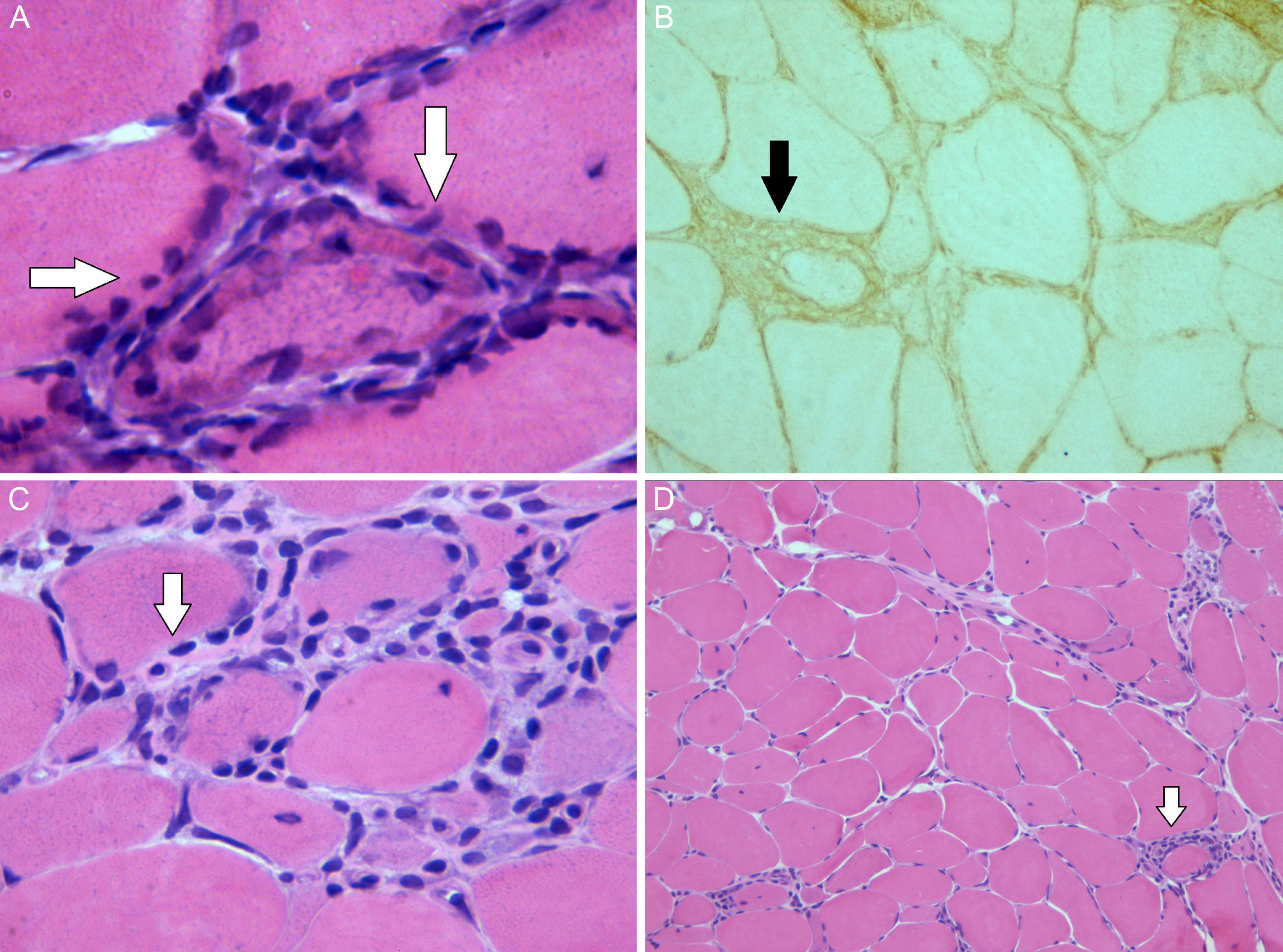
Ulcerative colitis (UC) is an inflammatory disease that affects the colorectal mucosa in a diffuse form, continuously and superficially.1 Polymyositis (PM) belongs to the spectrum of idiopathic inflammatory myopathies, and is differentiated from dermatomyositis (DM) because of the absence of the characteristic skin rash.2 Muscle involvement in the form of PM has rarely been described in UC. We report the case of a patient who was initially diagnosed as having UC, and developed PM over the course of his disease. We also review cases published to date. Our patient was a 46-year-old man, an ex-smoker, who presented with persistent bloody diarrhea with no other associated symptoms, and was diagnosed with UC. At the age of 58 years, he presented with an episode of pain and swollen hands, and was too weak to climb stairs. Laboratory tests detected increases in creatine kinase (CK) (1578U/L) and lactate dehydrogenase (LDH) (506U/L), although all other inflammatory parameters were normal. The rest of the biochemical study, including complete blood count, showed normal values. The immunological study demonstrated the presence of antinuclear antibodies, at a titer of 1/160, and negative tests for anti-extractable nuclear antigens (ENA), anti-DNA antibodies, antineutrophil cytoplasmic antibodies (ANCA), anti-centromere antibodies, anti-Scl-70 and antibodies specific for myositis (Jo-1, PL7, PL12, OJ, EJ, SRP, Pm-Scl, Mi2 and Ku). A muscle biopsy of quadriceps was performed (Fig. 1), and evidenced variability in the size of the muscle fibers, with some necrotic fibers, regenerative basophilic fibers and frequent mononuclear inflammatory cell infiltrates, mostly lymphocytic and located in the endomysium. The expression of the major histocompatibility complex class I antigens was positive in the muscle fibers, all of which was compatible with the diagnosis of PM. Treatment was begun with a tapering dose of prednisone starting at 20mg/day, to be followed by methotrexate (maximum dose 25mg/week), and normalization of the CK and LDH levels was achieved after 16 months of treatment.
