Polymyalgia rheumatica is an inflammatory rheumatic disease that presents with bilateral pain and stiffness affecting mainly proximal muscles. It affects individuals over 50 years of age and it is usually associated with a raised erythrocyte sedimentation rate. Classically, treatment with low-dose corticosteroids results in a dramatic improvement in both symptoms and laboratory findings.
We report the case of an 80-year-old patient presenting polymyalgia rheumatica coinciding with pleuropericardial effusion. The patient had a very good response to treatment with rapid improvement in the symptomatology and laboratory findings.
Polymyalgia rheumatica is a common disease but it is rarely associated to pleuropericardial effusion. It should be considered in the differential diagnostic in patients presenting with pericardial effusion over 50 years of age due to the good response to treatment.
La polimialgia reumática es una enfermedad inflamatoria reumática que se caracteriza por dolor y rigidez bilateral que afecta principalmente a la musculatura proximal. Aparece sobre todo en personas por encima de los 50 años y se asocia a una velocidad de sedimentación globular elevada en la analítica. La enfermedad generalmente responde muy bien a dosis bajas de corticoides.
A continuación, presentamos el caso de un varón de 80años que presentó un cuadro compatible con polimialgia reumática asociado a derrame pleuropericárdico que respondió rápidamente a corticoides, con rápida mejoría en la sintomatología y en los hallazgos de laboratorio.
La polimialgia reumática es una enfermedad que se presenta con relativa frecuencia pero que raramente se asocia a derrame pleuropericárdico. Es importante tenerla en cuenta en el diagnóstico diferencial del derrame pericárdico en personas mayores de 50años por su buena respuesta a tratamiento.
Polymyalgia reumatica (PMR) is an inflammatory disease of unknown cause characterized by pain and morning stiffness in the cervical region, shoulders and shoulder girdle.1
Its frequency is increased in patients over 50 years and is two times more common in women. The annual incidence in Europe and in the United States varies between 1.3 and 11.3 per 10000 individuals over the age of 50 years.2,3
The association of pericardial effusion (PE) and PMR has rarely been reported. So far, three cases of PMR4–6 associated to PE have been documented and only one with pericardial and pleural effusion. 2 cases of associated cardiac tamponade with PMR have also been recorded.7,8
Case PresentationHere we present the case of an 80-year-old man with a history of hypertension, type 2 diabetes mellitus and chronic atrial fibrillation without anticoagulant and with a history of gastrointestinal bleeding, who was admitted for asthenia, anorexia and weight loss of 3 months duration. Coinciding with this, he had polyarticular pain and morning stiffness, especially in the shoulders and hips, preventing him from walking in the last 3 months. He had no headache.
He was under treatment with omeprazole, domperidone, amlodipine, digoxin, furosemide, metformin and ramipril.
Physical examination showed mild mucocutaneous pallor and decreased breath sounds of the left thorax; the remainder of the examination was normal.
The initial laboratory results highlighted a normocytic, normochromic anemia, Hb 10.2g/dl, normal leukocytes and platelets. The erythrocyte sedimentation rate (ESR) was 105mm/h, CRP 13mg/dl and proteins 6.3mg/dl. Renal function tests were performed and anemia was studied measuring ferritin, vitamin B12 and folic acid, all of them being normal. Proteingram showed increased alpha 2 and normal tumor markers (CA 19-9, CEA, AFP, chorionic gonadotropin), all negative, TSH normal, Mantoux negative. ANA and ANCA negative, complement (C3 and C4) normal.
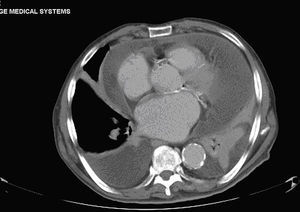
The chest X-ray showed cardiomegaly on admission, with no other findings. A few days later the patient presented an associated bilateral pleural effusion, predominantly on the left side (Fig. 1). A CT of the chest and abdomen reported a pericardial and pleural effusion, moderate in amount and of free morphology, causing a passive collapse of the basal segments of both lower lobes with the rest showing no abnormalities.2
A thoracentesis allowed us to examine the pleural fluid with the following results: LDH 104U/l, protein 3.1g/dl, glucose 116mg/dl, pH 7.52 and normal ADA (transudate characteristics, but in the threshold between exudate and transudate). Fluid cytology: serosanguineous, absence of neoplastic cells.
