Primary Sjögren's syndrome (pSS) is a condition that predominantly affects women. Reports of pregnancy outcome in these patients are limited and contradictory.
ObjectiveTo describe pregnancy characteristics and outcomes and newborn morbidity in women with pSS.
Material and methodsWe included women with pSS who became pregnant after the onset of the symptoms of the disease. Clinical and serological characteristics, risk factors and previous maternal comorbidities are described. For each pregnancy in a woman with pSS, we recorded pregnancy course and outcome and newborn condition.
ResultsWe assessed 11 patients with 18 pregnancies after the onset of pSS symptoms. All of them presented FAN +; 10 anti-Ro/SSA + and 7 anti-La/SSB +. The mean age in years at the onset of symptoms was 24.9 (SD 6.9) and at the time of pregnancy was 30.3 (SD 5.4). Thirteen pregnancies happened before the diagnosis, reporting only one miscarriage. Two preterm births, 1 case of oligohydramnios, 2 of premature membrane rupture and 2 low birthweight babies were reported after the onset of pSS symptoms. There was 1 newborn with congenital atrioventricular block and another with neonatal cutaneous lupus. All the women with pregnancy complications (n=6) had anti-Ro/SSA antibodies.
ConclusionsAlmost half of the pregnancies assessed in women with pSS were associated with complications not attributable to factors other than the disease.
El síndrome de Sjögren primario (SSp) afecta preferentemente al sexo femenino. Los informes sobre la evolución de los embarazos en estas pacientes son pocos y contradictorios.
ObjetivoDescribir las características del embarazo y su desenlace en mujeres con SSp, así como la morbilidad del recién nacido.
Material y métodosSe incluyeron pacientes con SSp que quedaron embarazadas luego del comienzo de los síntomas de dicha enfermedad. Se describieron las características clínicas y serológicas, los factores de riesgo y las comorbilidades maternas previas. Se detalló la evolución de cada embarazo, el desenlace y las características del recién nacido.
ResultadosSe evaluaron 11 pacientes con 18 embarazos posteriores al inicio de síntomas: todas presentaban FAN+; 10 anti-Ro/SSA+ y 7 anti-La/SSB+. El promedio de edad en años al inicio de los síntomas fue de 24,9 (DE 6,9) y al momento del embarazo fue de 30,3 (DE 5,4). Hubo 13 embarazos previos al diagnóstico, reportándose solo un aborto espontáneo. Después de la presentación del SSp, se informaron: 2 partos prematuros, un oligoamnios, 2 roturas prematuras de membranas y 2 recién nacidos con bajo peso al nacer. Se halló un caso con bloqueo cardíaco congénito y otro con lupus cutáneo neonatal. Todas las mujeres con complicaciones obstétricas (6) presentaban Ac anti-Ro/SSA+, 5 con Ac anti-La/SSB+. Quienes no tuvieron complicaciones (5): 2 presentaban anti-Ro/SSA y anti-La/SSB+, y 2 solo anti-Ro/SSA.
ConclusionesCasi la mitad de los embarazos de las pacientes con SSp analizados presentaron alguna complicación no atribuible a otro factor distinto de su enfermedad de base.
Sjögren's syndrome (SSJ) is a chronic inflammatory autoimmune disease which may present alone and is known as primary Sjögren's syndrome (pSS) or in the context of another disease of underlying connective tissue, most commonly rheumatoid arthritis (RA) or systemic lupus erythematosus (SLE), when it is known as secondary Sjögren's syndrome (sSS). This disease predominantly affects females (9:1 ratio), and has a .1%–4.8% prevalence rate in the total female population. It may begin at any age, but most frequently affects women in their forties and fifties. Due to the increase in average age for the first pregnancy in recent years, greater frequency of pSS has been observed in pregnant women.1,2
The most serious complication which may affect the children of these patients is congenital heart block (CHB), which is related to the presence of anti-Ro/SSA, anti-Ro52 and/or anti-La/SSB antibodies. An estimated rate of CHB is approximately 2%.3,4 In other autoimmune diseases such as SLE and in antiphospholipid syndrome (APS), the impact in the result of pregnancy has been well established and differentiated in accordance with the maternal disease, the course of the disease, the severity of the organ damage, the antibody profile and the treatment administered.5,6 However, in SSJ, reports on the evolution of pregnancies are limited and contradictory.7–11
The general aim of our study was to describe the characteristics of pregnancy and its outcome in women with pSS, together with the morbidity of the newborn. Specific objectives were to determine the presence of CHB, pregnancy characteristics and their outcome and the presence of complications.
