To propose a consensus modification of the HAQ according to the predominant values, language, and culture of the society.
MethodsFirst, a scoping review of the literature and a survey of HAQ users were conducted to identify the problems of this questionnaire. In a second phase, a meeting was held with expert professionals to discuss the results and design proposals for modification.
ResultsThe scoping review allowed us to describe the main versions of the HAQ, as well as their psychometric properties. The HAQ users survey assessed the degree of comprehension, usefulness, timeliness, and universality of each of the items, and suggestions and opinions on its main limitations were accepted. During the discussion meeting, modifications to the items were proposed based on the results of the scoping review and the users survey. In addition, the difficulty of understanding the items, their difficulty in assessing intended movements, redundancy, obsolescence, and possible gender bias were taken into account.
ConclusionsAn update of the Spanish version of the HAQ is proposed based on the literature review and expert opinion that highlights the paradigm shift in cultural values and aims to increase the content validity and discrimination capacity of this questionnaire.
Proponer una modificación consensuada del Health Assessment Questionnaire (HAQ) según los valores, idioma y cultura predominantes en la sociedad española actual.
MétodosEn primer lugar, se realizó una revisión de alcance de la literatura y una encuesta a usuarios del HAQ para identificar las limitaciones de este cuestionario. En una segunda fase se celebró una reunión con profesionales expertos para discutir los resultados y diseñar propuestas de modificación.
ResultadosLa revisión de alcance permitió describir las principales versiones del HAQ, así como sus propiedades psicométricas. En la encuesta a usuarios del HAQ se valoraron el grado de comprensión, la utilidad, la actualidad y la universalidad de cada uno de los ítems y se admitieron sugerencias y opiniones sobre sus principales inconvenientes. Durante la reunión de discusión se propusieron modificaciones de los ítems en función de los resultados de la revisión de alcance y de la encuesta a usuarios. Además, se tuvieron en cuenta la dificultad de comprensión de los ítems, su dificultad para evaluar los movimientos previstos, el carácter redundante, su obsolescencia y el posible sesgo de género.
ConclusionesSe propone una actualización de la versión española del HAQ en base a la revisión de la literatura y a la opinión de expertos que pone de manifiesto el cambio de paradigma en los valores culturales y que pretende aumentar la validez de contenido y capacidad de discriminación de este cuestionario.
The Health Assessment Questionnaire (HAQ) is the most widely used questionnaire to assess functional ability in patients with rheumatoid arthritis (RA), and in the general population1,2. It includes twenty activities of daily living grouped into eight categories (dressing and grooming, getting up, eating, walking, hygiene, reaching, grasping and complex activities) and asks about the ability to perform each activity in the past week, grading the response from 0 (no difficulty) to 3 (unable to do so). In addition, it adds another 14 questions on the need for help3,4.
Although the HAQ was developed for RA patients, it is now used as a generic questionnaire5,6. The activities included in its initial development in the 1980s were standard at the time, but they lack universal value and their relevance is highly dependent on the environment in which the individual lives7,8. Socio-cultural factors modify patient expectations and outcomes8,9. It has been suggested that the HAQ is not adapted to certain populations because it includes activities that are unusual in some cultures (“getting out of the car” or “working in the garden”), or inappropriate in some people (“cutting meat” in the case of vegetarians), and discrepancies have been observed between the patient’s perception and the score obtained7,9,10, underlining the need to assess the relevance of some items in different clinical contexts11.
In the years that have passed since the development of the HAQ, very important social changes have taken place that limit the current relevance of some items and may alter its psychometric characteristics12.
The aim of this study is to propose a consensual modification of the HAQ, with a perspective of fairness and universality, according to the predominant values in current Spanish society.
Material and methodsTwo-phase study. Phase 1: identification of possible limitations and areas of improvement in the HAQ, through review of the literature scope (1 A) and an HAQ user survey HAQ (1 B). Phase 2: meeting of experts to assess the results and design modification proposals.
1A. Scope reviewThe search strategy was designed to respond to the following question: “which versions of HAQ are used in patients with RA and what are its main limitations? The objective was to identify articles related to versions or modifications of the HAQ. The following inclusion criteria were defined: 1) studies which included patients with RA (population); 2) on the development or validation of different versions of the HAQ (intervention); 3) assessment of psycometric properties or limitations (outcome); and 4) by type of study only including reviews (systematic or narrative).
