Fever is a diagnostic challenge in the patient with lupus. Infections can mimic a lupus flare which further complicates the diagnostic approach. Moreover, immunosuppressive treatment of SLE may promote the development of infections and poor outcome. We report the case of a patient with SLE with an initial diagnosis of lupus flare, who was found to have Q fever showing an excellent response to treatment with doxycycline.
La fiebre constituye un reto diagnóstico en el paciente lúpico. Algunas infecciones pueden imitar un brote de la enfermedad, lo que complica aún más la orientación diagnóstica. Por otra parte, el tratamiento inmunodepresor del lupus eritematoso sistémico (LES) puede favorecer la aparición de infecciones y su mala evolución. Presentamos el caso de una paciente con LES en tratamiento con antipalúdicos y dosis bajas de esteroides, cuyo diagnóstico inicial fue de brote lúpico y que resultó tener fiebre Q, presentando una respuesta excelente al tratamiento con doxiciclina.
The presence of fever in a patient with SLE is a diagnostic challenge as the two main causes of it, the reactivation of the disease or infection, require very different1 therapeutic actions.2 Q fever is an infectious disease of worldwide distribution, caused by Coxiella burnetii (C. burnetii).3 The usual clinical manifestations of the acute form include fever, headache, asthenia, sweating, chills and frequent musculoskeletal pain and gastrointestinal symptoms, all common in lupus outbreaks. We describe a patient with SLE, who was diagnosed with Q fever in what appeared to be a lupus flare.
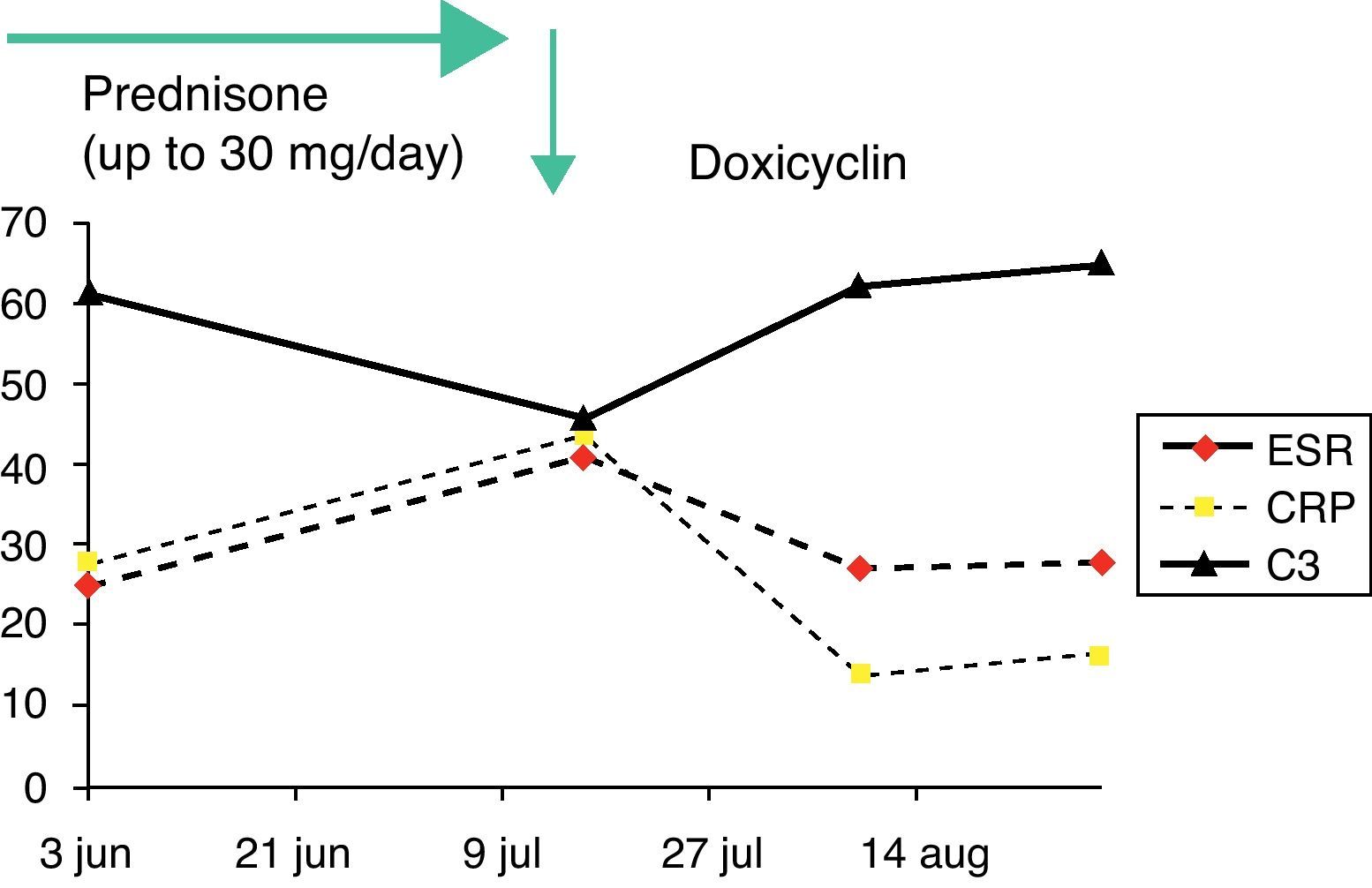
Clinical ObservationA 176-year-old woman was first seen by the rheumatology consultation in September 2008 in connection to thrombocytopenia and positive antinuclear antibodies (ANA). In November 2009, the diagnosis of SLE due to the presence of polyarthritis, leukopenia, and anti-DNA antibodies (titer of 1/80) was made. She was treated with deflazacort (6mg/day) and presented significant improvement of the arthritis and, later, treatment was begun with hydroxychloroquine (300mg/day) and nonsteroidal antiinflammatory drugs in varying doses and she remained virtually asymptomatic in the following months. She remained in remission until the end of May 2010, but developed fever of up to 39°C, with no clear chronological pattern, musculoskeletal pain and stiffness with doubtful signs of arthritis, loss of appetite, malaise and sore throat. Physical examination was normal except for some pharyngeal hyperemia, but cardiopulmonary examination was normal and the abdomen was soft and without organ enlargement. In the initial analysis we carried out, she had a hemoglobin of 10.5g/dl and 3700 leukocytes. The ESR was 41 and CRP 4.33mg/dl, complement fractions C3 46mg/dl (NV: 90–180) and C4 of 3mg/dl (NV: 10–40). The urinary sediment presented 1–5 cells/field without proteinuria and transaminases were normal. The chest X-ray was normal. Based on clinical and laboratory data and waiting for the other microbiological data requested, deflazacort was substituted by prednisone (30mg/day), due to the suspicion of a lupus flare. In the next 7 days we observed a slight reduction of fever and improvement of musculoskeletal pain, but in later days these symptoms were reactivated. The results of microbiological studies were negative for major viral infections (including hepatotropic virus, Epstein-Barr virus, cytomegalovirus and human immunodeficiency virus) and positive for C. burnetii phase II IgG 1/16384 (titers above 1/256 show active