In recent years, outpatient clinics have undergone extensive development. At present, patients with rheumatic diseases are mainly assisted in this area. However, the quality standards of care are poorly documented.
ObjectiveTo develop specific quality criteria and standards for an outpatient rheumatology clinic.
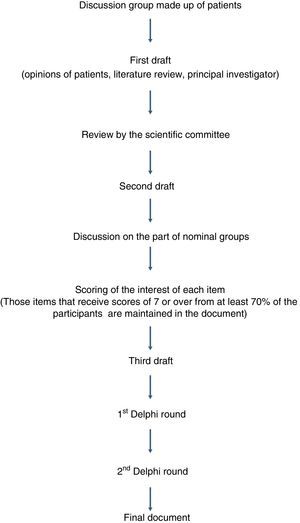
MethodThe project was based on the two-round Delphi method. The following groups of participants took part: scientific committee (13 rheumatologists), five nominal groups (45 rheumatologists and 12 nurses) and a group of discussion formed by 9 patients. Different drafts were consecutively generated until a final document was obtained that included the standards that received a punctuation equal or over 7 in at least 70% of the participants.
Results148 standards were developed, grouped into the following 9 dimensions: (a) structure (22), (b) clinical activity and relationship with the patients (34), (c) planning (7), (d) levels of priority (5), (e) relations with primary care physicians, with Emergency Department and with other clinical departments, (f) process (26), (g) nursing (13), (h) teaching and research (13) and (i) activity measures (8).
ConclusionThis study established specific quality standards for rheumatology outpatient clinic. It can be a useful tool for organizing this area in the Rheumatology Department and as a reference when proposing improvement measures to health administrators.
En los últimos años, el peso específico de las consultas externas ha aumentado considerablemente. En la actualidad, la mayor parte de la atención reumatológica se lleva a cabo en esta área del hospital. Sin embargo, apenas existe documentación respecto a estándares de calidad asistencial.
ObjetivoDesarrollar, mediante consenso, estándares de calidad asistencial específicos para las consultas externas de reumatología.
MétodoEl proyecto se llevó a cabo mediante metodología Delphi a 2 rondas. Se contó con la participación de un comité científico (13 reumatólogos), 5 grupos nominales (45 reumatólogos y 12 enfermeras especializadas) y un grupo de discusión formado por 9 pacientes. Se generaron de forma sucesiva diversos borradores hasta obtener un documento final que incluyó los estándares que recibieron una puntuación igual o superior a 7 en al menos el 70% de los participantes.
ResultadosEl documento consta de 148 estándares distribuidos en 9 áreas temáticas: a) estructura (22); b) actividad clínica y relación con los pacientes (34); c) planificación (7); d) niveles de prioridad (5); e) relación con atención primaria, con el servicio de urgencias y con otros servicios del hospital (20); f) proceso (26); g) enfermería (13); h) docencia e investigación (13), e i) cómputo de actividad (8).
ConclusiónSe han consensuado unos estándares de calidad asistencial que pueden ser útiles para organizar la actividad en las consultas externas de los servicios de reumatología y servir como marco de referencia a la hora de elevar propuestas de mejora a la gerencia del hospital o a otros estamentos de la administración.
At the present time, from the point of view of clinical management,1 the outpatient clinic is not thought of as an element that merely lends support to the hospitalization setting, but as an autonomous mechanism that enables the orderly flow of patients and guarantees continuity with primary care.
Rheumatology care is mostly centered in the ambulatory area (outpatient clinics and day hospitals). Undoubtedly, at a time in which administrations promote formulas that offer an alternative to hospital admission,2–5 the determination of rheumatology to wager on outpatient activity lends added value to the specialty.
Nevertheless, to a great extent, the health care field continues to measure the relative importance of a clinical discipline on the basis of the work of its professionals in the hospital wards. This is due, to a great extent, to the fact that the indicators of activity and quality of care standards focus on the process of hospital admission and hardly take into account the work done in the ambulatory setting. The availability of indicators and standards that guarantee the quality of the care provided in this area and reveal the true scope of the services it offers is essential to achieve the recognition of the importance of specialties, like rheumatology, that are not necessarily involved in the admission of patients.