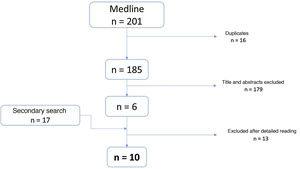
An expert documentalist designed the search strategies in Medline, using MeSH terms and free text. The resulting records were downloaded into a bibliographic manager (EndNote®). Duplicates were identified and removed and studies were selected, first by title and abstract and then by close reading, with collection of relevant information and identification of additional articles.
1B. HAQ user surveyA survey was designed to find out the opinion of healthcare professionals and RA patients on different aspects of the HAQ and its need for updating. Recruitment was done through social networks (Twitter and LinkedIn), or direct invitation to professionals with a recognised interest in these questionnaires.
For each item, comprehension, usefulness, timeliness and universality were rated on a scale of 1 (“not at all”) to 10 (“very much”), with scores above and below 7 being used to classify ratings as “good/very good” and “poor/very poor”, respectively.
Free text spaces were allowed for suggestions from respondents.
Due to the nature of the study, no ethics committee approval was required.
Results1A. Scope reviewTen articles were selected for close reading (Fig. 1). Most of the eliminated articles concerned studies of efficacy, utility and cross-cultural adaptation.
One of the selected articles was a systematic review, published in 2021, on the psychometric properties of patient reported outcome measures (PROMs) used in RA over the last 20 years. In this review, and for the domain of functional ability, the different versions of the HAQ13 are described. Table 1 presents the general and psychometric characteristics of these versions.
General and psychometric characteristics of the different versions of the HAQ.
| Characteristic | HAQ | M-HAQ | MDHAQ | HAQ-II | PI-HAQ |
|---|---|---|---|---|---|
| Type | Specific | Hybrid | Hybrid | Specific | |
| Content | 20 ADL (8 areas) | 8 ADL (1/area) | 10 items: | 10 ADL | |
| 13 help | 8 ADL | ||||
| 2 complex | |||||
| Score | ADL: Likert 0−4 | Likert (0–4) | Likert (0–4) | Likert (0–4) | |
| Help: Yes/no | |||||
| Period | 1 week | 3 months | 1 week | 1 week | 1 week |
| Score | From 0 to 3: | From 0 to 3: | From 0 to 3: | ||
| 0 (normal) | 0 (normal) | 0 (normal) | |||
| 3 (worse FC) | 3 (worse FC) | 3 (worse FC) | |||
| Time | Administration 5 m | Administration <5 m | Administration <5 m | Administration <5 m | |
| Estimation: <2 m | Estimation: <1 m | Estimation: <10 s | Estimation: <1 m | ||
| Reliability | Internal consistency | Internal consistency | Internal consistency | Internal consistency | |
| Test-retest | |||||
| Validity | Content | Structural | Convergent | Structural | Construct |
| Structural | Convergent | Predictive | Convergent | ||
| Convergent | Predictive | ||||
| Sensitivity to change | Yes | Yes | No | Limited | |
| Strengths | Gold standard FC | Brevity | Brevity | >Correlation with HAQ | |
| Multiples languages | |||||
| Limitations | Long | It is not = HAQ | Floor effect (25%) | Floor effect (5.8%) | Complementary to HAQ, not substitute |
| Complexity Estimation | Floor effect | Not sensitive to change | Not sensitive to change | ||
| Floor effect (10%) | Not sensitive to change | ||||
ADL: activities of daily life; FC: functional capacity; HAQ: Health Assessment Questionnaire; HAQ-II: Health Assessment Questionnaire-II; MDHAQ: Multidimensional Health Assessment Questionnaire; MHAQ: Modified Health Assessment Questionnaire; MICD: minimally important clinical difference; PI-HAQ: Personal Impact Health Assessment Questionnaire.
Source: Esteve-Vives et al.4.
Ten articles for detailed reading were selected (Fig. 1). Most of the eliminated articles referred to efficacy, utility and transcultural adaptation studies.
One of the selected articles was a systematic review, published in 2021, on the psychometric properties of the patient reported outcome measures (PROM) which have been used in RA for the last 20 years. In this review and for the domain of functional ability, the different versions of the HAQ13 are described. Table 1 presents the general and psychometric characteristics of these versions.
HAQ original or HAQ-DIIt is a self-administered questionnaire developed by Fries et al. in 1980. It contains 34 items: 20 items on the patient’s difficulty in performing various activities of daily living (ADLs) divided into 8 areas and with a Likert-type response with 4 options (0, 1, 2, 3), and 14 additional items on the need for help with a yes/no response. The scores in each area are given according to the need for help, and an overall score is obtained from 0 to 3, where 0 represents the absence of functional limitation and 3 represents severe disability. Fries et al. presented the questionnaire together with an analysis of its reliability (internal consistency and test-retest) and its multidimensional structure (principal component analysis). However, there are no data on sensitivity to change or on the impact of comorbidity on the score6.
