Prosthetic knee infection by Mycobacterium tuberculosis (MT) is rare.1,2 Reviews in 2011 and 2013 found 7 and 15 cases of prosthetic infections due to MT, respectively.3–5 Since the introduction of biological treatment for rheumatoid arthritis (RA), there has been an increase in the incidence of infection by MT, mainly in patients treated with antagonists to tumor necrosis factor (anti-TNF).6,7 One study showed an MT infection rate of 49 per 100,000 person-years in patients with RA treated with anti-TNF versus 8.76,7 in patients with RA not treated with these agents. Here, we present a case of prosthetic infection by MT in a patient with RA treated with anti-TNF.
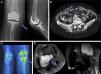
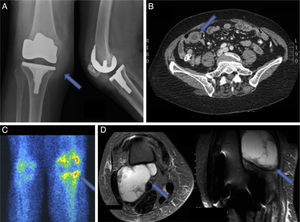
The patient is a 77-year-old woman who had RA treated with methotrexate 7.5mg/weekly and infliximab (IFX) 3mg/kg, and a right knee prosthesis. In March 2012 she developed cough, and fever with nightly sweating lasting for 2 months; BK and sputum culture were requested, both negative. She received IFX in May and in June went to a review visit referring multiple respiratory infections during that time. In August she was assessed by Orthopedics, finding fever, pain and swelling of the right knee; discharged with a suspected prosthetic infection (Fig. 1A). In November, she was hospitalized in Internal Medicine (IM) for partial bowel obstruction and was discharged on prednisone 15mg/day; during admission, a computed tomography (Fig. 1B) was performed, showing a pulmonary nodule indicative of granuloma and chest and retroperitoneal lymphadenopathy. In January 2013 she came to the Rheumatology clinic due to knee pain, and IFX was suspended; she also was assessed by IM, who recommended surgery for the persistent intestinal subocclusion. In April, she was evaluated by General Surgery and operated. Pathologic examination showed necrotizing granulomatous lymphadenitis and necrotizing granulomatous inflammation and ulceration of the mucosa in the small intestine; microbiological study was negative for Mycobacterium. Rifater® was begun and QuantiFERON® performed, which was negative. In June, she went to Rheumatology for leg edema and pain in the right knee; Doppler ultrasound was performed, showing a cystic mass of 10cm, which was drained and analyzed; an MRI was also requested (Fig. 1D). The drained fluid PCR was positive for Mycobacterium tuberculosis complex. During this period, the patient had slightly higher acute phase reactants; Orthopedics also performed a scintigraphy, suggestive of periprosthetic infection (Fig. 1C). Currently, Orthopedics dismissed surgery and the patient continues on a tuberculostatic.
Prosthetic infection MT may be a reactivation of a latent focus that reaches the joint by hematogenous or local reactivation.8,9 Risk factors for prosthetic infection are: RA or other immunosuppressive conditions, peri- and postoperative joint infections, non-adjacent previous infection, previous surgery on the same joint, prolonged surgery, higher body mass index, postoperative hematoma, advanced age and diabetes mellitus.10 Risk factors for MT prosthetic infection are: advanced age (>70 years), past MT infection and immunosuppressive conditions.5
Treatment usually is medical and surgical; it is recommended to obtain tissue samples or pre-antibiotic liquid; if the patient has a poor clinical condition, we recommend starting vancomycin and cephepime.11 The surgery depends on: etiology, time of the infection presentation from the implantation of the prosthesis and comorbidities. Surgical options include prosthetic replacement (in one or two [the recommended] times), debridement and retention of the prosthesis and prosthetic resection in case a reimplantation is not contemplated.11 A study in patients with RA and prosthetic infection concluded that prosthetic replacement in 2 times has a better prognosis.12 The choice of surgery in MT infection is controversial for the few cases reported.6 6–9 months of treatment are recommended for osteoarticular tuberculosis (2 months of isoniazid, rifampicin, pyrazinamide and ethambutol, followed by 4–7 months of isoniazid and rifampicin),12 but can vary according to the patient characteristics and outcomes between 6 and 24 months.11
This patient had a prosthetic infection secondary to a tuberculosis, but we recommend, according to the literature, a combined treatment: prosthetic replacement in 2-times and 4-tuberculosis drugs for a minimum of 6 months.
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Egües Dubuc C, Uriarte Ecenarro M, Errazquin Aguirre N, Belzunegui Otano J. Infección protésica por Mycobacterium tuberculosis en paciente con artritis reumatoide: reporte de un caso y revisión bibliográfica. Reumatol Clin. 2014;10:347–349.