In Spain, there are two documents, one drawn up in 2002 by the Society of Rheumatology of the Community of Madrid (SORCOM)6 and the other issued by the Spanish Society of Rheumatology (SER) in 2007,7 that establish the standards for quality in rheumatology care. These documents are highly useful when it comes to organizing and administering rheumatology departments, but they are general in nature, not specific for the outpatient setting. Moreover, they do not evaluate in depth some of the health care dynamics that have been gaining in importance in recent years.
In the ambulatory care setting, a number of articles have been published over the last few years concerning the activity that takes place in rheumatology day hospitals. Their performance has been evaluated in different departments in Spain,8 the situation in the Valencian Community has been analyzed—and proposals for improvement have been put forward9—and, recently, the Working Group on Day Hospitals of the SER defined a set of quality of care standards for this area.10 In contrast, none of the existing documents refer specifically to the activity carried out in the outpatient clinics.
The objective of the strategy we present, the EXTRELLA project, was to establish, by consensus, quality of care standards for rheumatology outpatient clinics. The EXTRELLA project participates in the program of the Plan ICARO for the improvement of the quality of care in rheumatology, a project of the SER (http://www.ser.es/investigacion/Proyectos/Icaro/icaro.php) that works toward the development of quality standards for their implementation in clinical practice.
MethodsThe work, initiated in January 2013, was carried out with the participation of: (a) a scientific committee made up of 13 rheumatologists (a principal investigator and 12 research collaborators); (b) 5 nominal groups, which included a total of 57 rheumatology professionals (45 rheumatologists and 12 nurses specialized in rheumatology); and (c) a discussion group made up of patients. Methodological and logistic support was provided by the Research Unit of the SER (RU-SER).
Fig. 1 shows the dynamics of the project that led to the generation of the final document.
The project commenced with the constitution of a discussion group of patients, for the purpose of gathering their opinions on the care they received in the rheumatology outpatient clinics and to identify quality of care criteria that could be taken into account in the subsequent work with the professionals. The group consisted of 5 women and 4 men, ranging in age between 40 and 72 years, who had a variety of rheumatic diseases and had been being treated for at least 2 years in different hospitals of the Community of Madrid. A meeting of the group was called, in which the moderator was a methodologist from the RU-SER. The subjects for debate were structured, on the basis of a preestablished outline, in 4 major groups: (a) self-perception of health and disease; (b) access to a specialist, the visit and follow-up; (c) perceived satisfaction with the care received; and (d) suggestions for the improvement of patient care.
After that, the principal investigator drew up a first draft of the document, incorporating the contributions of the patient discussion group and the information provided by a systematic literature search performed by the RU-SER. The remaining members of the scientific committee reviewed this first draft and, with their opinions and suggestions, a second draft was drawn up, which was the version that was discussed in the nominal groups.
Two types of nominal groups were established: (a) with specialists in rheumatology (4 groups) and (b) with nurses specialized in rheumatology (1 group). The rheumatologists were selected taking into consideration gender parity (23 men and 22 women), geographic distribution that was equitable and proportional to the population of each Spanish autonomous community (8 from Andalusia, 7 from Catalonia, 6 from the Community of Madrid, 5 from the Valencian Community, 3 from Galicia, 2 each from the Canary Islands, Castile-La Mancha, Castile and León, and the Basque Country, and 1 each from Aragon, the Principality of Asturias, the Balearic Islands, Cantabria, Extremadura, La Rioja, the Region of Murcia and the Chartered Community of Navarre), type of hospital (15 level 1 or basic hospitals, 15 level 2 or referral hospitals and 15 level 3 or high-technology hospitals), and professional position (31 associate physicians, 9 section heads and 5 department heads). The nurses worked in hospitals in Andalusia (n=2), Aragon (n=1), the Canary Islands (n=1), Catalonia (n=2), the Valencian Community (n=2), the Community of Madrid (n=2), Galicia (n=1) and the Basque Country (n=1); of these, 2 worked in level 1 hospitals, 3 in level 2 hospitals and 7 in level 3 hospitals.
The discussion of the second draft was held in a series of 5 meetings—which required the attendance of the participants—one with each nominal group, in which the principal investigator put forward each of the items of the questionnaire and encouraged debate on them.
Once these sessions with the presence of the participants had been held, and after a period of reflection of approximately 3 weeks, each of the participants rated the interest of each item in the second draft on a scale of 0–10 (0: absolutely no interest; 10: maximum interest), and they also filled out those items that required a numeric expression. They were offered the possibility of not scoring those items in which they considered that they did not have a solidly based opinion on the content.