We present a report on 18 pregnancies which took place after the onset of this disease symptoms.
Material and MethodsThis was a multicentre, retrospective and observational study. We reviewed the medical files of patients with SSJ from 5 rheumatology centres in Argentina. Those patients with pSS were included in accordance with AECG 200212 criteria, were over 18 years of age, attended the participating centres and had become pregnant after the beginning of symptoms suggestive of the disease. Patients were excluded if they met with the APS criteria (Sydney 2006 criteria).13 The clinical and serological traits of the disease were described together with the risk factors and previous maternal comorbidities. The development of each pregnancy was reported in detail, together with its outcome and the features of the newborn. These data were collected through pre-established records which were sent to each centre and were completed by the patients with help from their practitioner if required.
The protocol was assessed and approved by the hospital ethics committee and the patients gave their informed consent prior to completing the records.
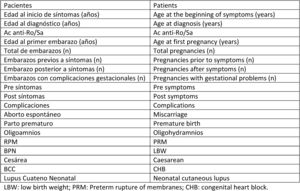
ResultsEleven patients diagnosed with pSS were included in the study, with a total of 31 pregnancies: 13 developed the beginning of symptoms of the disease before falling pregnant and 18 after. Regarding the patient characteristics (Table 1), the mean age at the beginning of symptoms was 24.3 years (SD 6.5), the mean age at diagnosis AECG 2002 criteria was 28.1 years (SD 5.6), and the age at the time of pregnancy after the development of the disease was 30.3 years (SD 5.4). With regard to serological traits, 100% (11/11) of the patients had positive antinuclear antibodies (ANA), 10/11 presented with positive specific anti-Ro/SSA antibodies and 7/11 for the anti-La/SSB antibody. In no cases was the antibody anti-Ro52 determined. The presence of positive anticardiolipin antibodies at moderate rates on 2 occasions was present in a single patient with no APA criteria being met.
Characteristics of the Population and of the Pregnancies.
| Patients n=11. Total pregnancies, n=31 | |
|---|---|
| Age at the beginning of symptoms, in years, mean (SD) | 24.3 (6.5) |
| Age at the diagnosis, in years, mean (SD) | 28.1 (5.6) |
| Age at time of pregnancy, in years, mean (SD) | 30.3 (5.4) |
| Positive anti-Ro/SSA Ab | 10/11 |
| Positive anti-La/SSB Ab | 7/11 |
| Positive ANA | 11/11 |
| Positive APA without meeting APS criteria | 1/11 |
| Pregnancies before the beginning of symptoms | 13/31 |
| Complications in pregnancies prior to the beginning of symptoms | 1/13 (7.6%) |
| Pregnancies after the beginning of symptoms | 18/31 |
| Complications in pregnancies after the beginning of symptoms | 10/18 (55.5%) |
Ab: antibodies; APA: antiphospholipid antibodies; ANA: antinuclear antibodies; SD: standard deviation; APS: antiphospholipid syndrome.
The course of the disease during pregnancy was not detailed because no standardised tool to retrospectively homogenise these data was available. Out of the 13 pregnancies which developed prior to symptom onset, only one complication was reported (1/13; 7.6%), which consisted of a miscarriage. Of those pregnancies which occurred after symptom onset (18), in 55.5% (10/18) we observed some type of complication. Of the 11 patients only 3 presented with pregnancies before and after onset of symptoms suggestive of the disease. These women presented with complications prior to the onset of symptoms of 1/13 previous total pregnancies and after onset of symptoms the complicated pregnancies were 5/5 of the total post-symptom pregnancies.
