The patient was a 77-year-old woman who been complaining of a history of several months of pain and functional impotence, due to discomfort involving the abduction and internal rotation of her right shoulder. It had improved, but had gotten worse in the last 2 weeks.
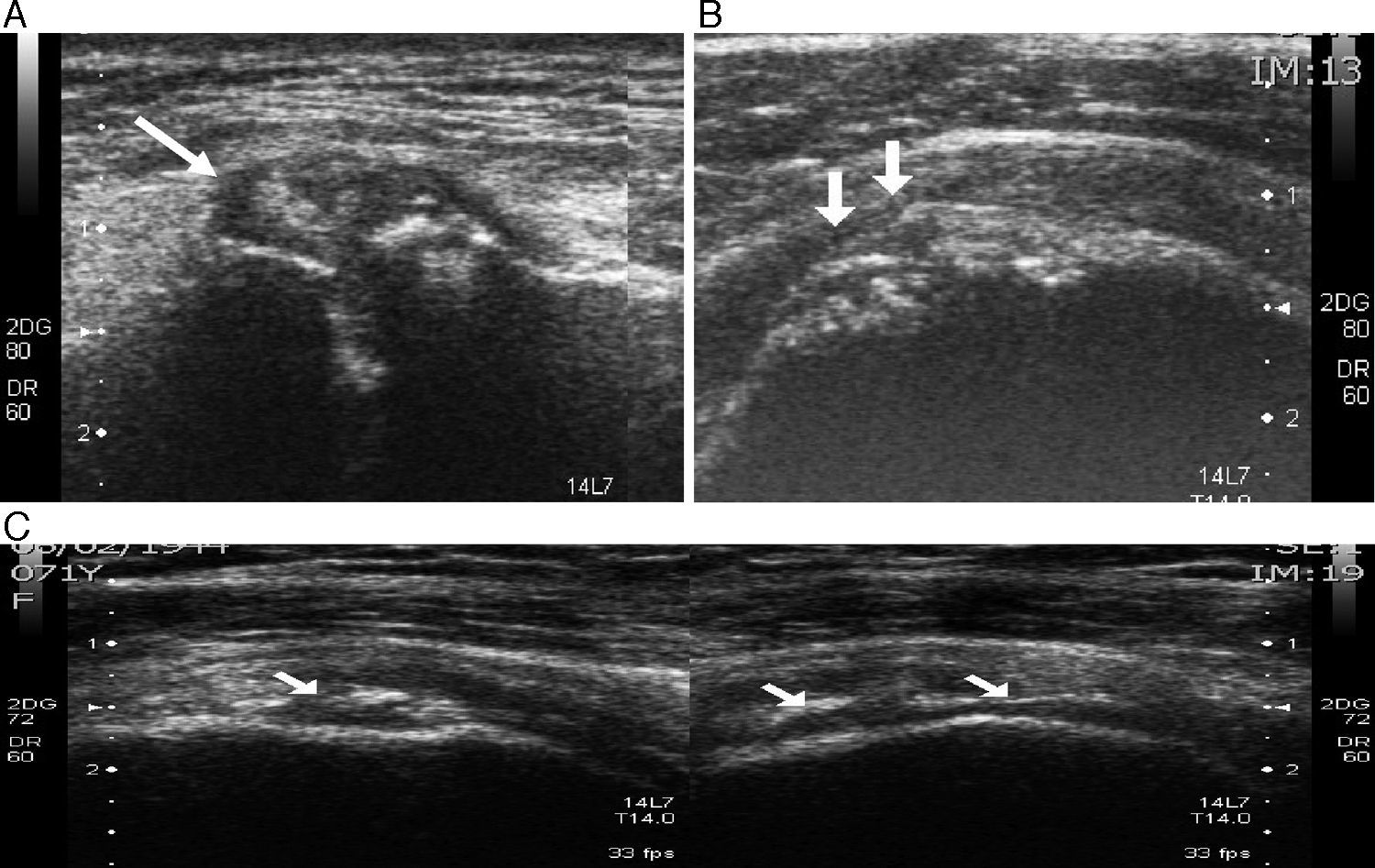
In the ultrasound performed initially to exclude involvement of the rotator cuff (Fig. 1), there are signs of supraspinatus tendinopathy, with a small partial rupture and the characteristic calcifications of pyrophosphate depositions in the acromioclavicular joint and in the cartilage of the humeral head, following its outline.