After that, the scores for each item were analyzed. Those items that received scores of 7 or over from at least 70% of the participants were maintained in the document and the rest were eliminated. Thus was generated a third draft in which new items were included, fruit of the contributions of the nominal groups, and in which the text of some of them were slightly modified.
This third draft was subjected to a first Delphi round, with the participation of the 58 specialists in rheumatology (45 from the nominal groups and 13 from the scientific committee) and the 12 nurses involved in the project. Each participant rated the interest of each item on a scale of 0–10. The mean, standard deviation, coefficient of variation (CV), median, 25th and 75th percentiles and interquartile range were calculated. After the results had been evaluated in the RU-SER, the items with a score of 7 or over from at least 70% of the participants, with an interquartile range of less than 4, went on to form part of the final document.
Those items that did not achieve a score of 7 or over from at least 70% of the participants and those that had an interquartile range greater than 4 were included in a second Delphi round. Subsequently, the items that achieved a score of 7 or over from at least 70% of the participants were added to the final document.
The CV was categorized according to the following cutoff points: (a) CV less than or equal to 25%=very low variability; (b) CV greater than 25% and less than or equal to 50%=low variability; (c) CV greater than 50% and less than or equal to 75%=intermediate variability; d) CV greater than 75% and less than or equal to 100%=high variability; and (e) CV greater than 100%=very high variability.
ResultsThe consensus document comprises 148 standards distributed in 9 subject areas: (a) structure (n=22), (b) clinical activity and relationship with the patients (n=34), (c) planning (n=7), (d) levels of priority (n=5), (e) relationship with primary care, with the emergency department and with other departments of the hospital (n=20), (f) process (n=26), (g) nursing (n=13), (h) teaching and research (n=13) and (i) calculation of the activity (n=8).
One hundred eight items (73%) received a score of 7 or over from 90% or more of the participants; in 34 (23%), the percentage ranged between 80% and 89%, and in 6 (4%), between 70% and 79%. In 125 standards (84%), the CV was less than or equal to 25%.
Tables 1–9 show the consensus standards in each of the subject areas. The percentage of participants who gave a score of 7 or over is indicated, as are the mean, standard deviation, median and CV of the scores. The hard copy edition includes Tables 1–3; the online edition provides all 9 Tables (Supplementary material).
Quality of Care Standards for Structure.
| %≥7 | Mean | SD | Median | CV (%) | |
|---|---|---|---|---|---|
| The zone of outpatient clinics should be accessible, free of architectural barriers that create difficulties for the mobilization of patients with disabilities | 100 | 9.6 | 0.7 | 10 | 7.3 |
| The zone of outpatient clinics should be staffed by a sufficient number of auxiliary personnel (orderlies) to guarantee the mobility in wheelchairs of patients with disabilities | 94 | 8.8 | 1.3 | 9 | 14.8 |
| The zone of outpatient clinics should be equipped with lavatories adapted to patients with disabilities | 97 | 9.4 | 0.9 | 10 | 9.6 |
| The zone of outpatient clinics should have a system of climate control to ensure an adequate room temperature | 96 | 8.8 | 1.4 | 9 | 15.9 |
| The zone of outpatient clinics should have information panels with changeable messages to help guide the patients | 87 | 8.1 | 1.4 | 9 | 17.3 |
| The zone of outpatient clinics should have an information desk staffed by trained personnel to which patients can turn to resolve their doubts | 93 | 8.9 | 1.4 | 9 | 15.7 |
| In the zone of outpatient clinics, the administrative areas should be clearly differentiated from the clinical areas | 90 | 8.5 | 1.4 | 9 | 16.5 |
| In the zone of outpatient clinics, the management of the agendas should be computerized | 99 | 9.3 | 1.1 | 10 | 11.8 |
| The zone of outpatient clinics should have an automatic reception system based on the Individual Health Card | 84 | 7.9 | 2.1 | 8 | 26.6 |
| The zone of outpatient clinics should have an electronic system that indicates, via the physician's agenda, the arrival of a patient in the waiting room | 84 | 7.9 | 2.1 | 8 | 26.6 |
| In the zone of outpatient clinics, the waiting rooms should be spaces differentiated from the corridors leading to the offices | 91 | 8.5 | 1.4 | 9 | 16.5 |
