (3.4%) |
| Other | 35 (7.2%) | 16 (5.5%) |
PsA: psoriatic arthritis; SpA: spondyloarthritis.
However, 22% of the respondents with SpA and 14% with PsA reported that their doctor never asked them about the aspects that limit their life. Of the respondents, 14.3% and 6%, respectively, never discussed the impact of the disease on quality of life, and 43.8% (SpA) and 31.2% (PsA) did not discuss treatment goals with the doctor. Similarly, almost 30% of respondents (irrespective of the underlying disease) said they would like to have more time to discuss issues and concerns with the rheumatologist, and about 25% would like more follow-up visits.
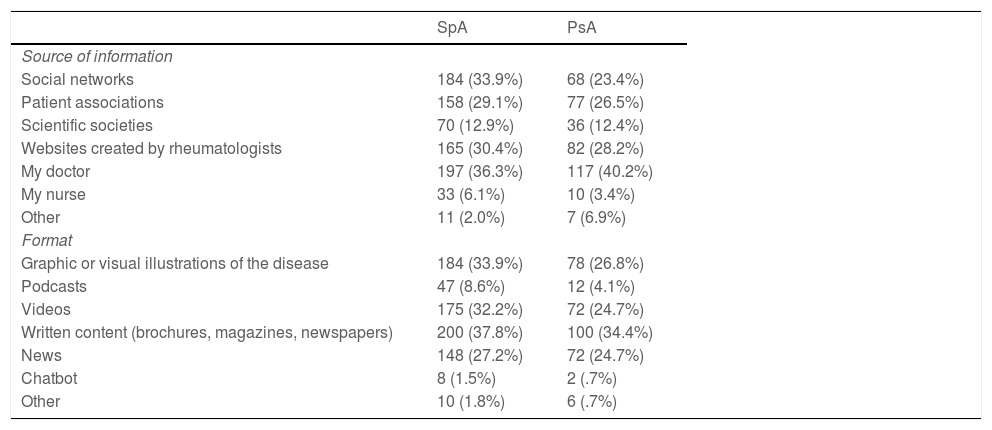
Table 5 describes the most frequently used sources of information and formats on SpA and PsA. The physician is the main source of information for 36.3% of the patients with SpA and for 40.2% with PsA. In second and third place are websites created by rheumatologists and social networks. Written content (brochures, magazines, newspapers) and graphic or visual illustrations about the disease were the formats most used.
Sources of information about their disease most frequently used by patients.
| SpA | PsA | |
|---|---|---|
| Source of information | ||
| Social networks | 184 (33.9%) | 68 (23.4%) |
| Patient associations | 158 (29.1%) | 77 (26.5%) |
| Scientific societies | 70 (12.9%) | 36 (12.4%) |
| Websites created by rheumatologists | 165 (30.4%) | 82 (28.2%) |
| My doctor | 197 (36.3%) | 117 (40.2%) |
| My nurse | 33 (6.1%) | 10 (3.4%) |
| Other | 11 (2.0%) | 7 (6.9%) |
| Format | ||
| Graphic or visual illustrations of the disease | 184 (33.9%) | 78 (26.8%) |
| Podcasts | 47 (8.6%) | 12 (4.1%) |
| Videos | 175 (32.2%) | 72 (24.7%) |
| Written content (brochures, magazines, newspapers) | 200 (37.8%) | 100 (34.4%) |
| News | 148 (27.2%) | 72 (24.7%) |
| Chatbot | 8 (1.5%) | 2 (.7%) |
| Other | 10 (1.8%) | 6 (.7%) |
PsA: psoriatic arthritis; SpA: spondyloarthritis.
In this survey we have shown that, despite the latest advances in SpA including PsA, the impact of this group of diseases is still high in many patients. We also found that there remain unmet needs in these patients. We would like to highlight the high impact of symptoms such as fatigue on patients' daily lives, with almost two thirds of patients reporting that they are used to living with pain on a daily basis, and the work-related problems caused by SpA, including PsA. We would also like to draw attention to the low level of satisfaction overall with treatments, and to the need reported by patients for more time and dialogue with their rheumatologists. The latest such data reported in our country come from the ATLAS project survey launched in 2016, which included patients with axial SpA (not PsA)11. Despite the progress made in the last five years, the impact of the disease on patients is still significant.
We conducted an extensive nationwide survey to obtain these data, which included a very large number of patients with SpA including PsA from all over Spain, whose sociodemographic characteristics are quite similar to those reported in observational studies in our country17, therefore we consider it a fairly representative sample of this group of diseases.
Health care models for chronic diseases such as SpA have been based on holistic, patient-centred care in recent years. This implies a more active role for patients in decision-making. Decisions will now include not only clinical aspects, but also patient opinion. It is therefore essential to know how they experience their disease, what their views are on treatments, and their concerns and unmet needs. Based on these principles, many clinical practice guidelines recommend shared decision-making with the patient and including their perspective in these decisions6.