Image of the muscle biopsy: (A) There are muscle fibers with regenerative peripheral basophilic areas (hematoxylin–eosin stain ×63). (B) Muscle expression of the class I antigens of the human leukocyte antigen (HLA) system. (C) There is an endomysial lymphocyte cell infiltrate located in the (hematoxylin–eosin stain ×40). (D) Variability of the size of the muscle fibers and periendomysial (hematoxylin–eosin stain ×10).
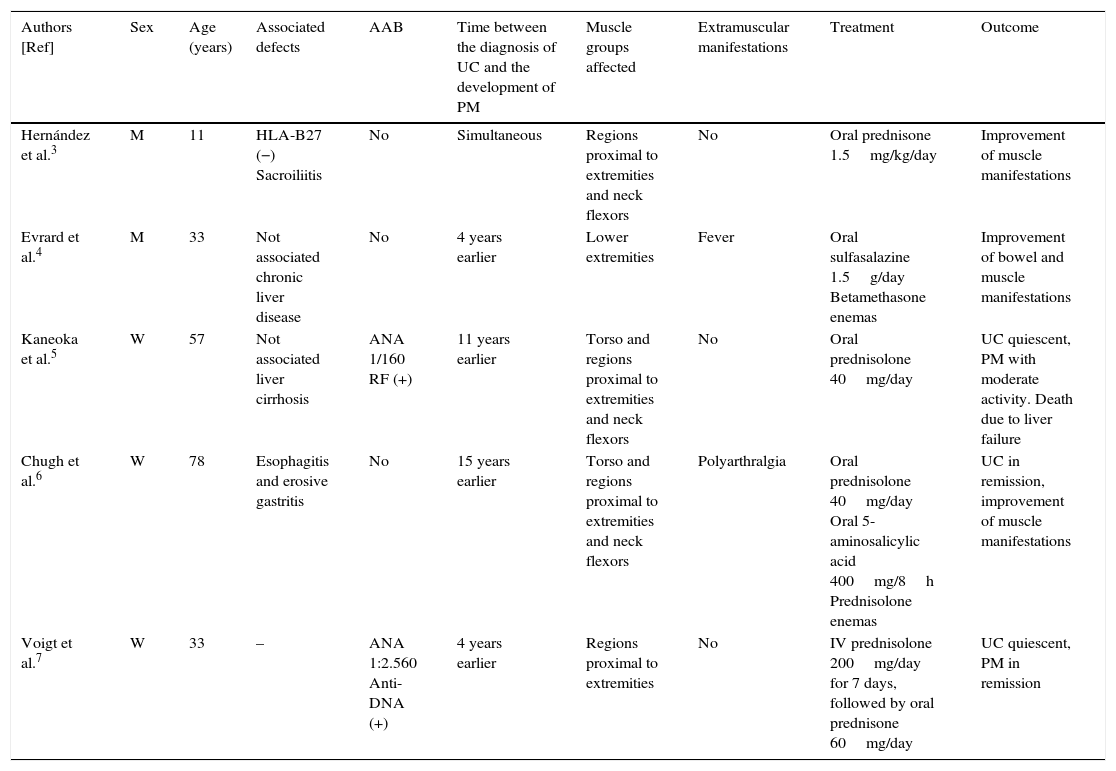
Muscle involvement in inflammatory bowel disease is uncommon; in fact, only 7 cases associating PM and UC have been published to date3–9 (Table 1). Only in the patient we describe was the diagnosis reached because of the increase in muscle enzymes. The response to glucocorticoid treatment was so good, in general, except in an individual who was refractory to several immunosuppressive agents and whose disease entered remission with mycophenolate mofetil.9 It has been suggested that the basis for the development of PM in UC results from the common immune-mediated mechanism, in which bowel inflammation and the damage to the mucosa would lead to a release of antigens, stimulating the production of antibodies that would damage the muscle. In conclusion, the development of PM in UC should be taken into account, especially when these patients describe symptoms such as myalgia, muscle weakness or present an increase in muscle enzymes. Although there are few cases reported in the literature, it may be underdiagnosed given that the symptoms may be few and not very specific, and can be attributed to other causes.
Characteristics of the Patients With Polymyositis Associated With Ulcerous Colitis.