| In the waiting rooms of the rheumatology clinics, the chairs should be ergonomic, suitable for patients with disabilities | 87 | 8.2 | 1.6 | 8 | 19.5 |
| In the waiting rooms of the rheumatology clinics, there should be at least 6 chairs for each office | 84 | 8 | 1.5 | 8 | 18.7 |
| The waiting rooms of the rheumatology clinics should have a space of at least 10m2 for each office | 87 | 8.2 | 1.9 | 9 | 23.2 |
| The minimum furnishings in the offices of the clinics should be: a telephone, a computer, a printer, a table, an office armchair for the health care professional, 4 chairs, a stool, an examination bed of adjustable height with a roll of paper, a cart or auxiliary table, a folding screen or a curtain, coat hooks, a closet and a hand basin. | 99 | 8.9 | 1 | 9 | 11.2 |
| The minimum clinical material in the offices of the rheumatology clinics should be: a blood pressure monitor, an X-ray viewer, a weighing scale, a height rod, and material to perform local injections, arthrocentesis and wound care | 97 | 9 | 1.5 | 9 | 16.7 |
| Each office of the rheumatology clinics should be equipped with electronic infrastructure that enables connection to the Internet, with the possibility of access to an online library | 100 | 9.6 | 0.8 | 10 | 8.3 |
| Each office of the rheumatology clinics should be equipped with electronic infrastructure that enables access to the data in the computer network of the hospital and health area | 100 | 9.7 | 0.6 | 10 | 6.2 |
| Each office of the rheumatology clinics should measure at least 15m2 | 94 | 8.9 | 1.3 | 9 | 14.6 |
| An administrative assistant in the rheumatology clinics should attend to a maximum of 4 offices | 80 | 7.7 | 2.1 | 8 | 27.2 |
| The structural requirements of the rheumatology clinics should be the same, regardless of whether they are located in the hospital or in a specialty center | 99 | 9.3 | 1 | 10 | 10.7 |
| The rheumatology clinics should be well-ventilated and receive natural lighting | 93 | 9.0 | 1.7 | 10 | 18.9 |
%≥7, percentage of participants who rated the item with a score of 7 or higher; CV (%), coefficient of variation expressed as a percentage; SD, standard deviation.
Quality of Care Standards for Clinical Activity and Relationship With the Patients.
| %≥7 | Mean | SD | Median | CV (%) | |
|---|---|---|---|---|---|
| The maximum time spent by the patient in the waiting room beyond the time of the appointment should be 30min | 82 | 8.1 | 1.9 | 9 | 23 |
| To protect their intimacy, patients in the waiting room should be notified of their turn by means of an information panel that doses not identify them by name | 72 | 7.3 | 2.2 | 7 | 30 |
| The medical record should have electronic support | 99 | 9.2 | 1.0 | 10 | 11 |
| The electronic medical record should be incorporated into an integrated system that enables access to all the information referring to the care of the patient (primary care, specialized care, hospital admissions, emergency department) | 100 | 9.6 | 0.6 | 10 | 7.5 |
| In a first rheumatology visit, the minimum data set that should be available are: (a) reason for consultation; (b) medical history; (c) physical examination; (d) ancillary examinations (provided by the patient and ordered); (e) proposed diagnosis; (f) therapeutic recommendations; and (g) need for follow-up and recommended duration or discharge | 100 | 9.5 | 0.7 | 10 | 7.4 |
| In an outcome visit, the minimum data set that should be available are: (a) record of incidences since the previous visit; (b) assessment of the ancillary examinations; (c) opinion of the clinical status of the patient; (d) diagnosis; (e) therapeutic recommendations; and (f) need for follow-up and recommended duration or discharge | 100 | 9.5 | 0.8 | 10 | 8.4 |
| In a subsequent rheumatology visit, the minimum data set that should be available are: (a) record of incidences since the previous visit; (b) physical examination; (c) opinion of the clinical status of the patient with respect to the previous visit; (d) therapeutic recommendations; (e) need for follow-up and recommended duration or discharge | 97 | 9.2 | 1.6 | 10 | 17.4 |
| At the end of the visit, the rheumatologist should prescribe the medication, preferably via electronic prescription, and ensure that the patient has understood the therapeutic plan initiated | 100 | 9.3 | 0.9 | 10 | 9.7 |
| In the rheumatology clinics, the patient will be informed of the next appointment immediately after the rheumatologist has ended the visit | 93 | 8.6 | 1.5 | 9 | 17.4 |
| The discharge process will necessarily require the preparation of a written report which will be given or sent to the patient and will be accompanied by the electronic medical record | 96 | 9.2 | 1.2 | 10 | 13 |