This survey analysed the patients' opinion on different, very relevant aspects of their disease. Firstly, we found a high prevalence of pain (and in some cases arthritis) in all patients surveyed. It is possible, as described above, that some patients may have developed central pain sensitisation18, but others may have had disease activity. Regardless of the type of underlying pain or the objective presence of arthritis, the survey data suggest that these patients' pain needs to be better managed and as early as possible to avoid central sensitisation and perhaps better assess disease activity. In cases of chronic pain, it would be advisable to assess for central sensitisation in order to adjust treatment. A survey conducted in three Latin American countries in patients with PsA, showed that a significant percentage had moderate pain intensity at the time of the study14. Similarly, another survey, conducted in 13 European countries (EMAS), showed that a large percentage of patients with axial SpA not only experience, but are also very afraid of pain13. Along with pain, fatigue, and sleep disturbances, which, like pain, are very frequent, significantly impact patients' quality of life and are a major focus of their concerns about the disease. In recent years, several studies have been published in the literature that have also highlighted the prevalence and impact of sleep disorders11,19. The ATLAS project survey found that one fifth of patients with axial SpA have sleep disorders11, and slightly more than half in the EMAS survey13. International organisations such as the Ankylosing Spondylitis Assessment Study (ASAS) and Outcome Measures in Rheumatoid Arthritis Clinical Trials (OMERACT) also include them as domains to be assessed in clinical trials20,21. Furthermore, these variables are patient reported outcomes (PRO), and although they are subjective, several studies have shown that they correlate well with objective disease variables22 and reflect the patient's experience. Therefore, we believe that these variables should be systematically assessed in daily practice23, and that research should focus part of its resources on improving these variables that highly impact patients.
Another important finding, also widely described in the literature10, is the occupational impact of this group of diseases. Although the percentage reported in our survey is somewhat lower than that reported in the ATLAS project five years ago11, this impact is still very significant. In the EMAS survey, up to two thirds of patients reported difficulties in finding work due to the disease13, and the Latin American survey also found a significant impact in relation to absenteeism and difficulties at work14. This impact must also be contextualised, because many of these diseases appear in young people. Therefore, we consider that this variable could be given more relevance, together with objective variables and PROs, in decision-making in relation to the disease. Although changes in the patients’ work environment are not in the hands of professionals, more social or even medical information provided to patients' work managers could help in this regard.
The low level of satisfaction with treatments is striking, somewhat lower in SpA than in PsA. And with regard to treatments specifically, satisfaction with biologic therapies is higher than with synthetic DMARDs and anti-inflammatory drugs. In the ATLAS project, many patients reported being encouraged by and satisfied with the effects of using biologic treatments, in their ability to change their disease process and improve their quality of life11. Very similar results have been observed in other surveys of patients with rheumatic diseases16. This study was not designed to analyse this question in depth, but there are data suggesting that in daily practice the recommendations made for correct patient management are not well implemented24. Of these, we highlight the need to reach a consensus on therapeutic objectives. Many guidelines recommend informed and shared decision-making between doctors and patients25. To that end, it is essential to bear in mind that the patient's perspective in terms of their experience, priorities, goals, and expectations of the disease is often different from that of the doctor26. In addition, patient empowerment is necessary (for which they will need to acquire certain skills, have accurate and adapted information, be actively listened to, etc.), to achieve their active involvement in disease management and decision-making27. All this indicates that we must continue working towards maximum implementation of all the recommendations made in this regard and thus improve these patients’ clinical situation.
Although the general data point to a good scenario regarding the doctor-patient relationship, there remain areas for improvement, for example in terms of assessing the impact of this group of diseases on patients' quality of life. Other international surveys have also shown that doctor and patient are not always attuned14. Therefore, and even more so in the context of the current pandemic (which may have led the patients to report that they would like to have more time with the rheumatologist and more follow-up visits), we believe it important to follow the recommendations published in this regard28. Training health professionals in social and communication skills, motivational interviewing, etc., could contribute positively to improving the doctor-patient relationship.
Finally, we must mention a number of limitations of this survey. Due to the type of design and the source for selecting patients (patient associations), selection bias cannot be ruled out. In other words, patients whose disease was more active or severe may have been more willing to answer the survey. Likewise, given that an online system was used, it is possible that there were patients without internet access or who, due to age or other conditioning factors, were not users of new technologies. However, considering the sample size and its characteristics, we are confident that it is fairly representative. However, most of the responses were subjective, and therefore it is always important that they are put into context.
In summary, in the current context, where we have a comprehensive approach with an innovative, broad, and effective therapeutic arsenal, as well as excellent health professionals, the impact of SpA, including PsA, remains very high. We must therefore continue to work to improve this situation.
Authors’ contributionEstíbaliz Loza and Pedro Plazuelo contributed equally and fully to the design of the study, the analysis and interpretation of the data, critically reviewed the article, and approved the version for publication.
FundingThis work was funded by CEADE.
Conflict of interestsEL has received funding for research and teaching projects from AbbVie, Lilly, Pfizer, Roche, Sanofi, Gebro, Bristol-Myers Squibb, UCB, Novartis, MSD. PP has no conflict of interest to declare.
We would like to thank the CEADE members for their participation in the survey.