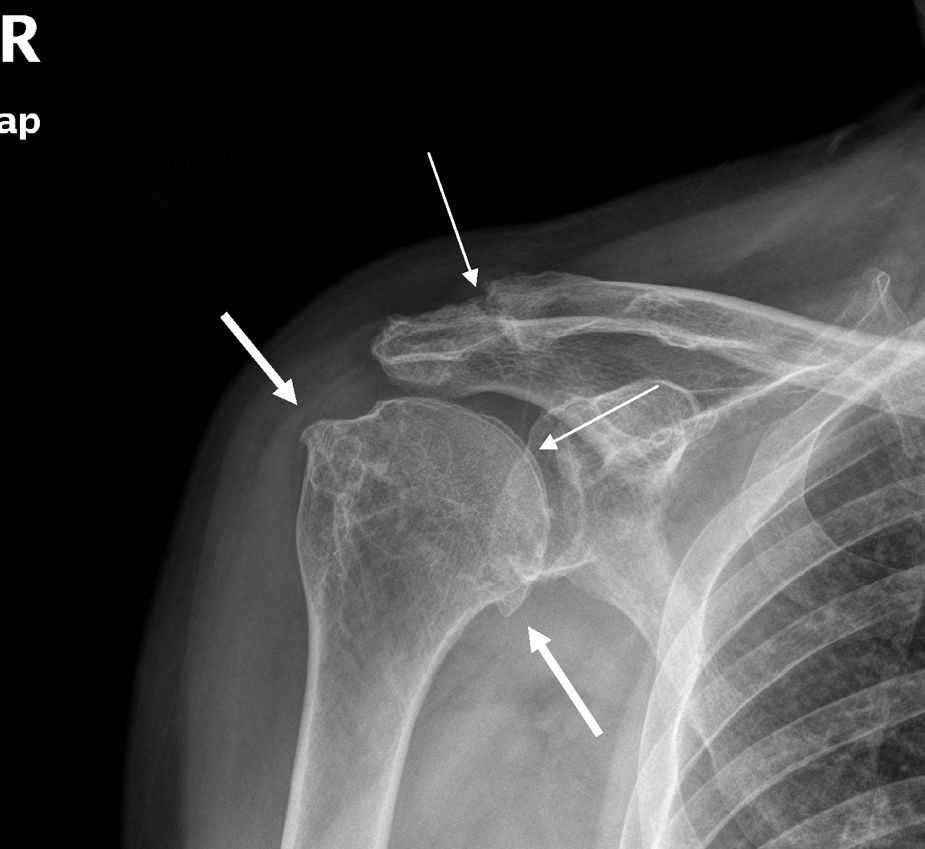
Plain radiography (Fig. 2) from that moment shows degenerative changes in the glenohumeral joint, and also reveals chondrocalcinosis of the humeral cartilage and the acromioclavicular joint.
The deposits of calcium pyrophosphate occur just inside or, surrounding the joints, where there are calcifications in the thickness of joint cartilages, menisci, synovial and periarticular tissues.1,2 Although, the deposit of pyrophosphate crystals has nearly no hyaline cartilage or fibrocartilage. However, areas of chondroid metaplasia have also been found to have extraarticular deposits similar to tophi, as in tendons or bursa.
However, the crystal deposits in cartilage are not made exclusively of pyrophosphate, and have been reported in the case of monosodium urate.3
These deposits (chondrocalcinosis) can be asymptomatic, become associated with degenerative joint manifestations, or produce acute episodic arthritis (pseudogout).1
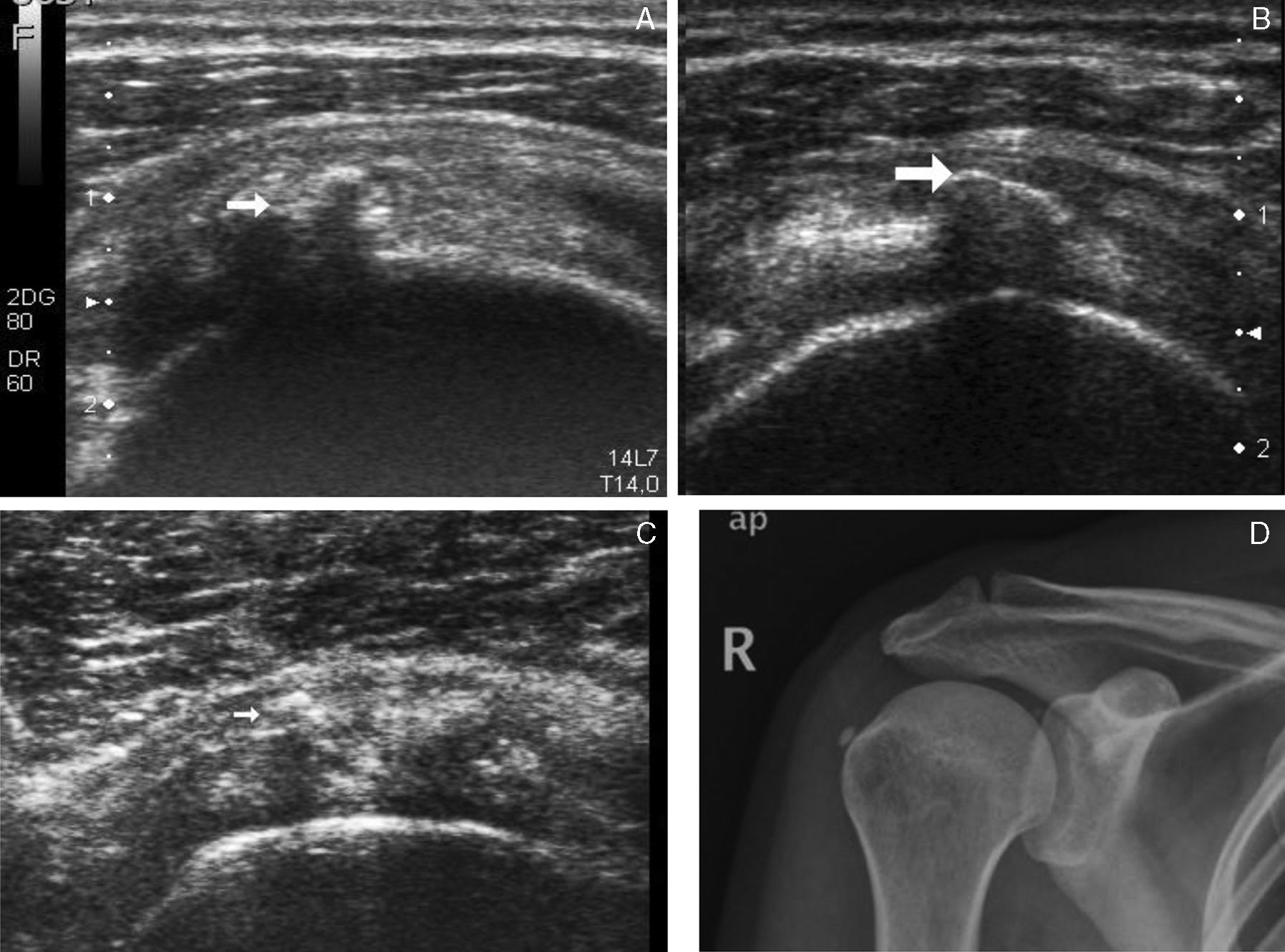
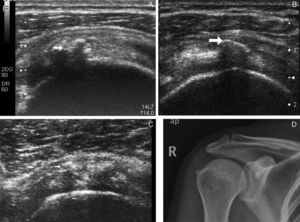
They should be differentiated from calcific tendinitis, mainly through the presence in the deposit of hydroxyapatite (and, less frequently, monosodium urate or calcium pyrophosphate),3 in which the crystal deposit is intratendinous, and can produce the rupture of the base of the tendon, and extend to the interior of the subacromial bursa (Fig. 3).
Arthropathy for a hydroxyapatite deposit. (A) Intratendinous calcifications (see arrow). (B) Calcification in floor of the subacromial bursa. (C) Small calcifications in anterior portion of the supraspinatus tendinopathy and 1 (see arrow) in the interior of the subacromial bursa. (D) Plain radiography of tendinous calcification of supraspinatus.