| In a discharge report, the minimum data set that should be included are: (a) the reason for consultation; (b) relevant past medical history; (c) current history; (d) physical examination; (e) ancillary examinations; (f) diagnosis; (g) therapeutic plan; and (h) specific instructions for the family physician | 99 | 9.2 | 1 | 10 | 10.9 |
| Patient care activity in the rheumatology clinics should follow established protocols to reduce the variability in clinical practice | 96 | 8.6 | 1.2 | 9 | 14 |
| The data included in the medical records should be in accordance with the clinical practice guidelines for the specialty of rheumatology | 97 | 8.9 | 1.1 | 9 | 12.4 |
| The rheumatology department should adopt a diagnostic coding system to identify the diseases being treated and evaluate the department's activity | 93 | 8.8 | 1.4 | 9 | 15.9 |
| The rheumatologist should inform the patient of the relevant aspects of his or her disease (diagnosis, prognosis and therapeutic plan) | 100 | 9.5 | 0.7 | 10 | 7.4 |
| The rheumatologist should ensure that the patient understands the relevant aspects of his or her disease (diagnosis, prognosis and therapeutic plan) | 97 | 9.1 | 1.2 | 9 | 13.2 |
| In the rheumatology clinics, unless something unexpected comes up, the patient should be attended to by the same rheumatologist | 97 | 8.9 | 1.3 | 9 | 14.6 |
| All of the patients attended to in the rheumatology clinics should be given an individual appointment at a specific time to avoid their having unnecessary waits | 93 | 8.9 | 1.4 | 9 | 15.7 |
| The patients should be asked to inform the center if they are going to miss an appointment, so that another patient can be attended to | 96 | 9 | 1.5 | 10 | 16.7 |
| The patient should know what telephone number to call to cancel or reschedule appointments | 97 | 9.2 | 1.5 | 10 | 16.3 |
| The patients should be guaranteed rapid access to the rheumatology clinics if their disease worsens or unexpected events arise | 94 | 9.1 | 1.5 | 10 | 16.5 |
| The patients should know what telephone number they should call to consult matters related to their disease and the treatment | 94 | 8.9 | 1.4 | 9 | 15.7 |
| It is recommendable that hours be established for consultation by phone to minimize the impact on the health care activity | 94 | 9 | 1.2 | 9 | 13.3 |
| All the members of the department of rheumatology should abide by the uniformity of the center and wear an identification card with their personal data where it can be easily seen | 90 | 8.6 | 1.6 | 9 | 18.6 |
| The rheumatology clinics should be able to provide informative pamphlets and webpages where the features of the different rheumatic diseases and their treatment are explained | 77 | 7.7 | 1.8 | 8 | 23.4 |
| Patient satisfaction with the care received in the rheumatology clinics should be evaluated periodically by means of questionnaires on perceived quality and the analysis of claims and suggestions formulated in the Office for Attention to the User | 81 | 7.7 | 2 | 8 | 26 |
| In the zone of outpatient clinics, there should be specific information on the existence in the center of an Office for Attention to the User and Social Work Office | 81 | 7.7 | 1.9 | 8 | 24.7 |
| The door of every office of the rheumatology clinics should bear the name of the rheumatologist or nurse who will be attending to the patients | 88 | 8.3 | 1.7 | 8 | 20.5 |
| It is advisable that the rheumatology clinics receive visits in the afternoon/evening, at least once a week, to facilitate accessibility for the patients | 73 | 7 | 1.9 | 7 | 27.1 |
| The rheumatology clinics should provide patients with specific information on the rheumatologist and nurse who are their attending professionals | 88 | 8.4 | 1.9 | 9 | 22.6 |
| The rheumatology clinics should establish specific hours for visits from representatives from the pharmaceutical industry | 87 | 8.6 | 1.7 | 9 | 19.8 |
| The rheumatologist, in the successive visits, should systematically review the medication with the patient in order to detect and solve any problems related to its efficacy and safety and patient adherence | 100 | 9.3 | 0.9 | 10 | 9.7 |
| In the case of patients with a lack of autonomy, the rheumatologist, together with the nurse, should identify the person who acts as caregiver and assess his or her capacity to assume that function | 80 | 7.8 | 2.3 | 8 | 29.5 |
| In the rheumatology clinics, the possibility of holding group consultations should be considered and the effort made to set up the necessary infrastructure to carry them out | 75 | 7.4 | 2.2 | 8 | 33.6 |
%≥7, percentage of participants who rated the item with a score of 7 or higher.