MHAQExperience with the HAQ revealed some limitations, such as its long duration, difficulty of calculation, and lack of discrimination in some specific situations. Consequently, Pincus et al. developed a first modification of the HAQ (modified HAQ or MHAQ) by decreasing the number of ADLs assessed and adding items on the degree of satisfaction and change in difficulty perceived by the patient in the previous 6 months14.
In the MHAQ the number of ADLs was reduced from 20 to 8, one for each area of the original HAQ, and the questions on the need for help were removed. This resulted in an easier to score version with the same range from 0 to 3. It was shown that the 8 items of the MHAQ capture most of the information contained in the 20 items of the original HAQ and is easier to use due to its brevity. However, it has a floor effect (people with functional impairments may have normal scores), and its sensitivity to change is lower than that of the longer versions5. The development of the MHAQ was performed in a population of different rheumatic diseases, with no validation data of the index in RA15.
Multidimensional HAQ (MDHAQ)Although the MHAQ is shorter and easier to complete than the original questionnaire, it also has a floor effect. In addition, the HAQ and MHAQ only assess the simplest or most basic ADLs, but not other complex activities for which some patients may have difficulties that may go unidentified.
In order to address these problems, to assess psychological distress, and to improve detection ability at the lower ends of the scale, the multidimensional HAQ (MDHAQ) was designed. The MDHAQ includes 10 items, 8 from the original plus 2 additional complex activities referring to the ability to walk 3 km or to participate in recreational or sporting activities. The 2 advanced ADLs increase the likelihood of detecting score changes when there is clinical improvement, thus reducing the floor effect. The MDHAQ also assesses sleep, depression, fatigue, pain, joint count and symptoms. Partial validation data (face validity and test-retest reliability) have been obtained in a heterogeneous sample of rheumatic diseases15.
HAQ-IIThe many limitations of HAQ, such as its long duration (34 items), non-lineal distribution (the differences of score mean the same at different levels of incapacity), the difficulty of comprehension of some items, and the floor effect, led to the design of a new version by Wolfe and Pincus in 2004, the HAQ-II, which contains 10 items, 5 from the HAQ and 5 additional ones16.
As a shorter questionnaire, it is easier to complete and score and its floor effect is lower than that of the HAQ (5.8% vs. 10%). It correlates with clinical variables (convergent validity) and its performance is similar to that of the HAQ, which facilitates the exchange of scores. Although its psychometric properties are more favourable than those of the original HAQ, it is not as widely used5.
Personal impact (PI-HAQ)The calculation of weightings of the HAQ items allows the impact of the disability on the individual patient to be assessed. Thus, Hewlett et al. proposed the personal impact PI-HAQ in 200217. The PI-HAQ should be seen as a complementary instrument to the HAQ and not as a substitute. Its main value is to complete the assessment of disability and to facilitate its interpretation.
Evaluation of the different versions of the HAQThe validation data of the HAQ and its versions is variable. According to the COSMIN consensus, all have internal consistency, while test-retest reliability has only been adequately analysed for the original HAQ. Content validity, which assesses the relevance and comprehensibility of the items, has only been demonstrated for the original HAQ. Structural validity, or the degree to which the scores of an instrument are an adequate reflection of the dimensionality of the construct, has been demonstrated in all versions, although the results of the MDHAQ are limited5,18. As there is no gold standard, it is not possible to assess criterion validity. All versions have convergent validity, especially the original. Data on sensitivity to change, or the ability of an instrument to detect clinical change over time, are limited, among other reasons because of the multitude of statistics used. The best results have been obtained for the HAQ and the M-HAQ, and to a lesser extent for the HAQ-II5. Instruments with 3–4 category ordinal scales, such as the HAQ, have lower sensitivity to change than those using continuous interval scales, which may explain the low sensitivity to change of this tool19.
There are several studies which compare the different versions of the HAQ. Wolfe et al. compared the HAQ, the MHAQ composed of only 8 items, and the RA-HAQ, which also has 8 items and adequate psychometric characteristics, although it has not been used clinically20. Differences in distribution could explain the clustering of values at the lower end of the scale in the abbreviated forms, resulting in many individuals having a normal score and a significant part of the functional impairment not being identified, confirming the floor effect. Despite being longer, with more difficult items and more complex scoring, the original HAQ is more efficient in discriminating patients and is more sensitive to change than the abbreviated forms.