| Authors [Ref] | Sex | Age (years) | Associated defects | AAB | Time between the diagnosis of UC and the development of PM | Muscle groups affected | Extramuscular manifestations | Treatment | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Hernández et al.3 | M | 11 | HLA-B27 (−) Sacroiliitis | No | Simultaneous | Regions proximal to extremities and neck flexors | No | Oral prednisone 1.5mg/kg/day | Improvement of muscle manifestations |
| Evrard et al.4 | M | 33 | Not associated chronic liver disease | No | 4 years earlier | Lower extremities | Fever | Oral sulfasalazine 1.5g/day Betamethasone enemas | Improvement of bowel and muscle manifestations |
| Kaneoka et al.5 | W | 57 | Not associated liver cirrhosis | ANA 1/160 RF (+) | 11 years earlier | Torso and regions proximal to extremities and neck flexors | No | Oral prednisolone 40mg/day | UC quiescent, PM with moderate activity. Death due to liver failure |
| Chugh et al.6 | W | 78 | Esophagitis and erosive gastritis | No | 15 years earlier | Torso and regions proximal to extremities and neck flexors | Polyarthralgia | Oral prednisolone 40mg/day Oral 5-aminosalicylic acid 400mg/8h Prednisolone enemas | UC in remission, improvement of muscle manifestations |
| Voigt et al.7 | W | 33 | – | ANA 1:2.560 Anti-DNA (+) | 4 years earlier | Regions proximal to extremities | No | IV prednisolone 200mg/day for 7 days, followed by oral prednisone 60mg/day | UC quiescent, PM in remission |
AAB, autoantibodies; ANA, antinuclear antibodies; CK, creatine kinase; IV, intravascular; M, man; PM, polymyositis; Ref, reference; RF, rheumatoid factor; UC, ulcerative colitis; W, woman.
The authors declare they have no conflict of interest directly or indirectly related to the contents of this manuscript.
Please cite this article as: González García A, Sifuentes-Giraldo WA, Diz Fariña S, Pian H. Polimiositis en un paciente con colitis ulcerosa. Reumatol Clin. 2016;12:360–362.