CV (%), coefficient of variation expressed as a percentage; SD, standard deviation.
Quality of Care Standards for Planning.
| %≥7 | Mean | SD | Median | CV (%) | |
|---|---|---|---|---|---|
| The rheumatology department is responsible for planning the agendas of the clinics | 100 | 9.5 | 0.7 | 10 | 7.4 |
| The rheumatology department must be notified 30 days in advance of any change in the agenda due to a scheduled activity (attendance at a meeting or teaching activities, among others) | 90 | 8.5 | 1.4 | 9 | 16.5 |
| The rheumatology department must be notified 60 days in advance of any change in the agenda due to vacations | 87 | 8.2 | 1.8 | 9 | 22 |
| If the changes in the schedule are made known before the established deadlines, the rheumatology department will take charge of canceling and rescheduling appointments | 96 | 9 | 1.4 | 10 | 15.6 |
| Changes in the schedule that are not made known before the established deadlines will be assumed by the rheumatology department | 84 | 8.4 | 1.9 | 9 | 22.6 |
| If a patient's appointment has been canceled for reasons for which he or she is not responsible, a new appointment must be scheduled within a maximum of 15 days | 97 | 8.8 | 1.5 | 9 | 17 |
| When patients come to the clinics without a previous appointment because their disease has worsened, due to an unexpected event or because they have been referred from the emergency department, the possibility of seeing them that same day should be taken into account. The idea of systematically leaving gaps in the agendas should be considered, so that the routine activity does not have to be interrupted to attend to them | 96 | 8.7 | 1.8 | 9 | 20.7 |
%≥7, percentage of participants who rated the item with a score of 7 or higher.
CV (%), coefficient of variation expressed as a percentage; SD, standard deviation.
In the following sections, we summarize the content of each subject area.
A. StructureRheumatology outpatient clinics should have natural lighting, be spacious and accessible, and be equipped with suitable and sufficient furnishings. The administrative area must be clearly differentiated from the clinical area. The infrastructure must be that necessary to ensure computerized management of the agenda, as well as a connection to the Internet and access to data in the computer network of the hospital and the health area. The structural requirements must be the same, regardless of whether the clinics are located in hospitals or in specialty centers.
B. Clinical Activity and Relationship With the PatientsThe medical record should be computerized and be included in an integrated system in which it is possible to access all the information on a patient's health (primary care, specialized care, hospital admission, emergency department). The clinical activity has to follow established protocols and there should be a system of diagnostic coding. Unless something unexpected arises, a patient should always be attended to by the same rheumatologist, who must make sure that the patient understands the relevant aspects of his or her disease and its treatment. It is essential to guarantee adequate communication between rheumatologists and patients and between the latter and the rheumatology department. Patient satisfaction with the care received should be evaluated periodically.
C. PlanningThe rheumatology department is responsible for planning the agendas of the outpatient clinics
D. Levels of PriorityThree levels of priority are considered in referrals to outpatient clinics: (1) urgent (maximum delay of 72h); (2) preferential (maximum delay of 15 days); and (3) ordinary (the appointment can be scheduled in accordance with the existing waiting period). In scheduling first visits, it is necessary to pre-establish a sufficient number of urgent and preferential visits to cover the needs of the health area.
E. Relationship With Primary Care, With the Emergency Department and With Other Departments of the HospitalThe rheumatology department should reach an agreement with primary care on patient care protocols that cover: (1) the disease processes included in the rheumatology service portfolio; (2) the criteria to be applied for patient referral in each disease process, as well as the level of priority; (3) the minimum data set that should be provided upon referral of a patient; and (4) the general guidelines for the follow-up of rheumatology patients in the primary care setting. Communication channels should be established between the rheumatology department and primary care in order to detect and correct, periodically, any diversions in the application of the patient care protocol. Likewise, agreements on patient care protocols should be reached with the emergency department and with other departments of the hospital.