Maska et al. compared the psychometric characteristics of the original HAQ and different later versions. According to these authors, the main limitations of the HAQ are its length, the complexity of calculation, the non-linear scoring (floor effect), and the consequent difficulty in assessing sensitivity to change21. Although shorter and easier to apply, the MHAQ is not equivalent to the original HAQ, as it assesses fewer items, which may mask patients’ disability. Again, scores tend to cluster at the lower end of the scale, showing a non-normal distribution that makes it difficult to assess sensitivity to change. The MDHAQ has the best correlation with the original HAQ, the lowest impact of missing items and the lowest floor effect, around 5.8%, significantly lower than that of the HAQ (10%) and the MHAQ (25%)21.
Improved-HAQIt is a slight modification of the HAQ that uses the same 20 items but adds a new response category (“with some difficulty”) to try to reduce the floor effect. Introduced in 2007 as HAQ-100 and later as PROMIS HAQ, its name was subsequently changed to Improved-HAQ to avoid confusion with the official Patient-Reported Outcome Measurement Information System (PROMIS) instruments. The Improved-HAQ contains 20 items on ADLs plus 4 on the need for help. Unlike the original, the items are not grouped by domains. A 5-choice Likert scale is used for responses, with a total score ranging from 0 to 100. It shows higher reliability and lower floor effect than the original version. Its main limitation is that the change in score from 0–3 to 0–100 makes it difficult to compare with studies carried out with the original version, and there are no data on construct and predictive validity21.
1B. HAQ user surveyIn the user survey, 24 responses were obtained, corresponding to physicians (n = 7; 70.8%), rheumatology nurses (n = 3; 12.5%), RA patients (n = 2; 8.3%), and rheumatology psychologists (n = 2; 8.3%).
Item comprehension was the highest rated aspect with scores ≥8, the lowest being items 3 (8.0 ± 2.0); 6 (8.2 ± 2.0); 13 (8.0 ± 2.0); and 18 (8.0 ± 2.1). The least useful items were 6 (6.5 ± 2.4); 15 (7.1 ± 2.6); 17 (7.0 ± 2.5); and 18 (7.2 ± 2.1). The least current are 6 (5.9 ± 2.7); 17 (6.4 ± 2.9); 18 (7.1 ± 2.5); and 20 (7.4 ± 2.6). Those considered less universal 6 (6.1 ± 2.5), 15 (7.1 ± 2.7); 17 (6.4 ± 3.0) and 18 (6.9 ± 2.6) (Table 2).
Results of the HAQ user survey.
| Item | Understandable | Useful | Contemporary | Universal | Limitations/modification suggestions | |
|---|---|---|---|---|---|---|
| Dressing grooming | 1. Self-dressing including doing up buttons and tying shoelaces | 9.4 ± .8 | 9.0 ± 1.2 | 7.7 ± 1.9 | 8.1 ± 2.2 | Eliminate shoelaces, buttons |
| 2. Lathering head | 9.4 ± .6 | 8.4 ± 1.6 | 8.4 ± 1.8 | 8.6 ± 1.9 | Putting on/taking off socks, tights | |
| Getting up | 3. Getting up from a chair without arms | 8.0 ± 2.0 | 8.3 ± 1.6 | 8.3 ± 1.3 | 8.4 ± 1.8 | Fastening bra |
| 4. Getting into and out of bed | 9.1 ± 1.5 | 9.0 ± 1.2 | 9.3 ± .8 | 9.4 ± .8 | Getting up “unaided” | |
| Getting out of bed unaided | ||||||
| Eating | 5. Cutting up meat | 8,9 ± 1,2 | 8,1 ± 1,6 | 7,7 ± 1,8 | 7,7 ± 1,9 | |
| People who do not eat meat | ||||||
| 6. Opening a new carton of milk | 8.2 ± 2.0 | 6.5 ± 2.4 | 5.9 ± 2.7 | 6.1 ± 2.5 | Need to modify 6 | |
| 7. Serving oneself a drink | 8.3 ± 1.9 | 7.8 ± 2.1 | 8.1 ± 1.9 | 8.2 ± 1.9 | Serving oneself a drink by getting the full jug or bottle | |
| Walking | 8. Walking outside the house on a level surface | 9.0 ± 1.3 | 8.9 ± 1.0 | 9.1 ± 1.0 | 9.1 ± 1.0 | Add “distance (200 m)” |
| 9. Going up five steps | 9.5 ± .7 | 8.9 ± 1.2 | 9.1 ± 1.2 | 9.2 ± 1.2 | ||
| Hygiene | 10. Washing and drying the whole body | 9.1 ± 1.4 | 8.7 ± 1.7 | 8.2 ± 1.5 | 9.1 ± 1.3 | Replace by “is able to shower, bathe and wash hair without support or help” |
| 11. Go into and out of the bathroom | 9.1 ± 1.1 | 8.8 ± 1.5 | 8.9 ± 1.2 | 9.0 ± 1.1 | Difficult comprehension, possibility of modification | |