Subsequently, echocardiography showed: left ventricular hypertrophy, with conserved size and systolic function, mild mitral and aortic insufficiency, with the rest of the valves normal, slight pulmonary hypertension and moderate anterior pericardial effusion and moderate to severe posteriorly with fibrin without collapse during dyastole of the right chambers (Fig. 2).
Since the patient had criteria compatible with PMR (age >50 years, pain on the proximal muscles, shoulders and hip, ESR >40mm/h and we excluded other diagnoses), we confirmed the diagnosis and the patient was treated with prednisone at a dose of 15mg daily.
Clinical improvement was evident in the first 48h, with increased mobility and a clear decrease in rigidity, especially at the level of the shoulder girdle, with the patient being able to walk. Likewise there were decreased inflammatory markers and the X-rays showed a marked decrease of the pleural effusion. The echocardiography performed after one month showed that the pericardial effusion had completely disappeared with only a slight right pleural effusion.
DiscussionPMR patients present bilateral discomfort involving the proximal parts of the limbs and joints in relation to synovitis of proximal joints.
The combination of persistent pain for at least a month, with pain and morning stiffness in the neck region, the shoulder girdle and the pelvic girdle, lasting at least 30min, associated with an increase in ESR of at least 40mm per hour, is highly indicative of polymyalgia reumatica.9 Musculoskeletal pain worsens with movement of the affected areas and typically interferes with activities of daily living.
Shoulder pain is present finding in most of patients (70%–95%), however the hips and neck are less frequently affected (50%–70%). In the shoulders and pelvic girdle pain usually radiates distally into the elbows and knees. The discomfort may start on one side but quickly becomes bilateral.1
Systemic symptoms are common, being present in one third of patients, and include fever, fatigue, anorexia and weight loss.9,10 In our case, the reason for admission was mainly fatigue and weight loss, but after asking specific questions the patient informed us of proximal muscle pain.
On examination, there is limitation of active movements and, often, also passive movements are limited due to pain.
Generally, the diagnosis is made after 2 or 3 months since the onset of symptoms.
Analytically, most patients have mild anemia of chronic disorders, as in our case, and one third of patients have altered liver function tests.2 Rheumatoid factor and ANA are usually negative.
Corticosteroids are used to treat patients at a dose of 10–20mg. The response to corticosteroids is rapid, with resolution of symptoms within days it after the start of therapy. A lack of improvement should lead us to question the diagnosis. The initial dose is usually maintained for 2–4 weeks, and subsequently it can be gradually reduced every week or every two weeks at a maximum rate of 10% every two weeks from the total daily dose. If the steroid dose is reduced or withdrawn too quickly, symptoms may recur. However, approximately 30%–50% of patients have spontaneous exacerbations, and a course of treatment for one or two years is often required. Some patients have a relapsing course and may require low-dose corticosteroids for several years.1,10
Given the clinical presentation of anorexia and weight loss associated with pleural and pericardial effusion, different diagnoses such as tumors, tuberculosis and autoimmune diseases might be suspected, all of which are reasonably discarded when the CT is normal, and Mantoux ADA are negative and, for the case of autoimmune diseases, ANA and ANCA and complement, were negative and clinical presentation was not consistent with these diseases. The diagnosis of rheumatoid arthritis was also considered, which seemed unlikely due to the clinical presentation; in rheumatoid arthritis peripheral joints are more commonly affected, and is characterized by a negative rheumatoid factor. The acute edematous polysynovitis of the elderly (RS3P3), is also a diagnosis that should be considered when joint pain occurs in older people and is characterized, as is PMR, by an excellent prognosis with low doses of corticosteroids; this was excluded since the patient had no synovitis of the distal joints and showed no edema of the back of the hands.
In our patient, clinical improvement was evident within days of initiation of low-dose corticosteroids. One month after treatment, the pericardial effusion completely disappeared and pleural effusion improved considerably.
The presentation of joint pain and stiffness of long duration, accompanying systemic symptoms (anorexia and weight loss), laboratory data (increased ESR and CRP) and a fast response to steroids confirmed the diagnosis of PMR.
Ethical ResponsibilitiesProtection of People and AnimalsThe authors state that no experiments were performed on humans or animals.
Data ConfidentialityThe authors state that no patient data appears in this article.
Right to Privacy and Informed ConsentThe authors state that no patient data appears in this article.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Sánchez Ruiz-Granados E, et al. Presentación de un caso de derrame pleurocárdico en un paciente diagnosticado de polimialgia reumática. Reumatol Clin. 2013;9:376–378.