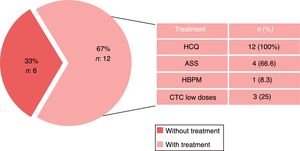
The different complications reported were in decreasing order: prolonged labour which terminated in caesarean section, preterm rupture of membranes, low birth weight and miscarriage in the first trimester. Only one case of CHA was found with a requirement for permanent pacemaker during the first month of life and one case of neonatal cutaneous lupus (Table 2). All the women with obstetric complications (6/11) presented with anti-Ro/SSA+antibodies and y 5 also had anti-La/SSB+antibodies. In the only patient with the presence of positive anticardiolipin antibodies the newborn presented with neonatal cutaneous lupus as a complication. With regard to the women who did not have any complications (5/11): 2 presented with anti-Ro/SSA and anti La/SSB +, and 2 only with the former. One patient who suffered from preterm labour with a low birth weight had a hereditary history of thrombophilia. During the course of the pregnancies, 12 of the 18 received treatment (67%). All used hydroxychloroquine (HCQ), 4 used acetylsalicylic acid (ASA) prophylactically, 3 used low dose corticoids (CTC) and one patient received low molecular weight heparin (LMWH) prophylactically (Fig. 1).
It has been well established that autoimmune diseases are clearly predominant in females, and the ages of presentation generally coincides with the reproductive years of the woman. The activity of the disease, its serological traits, and the treatments administered are possible generators of complications for both the mother and her child. In recent times due to greater knowledge of the disease and the development of more sensitive serological techniques, a lower age for the appearance of SSJ has been noted than that previously reported. This type of earlier disease has been characterised by being more aggressive in nature, with a higher frequency of extra-glandular complications and the presence of positive antibodies even prior to the appearance of symptoms of dryness.14
The most serious complication which may affect the children of patients with an autoimmune disease is CHB, which has been related to the presence of anti-Ro/SSA, anti-Ro52 and/or anti-La/SSB antibodies. These antibodies are present in SSJ, and also in SLE and in other colagenopathies. The incidence rate of CHB in our media has been estimated as approximately in 2% and 3% of all children born by women with anti-Ro/SSA and anti-La/SSB antibodies, respectively. CHB carries a high morbidity and mortality rate, with most of the children who survive this complication having to have permanent pacemakers before reaching adulthood.4–15 Maternal treatment with fluoridated steroids, plasmapheresis, immunoglobulins and sympathomimetics could reduce the inflammatory damage measured by antibodies in the nodal tissue of the newborn.16,17
In other autoimmune diseases such as in SLE and APS, the impact in the evolution and the result of the pregnancy has been well established and differentiated in accordance with the maternal disease, the activity of the disease, the severity of organ damage, the antibody profile and the treatment administered.11,12 However, in pSS the scarcity of reports on the evolution in pregnancies are contradictory. Two studies which included 21 patients report an increase in the rate of miscarriages and foetal losses, but with no relationship found with the presence of anti-Ro/SSA and/or anti-La/SSB antibodies or antiphospholipids.13,14 Other studies with approximately between 14 and 30 patients did not confirm these data, but stated that the pregnant women with pSS were of more advanced ages, there was a high rate of intrauterine growth retardation (IUGR) and newborns with lower birth weights.15,16 There was also a lower rate of normal labours.17
Coinciding with that previously published, in our work we observed that almost half of the pregnancies analysed in patients with SSJ presented with some type of complication not attributable to factors other than their baseline disease, except in the patient with thrombophilia. Our study was retrospective and therefore has several weaknesses such as the loss or inexactitude of some data, mainly due to the lack of specific details by the patients. Because it was undertaken in reference centres in a study on autoimmune disease, errors could have been made in interpretation of secondary results on a selection bias, such as the early age of presentation in our patients. On assessing only patients in rheumatology centres there are greater possibility of describing only the most severe cases, or that they are referred for consultation with the consequent underestimation of incidence and the overestimation of the severity of the presented cases. The lack of a control group of mother with similar socio-demographic characteristics and pregnancies without any autoimmune disease for comparing the presence of complications is the most poignant limitation of our study. Although we acknowledge these methodological imperfections, we believe that the pregnancies in patients with SSJ, like those with autoimmune diseases which involve positive anti-Ro (SSA or Ro52) antibodies should be considered high risk since the possibility of CHB is present. The follow-up of these patients should be undertaken by a multidisciplinary tem in the centres of reference.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that for this research no experimentation has been carried out on human beings or animals.
Confidentiality of dataThe authors declare that they have adhered to the protocols of their centre of work on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestThe authors have no conflicts of interests to declare.
Please cite this article as: Demarchi J, Papasidero SB, Klajn D, Alba P, Babini AM, Durigan V, et al. Síndrome de Sjögren primario y embarazo: reporte de 18 casos. Reumatol Clin. 2019;15:109–112.