| 12. Shower | 9.3 ± 1.0 | 8.4 ± 2.2 | 8.9 ± 1.2 | 8.8 ± 1.5 | Pick up anything small from the floor | |
| Reaching | 13. Get a 1 kg packet of sugar from a shelf above one’s head | 8.2 ± 2.0 | 7.9 ± 2.1 | 7.8 ± 2.2 | 8.1 ± 2.0 | Sign a document |
| 14. Bend down and pick up clothes from the floor | 8.8 ± 1.5 | 8.9 ± 1.2 | 8.8 ± 1.6 | 8.8 ± 1.6 | Change the time on a wristwatch | |
| Pressure | 15. Open a car door | 8.5 ± 1.8 | 7.1 ± 2.6 | 7.5 ± 2.4 | 7.1 ± 2.7 | Open the washing machine or freezer |
| 16. Open closed jars which had already previously been opened | 8.8 ± 1.4 | 8.6 ± 1.6 | 8.5 ± 1.5 | 8.5 ± 1.7 | Dress, wash, groom (associate with item 1) | |
| 17. Turn taps on and off s | 8.3 ± 1.9 | 7.0 ± 2.5 | 6.4 ± 2.9 | 6.4 ± 3.0 | Go outside the home to do errands or go shopping | |
| Others | 18. Do errands and go shopping | 8.2 ± 2.1 | 7.2 ± 2.1 | 7.1 ± 2.5 | 6.9 ± 2.6 | Change the time on a wristwatch |
| 19. Get in and out of a car | 9.0 ± 1.2 | 8.0 ± 2.0 | 8.2 ± 1.6 | 8.0 ± 2.0 | Open the washing machine or freezer | |
| 20. Do household chores such as sweeping and washing the dishes | 8.9 ± 1.5 | 7.8 ± 2.3 | 7.4 ± 2.6 | 7.5 ± 2.8 | It is an obsolete item | |
In the free text of the survey, limitations and suggestions for changes to the different items were collected (Table 2).
Discussion and proposal for modificationDuring the meeting of experts (rheumatologists and Spanish-speaking nurses from Spain (n = 7) and Latin America (n = 1)) the results of the review and the survey were discussed, and modifications to the items were proposed based on their comprehensibility, suitability for assessing the movements for which they were designed, redundancy, outdatedness, and gender bias. Suggested changes for each item are presented below and a proposed modified questionnaire is presented in Table 3.
HAQ modification proposal.
| Current version | Modification proposal | |
|---|---|---|
| Dressing, groom | 1. Self-dressing including doing up buttons and tying shoelaces | 1. Self-dressing including putting on one’s shoes |
| 2. Lathering one’s head | ||
| Getting up | 3. Getting up from a chair without arms | 2. Getting up from a chair unaided |
| 4. Getting into and out of bed | 3. Getting into and out of bed unaided | |
| Eating | 5. Cutting up meat | 4. Using a knife and fork to cut food on one’s plate |
| 6. Opening a new carton of milk | 5. Opening drinks in general (bottles, cans, etc.) | |
| 7. Serving oneself a drink | 6. Serving oneself a drink from a 1 L jug or a bottle | |
| Walking | 8. Walking outside the home on level ground | 7. Walking outside the house on level ground for a distance of 200–300 m |
| 9. Going up five stairs | 8. Going up five steps with or without help | |
| Hygiene | 10. Washing and drying the whole body | 9. Is able to shower, bathe and wash hair without support or help |
| 11. Sting down and getting up from the toilet | ||
| 12. Showering | ||
| Reaching | 13. Getting a 1 kg packet of sugar from a shelf above one’s head | 10. Picking up a book from a shelf above one’s head |
| 14. Bending down and picking up clothes from the floor | 11. Bending down and picking up clothes from the floor | |
| Pressure | 15. Opening a car door | 12. Opening a door with a key |
| 16. Opening closed jars which had already previously opened | 13. Opening previously opened jars | |
| 17. Turning taps on and off | 14. Managing the television control | |
| Others | 18. Doing errands and going shoppings | 15. Taking out the rubbish |
| 19. Getting into and out of a car | 16. Getting into and out of a car | |
| 20. Doing household chores such as sweeping and washing the dishes | 17. Participating in recreational activities | |
Explores flexibility and fine mobility of hands. Not very topical (shoes with Velcro) and not very universal (buttons are not used in some countries). Change to “fasten bra” discarded due to gender bias.