F. ProcessThe rheumatology department should promote, provided that the necessary health care resources are available, dedicated clinics, multidisciplinary clinics and one-stop clinics. The rheumatology department is responsible for defining the agendas of the clinics and regulating the times necessary for each type of visit, which differ depending on the disease being treated. Outpatient clinics should be able to perform the diagnostic techniques used in the specialty. A rheumatologist should see patients a maximum of 4 days a week and a maximum of 5h a day.
G. Rheumatology NursingThe staff of the rheumatology department should include at least 1 specialized nurse. These nurses should have an office, an agenda of their own, in which to carry out their patient care activity. A nurse working in the rheumatology service should provide proof that he or she has sufficient knowledge of the specialty before undertaking the functions inherent in the rheumatology nurse's office.
H. Teaching and ResearchOutpatient clinics constitute a teaching space for students to practice their clinical learning and for the training of specialists. The patients should know that there is teaching activity taking place in the office in which they are being attended to. They should also know that they are being attended to by specialists in training. It is necessary to create specific agendas for patients included in clinical trials.
I. Calculation of the ActivityThe resolution ratio (ratio of first visits to successive visits) should be adjusted to the characteristics of the specialty of rheumatology. The following aspects should be differentiated in the calculation of the activity: (1) visits without a previous appointment; (2) writing reports; (3) consultations by telephone; (4) online consultations; (5) the techniques used routinely in the specialty; and (6) visits from patients in clinical trials.
DiscussionThe general guidelines for the clinical activity in outpatient clinics are described in the Guía de Gestión de Consultas Externas en Atención Especializada (Guidelines for the Management of Outpatient Clinics in Specialized Care) published by the Subdirectorate General of Specialized Care of the Spanish Ministry of Health.1 These guidelines are useful in terms of procedure, but make few references to quality of care.
With the present project, we have generated what, to our knowledge, is the first document of quality of care standards specifically designed to be applied in rheumatology outpatient clinics. Its major strengths lie in the utilization of a consensus methodology, in the large number of participants and in the inclusion of the perspective of the patient. Moreover, the document makes reference to all the activity carried out in the area of outpatient clinics, a circumstance that differentiates it from other previously published documents, which focus on quality of care standards for certain types of clinics, like those dealing with nursing in rheumatology11 and with early arthritis.12
The review of the literature carried out yielded no experience similar to that described here. In fact, the majority of the quality of care standards published focus on the management of specific diseases13–15 or on the regulation of the activity of specific functional units.16–18
The immediate reference of the EXTRELLA project is the document on quality of care standards drawn up by Alonso et al. and sponsored by the SER,7 in which the authors defined certain criteria for quality of care and for minimum time periods in rheumatology, both in patient and in training and research. The number of participants was very similar in both cases and consensus building was also achieved with 2 Delphi rounds. The differences between the 2 projects lie in that, in this one: (a) the participants who were not on the scientific committee were able to express, in the nominal groups, their opinion on the content of the questionnaire and propose changes; (b) the view of the patients was gathered through a discussion group; and (3) we listened to the opinions of nurses specialized in rheumatology (21% of all the participants).
Special care was taken to achieve a proportional territorial distribution of the participants, as well as stratification by hospital level, elements that are important since the aim was to obtain quality standards that would be valid regardless of the degree of complexity of the center and the health care model of the moment.
A considerable number of standards has been generated, classified according to 9 subject areas; the largest number correspond to areas with important content in terms of clinical care, such as “clinical activity and relationship with the patients” and “process”. Overall, the degree of agreement achieved can be considered very high. In fact, 90% of the participants gave scores of 7 or over in practically 3 fourths of the items. Nevertheless, there are differences by virtue of the different standards considered. The highest percentages were obtained for the standards for “calculation of the activity” and for “relationship with primary care, with the emergency department and with other departments of the hospital”, whereas the lowest percentages were obtained for the standards for “structure” and for “clinical activity and relationship with the patients”.
In the document, we advocate equipping the outpatient clinical with an adequate structure in terms of the physical dimension, as well as the clinical furnishings and electronic resources, we stress the need for easy and rapid communication between the patients and the department, and for patient care activities to be carried out in accordance with protocols. It is assumed that both the planning and management of the agendas correspond to the rheumatology department, that all the activity be computerized and that it is necessary to establish minimum times for patient care.