Both processes are susceptible to being diagnosed early by means of ultrasound, as the latter tends to evaluate the, characteristic site and extension of the calcifications.4,5 Plain radiography, also makes it possible to differentiate the degenerative changes in the glenohumeral joint, using arthropathy for pyrophosphate and an arthropathy for a rotator cuff tear.2,4–7
The prevalence of 3.7%–17.5% for radiological chrondrocalcinosis (according to the age group being used as a reference),1 and the 2.7%–20% for the calcic tendinopathy.8 Although, in our experience, pyrophosphate deposition (3/1) is much more probably due to the early detection of calcified acromioclavicular joint in the ultrasound.
ConclusionThe clinical entity referred to as the “sore shoulder” should probably be approached by a series of specialists, because of the frequency with which the diagnostic is delayed. It can also be based on an incorrect diagnostic information, meaning that the therapeutic approach becomes more difficult. Likewise, a multitude of imaging techniques, may be requested, and some may not be necessary.
Ultrasound and radiography of the shoulder, when verified together, make it easier to approach the management of the sore shoulder. Moreover, they provide an adequate and early differential diagnosis.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Román Sastre MM, Vega González ML. Artropatía por pirofosfato cálcico como causa de hombro doloroso: valor de la ecografía en el abordaje diagnóstico. Reumatol Clin. 2016;12:351–353.