Suggestion: self-dressing including putting on one’s shoes.
Item 2. Lathering the headMobility of the shoulder girdle and shoulders. Not very useful for women going to the hairdresser and men with alopecia. Redundancy with “hygiene” domain. Suggestion: add: unaided grooming of the hair.
Item 3. Getting up from a chair, without armsStrength of quadriceps, buttocks and back. Useful, current and universal item, but with comprehension difficulties (“without arms” is not understood). Suggestion: getting up from a chair without support.
Item 4. Getting in and out of bedEssential item that provides a lot of information. Suggestion: the action should be done without help: lying down on and getting out of bed unaided.
Item 5. Cutting up meatOut of date and not universal (people who do not eat meat, because they are vegetarians or because of chewing difficulties). Comprehension problems (does not distinguish between cutting a piece of meat for eating and a piece of meat for cooking). Suggestion: use knife and fork to cut food on your plate.
Item 6. Opening a new milk cartonLow usability, outdated (milk cartons with screw systems), and lack of universality (multiple types of containers). Suggestion: open beverage containers in general (bottles, cans, etc…).
Item 7. Serving oneself a drinkVery ambiguous and difficult to understand. The specific action should be better defined. Suggestion: pour a drink from a jug or a litre bottle.
Item 8. Walking outside the house on level groundMobility of lower limbs. The specific distance needs to be specified. Suggestion: walking outside the house on level ground for a distance of 200−300 m.
Item 9. Going up five stepsCorrect, well put and universal. Suggestion: add “with or without support”.
Items 10, 11, and 12 are redundant (correlation of 0.6 in the modified MHAQ)14 and it is therefore proposed to leave only one hygiene item: “Is able to shower, bathe and wash hair without support or assistance”.
Item 13. Get a 1 kg sugar packet from a shelf which is above your headToo specific, outdated and gender-biased. It was suggested to replace “sugar packet” with a neutral term such as “object”; however, this term does not specify volume or weight and was therefore not considered appropriate. Therefore, the final suggestion was to change sugar packet to a common activity in the collective imagination such as: “Picking up a book from a shelf above your head”.
Item 14. Bend down to pick up clothes from the floorAppropriate, useful, contemporary and universal.
Item 15. Open the car doorObsolete (automatic opening) and not universal (people who do not have a car). Suggestion: open a door with a key.
Item 16. Open closed jars which had been opened previouslyComprehension difficulties with the term “closed”. Suggestion: open previously opened jars.
Item 17. Open and close tapsOutdated (single lever taps) and redundant with the previous one (“open”). The change to other routine activities (operating a mobile phone or computer) is ruled out due to the difficulties some people have with these devices. Suggestion: operate the TV remote control.
Item 18. Running errands and making purchasesOutdated (Internet shopping) and ambiguity regarding the term “errands”. Replaced by a universal activity which involves going outside: taking out the rubbish.
Item 19. Getting in and out of a carUniversal action.
Item 20. Doing household chores such as sweeping or washing the dishesObsolete and gender biased. Suggestion: participation in recreational activities.
There was agreement on the deletion of the help questions as they complicate the scoring and do not add value.
ConclusionA proposal for updating the Spanish version of the HAQ, carried out by Spanish-speaking professionals and patients, is presented, which highlights the paradigm shift in the cultural values that underpin the activities of the questionnaire and aims to increase its content validity and discriminatory capacity.
Once this proposed update has been designed, and before its use in clinical practice, it is necessary to carry out a complete validation study to analyse its dimensionality and structure, and to ensure that its psychometric properties are adequate and in line with those of the original version.
This work can be the starting point for validation studies in different languages and in different patient populations, in order to facilitate comparisons with international studies.
FundingThe article was funded by the Andalusian Foundation of Rheumatology (FAR).
Conflict of interestsThe authors have no conflict of interests to declare.