We also promote the creation of new modalities of care such as multidisciplinary clinics,19 one-stop clinics (rapid diagnosis units)2 and virtual consultation in which the patient and physician are not face-to-face,20–22 and we underscore the need to establish a functional connection with primary care, with the emergency department and with other departments of the hospital, in order to improve efficiency in the referral of those patients who, given their disease processes, will benefit the most from specialized care.12,23–25 Moreover, we reinforce the importance of the role of specialized nurses,26 who should have their own office and agenda, and we call attention to the fact that outpatient clinics are spaces in which teaching activity and clinical research are being carried out.
Finally, we maintain that the opinion of the patients should be gathered periodically so that we can measure the degree of satisfaction with the care received. This an important question, especially when increases in the overall perceived quality appear to depend more on improvements in aspects related to the structure and process than on the outcome.27
In conclusion, with the EXTRELLA project, consensus has been reached, with a high degree of agreement, on a set of quality of care standards that we consider may prove to be useful for the organization and management of the activity of the outpatient clinics of rheumatology departments.
Undoubtedly, at this moment in time, although it does not mean a decline in the care provided, in many centers in Spain, it is not possible to meet the standards presented here. In those cases, the document, far from being discouraging, can be considered a horizon to be reached, an objective to be attained, in short, as a reference framework when it comes to submitting proposals for improvements to the hospital management or to other levels of the administration.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis project was promoted by the Spanish Rheumatology Foundation with financial support from Roche. The company did not participate in the design of the project or intervene in the conclusions or writing of the final report or the present manuscript.
Conflicts of InterestThe authors declare they have no conflicts of interest involving the purpose of this study.
| Miguel Ángel Abad Hernández |
| Juan José Alegre Sancho |
| Raquel Almodóvar González |
| María Ángeles Álvarez Cidoncha |
| María Carmen Arias Juana |
| Francisco Javier Ballina García |
| Rocío Baturone Rey |
| Joaquín Belzunegui Otano |
| Pilar Bernabeu Gonzálvez |
| Juan José Bethencourt Baute |
| Laura Cano García |
| Amelia Carbonell Jordá |
| José Luis de la Iglesia Salgado |
| Carmen Domínguez Quesada |
| Silvia García Díaz |
| José Francisco García Llorente |
| Antonio García Sánchez |
| Susana Gómez Castro |
| Beatriz González Álvarez |
| Laura González Hombrado |
| María del Rocío González Molina |
| José Luis Guerra Vázquez |
| María del Carmen Herrero Manso |
| Silvia Iniesta Escolano |
| Antonio Juan Mas |
| Eduardo Kanterewicz Binstock |
| María José León Cabezas |
| José María Llobet Zubiaga |
| Francisco Javier López Longo |
| Eduardo Loza Cortina |
| Inmaculada Macías Fernández |
| José María Martín Martín |
| Olga Martínez González |
| María Cristina Mata Arnaiz |
| María Ángeles Matías de la Mano |
| Núria Montalà Palau |
| Rosa Morlà Novell |
| Ana Ortiz García |
| Ángela Pecondón Español |
| Eva Pérez Pampín |
| Valvanera Pinillos Aransay |
| Gema Poveda Marín |
| José Santos Rey Rey |
| Elena Riera Alonso |
| Basilio Rodríguez Diez |
| José Manuel Rodríguez Heredia |
| José Andrés Román Ivorra |
| Montserrat Romero Gómez |
| Antonio Romero Pérez |
| Susana Romero Yuste |
| Alejandro San Martín Álvarez |
| Ricardo Sánchez Parera |
| Xavier Surís Armangué |
| Rosa Varela Míguez |
| María del Carmen Vargas Lebrón |
| Paloma Vela Casasempere |
| Javier Vidal Fuentes |
The names of the Working Group of the EXTRELLA Project are listed in Annex 1.
Please cite this article as: Nolla JM, Martínez C, García-Vicuña R, Seoane-Mato D, Rosario Lozano MP, Alonso A, et al. Estándares de calidad asistencial para las consultas externas de reumatología. El proyecto EXTRELLA. Reumatol Clin. 2016;12:248–255.