or recent infection) and IgM 1/64 (titles showing active infection are at or above 1/32), at which point we started doxycycline 100mg. Every 12h for 14 days, which began about 3 weeks after the process’ onset, and led to complete relief of the symptoms, with the patient being virtually asymptomatic after 5 days of antibiotic and with progressive normalization of acute phase reactants, as shown in Fig. 1. The serological testing performed at 3 weeks showed a negative result for IgM and a significant reduction of IgG (1/2048). Given the good outcome, no echocardiogram was performed and treatment was continued with hydroxychloroquine (300mg/day) and prednisone (5mg/day).
DiscussionIn patients with SLE, fever is a common symptom and distinguishing between an infection or lupus flare is sometimes a challenge. It has been suggested that elevated CRP levels (above 6mg/dl) are highly suggestive of infection and may be of help,4,5 and typical data of SLE activity, such as complement decrease or increased activity of SLE measured by the SLEDAI1 index, may be absent. On the other hand, the use of high doses of steroids in lupus patients with infection might be fatal, hence the importance of differentiating both. As previously described by Ohguchi et al.,6 the existence of Q fever might present with clinical and even biological SLE data and has an excellent response to antibiotic treatment and no further testing is needed to confirm SLE. In our case, we had a previous diagnosis of SLE, defined on the basis of clinical and laboratory data and, later, the patient developed nonspecific clinical signs and symptoms that could respond to both infection or a reactivation of SLE. Q fever is a universal zoonosis and infected animals excrete the organism in the feces, urine and milk. The usual route of human infection is inhalation of pseudoespores. It is asymptomatic in many patients (up to 50% in some series) and most cases occur as an acute process,7 which presents with fever and general symptoms such as pneumonia or liver disease, although in our case these complications did not occur. The differential diagnosis is broad, given the nonspecific symptoms, and the use of diagnostic criteria is aimed at the recognition of Q fever-associated endocarditis. The microbiological diagnosis by culture can be direct, but its sensitivity is very low, so one commonly resorts to indirect techniques, among them one of the most widely used is indirect immunofluorescence, which shows a 97% sensitivity and specificity of 100% for phase II IgG in some studies.8 In acute infection, it is common to find elevated antibody titers to phase II antigens, while those directed to phase I antigens are more characteristic of chronic infection. Test results can be misleading in the presence of rheumatoid factor, which was not present in our patient. Cross reactions with other microorganisms, such as Legionella, Bartonella and Ehrlichia, can be seen, although these seem more common in chronic forms of Q fever. The clinical differences and regional distribution can help in the differential diagnosis.
ConclusionsThe main interest of this case is to consider Q fever as a causal factor of fever and other symptoms that are similar to a lupus outbreak in a patient with SLE, especially in endemic areas where the infection is common, and where an appropriate therapeutic intervention is crucial.
DisclosuresThe authors have no disclosures to make.
Please cite this article as: Hernández Beriain JÁ, et al. La fiebre Q puede simular un brote lúpico. Reumatol Clin. 2012;8:143–4.