Anterior uveitis is the most common type of intraocular inflammation. Those associated to HLA-B27 represent 18 to 32% of all anterior uveitis cases.
ObjectivesTo describe clinical characteristics, systemic treatment need, and frequency and type of ocular complications in a cohort of patients diagnosed with HLAB27-related anterior uveitis and in a cohort of patients diagnosed with HLA-B27 non-related anterior uveitis.
To establish if statistically significant differences between both cohorts exist.
Material and methodsWe performed a retrospective cohort study including patients with non infectious anterior uveitis related and not related to the antigen HLA-B27.
Results162 patients were included, 58 diagnosed with HLA-B27-related anterior uveitis (cohort HLA-B27+1) and 104 diagnosed with HLA-B27-non related anterior uveitis (cohort HLA-B27−).
No statistically significant differences were found regarding clinical characteristics between both cohorts with the exception of a higher frequency of recurrences in cohort HLA-B27+ and a higher frequency of chronic uveitis in cohort HLA-B27−. No differences were found regarding systemic treatment use nor development of ocular complications.
DiscussionIn contrast to previous studies, we neither found higher male gender predominance in the cohort of patients with HLA-B27-related anterior uveitis, nor did we find differences regarding average age, laterality, development of complications nor use of systemic corticosteroids.
La uveítis anterior es la forma más frecuente de inflamación intraocular. Las formas asociadas al antígeno HLA-B27 suponen entre un 18 y un 32% de los casos de uveítis anterior.
ObjetivosDescribir las características clínicas, la necesidad de tratamiento sistémico y la frecuencia y el tipo de complicaciones oculares de una cohorte de pacientes con uveítis anterior asociada a HLA-B27 y de una cohorte de pacientes con uveítis anterior no asociada a HLA-B27.
Establecer si existen diferencias entre ambas cohortes.
Material y métodosSe realiza un estudio de cohortes retrospectivo descriptivo con componentes analíticos incluyendo a pacientes con uveítis anterior endógena no infecciosa asociada y no asociada a HLA-B27.
ResultadosSe incluye un total de 162 pacientes, 58 con uveítis anterior asociada a HLAB27 (cohorte HLA-B27+) y 104 con uveítis anterior no asociada a HLA-B27 (cohorte HLA-B27–).
No se aprecian diferencias estadísticamente significativas en las características clínicas de ambas cohortes a excepción de una mayor tendencia a la recurrencia en la cohorte HLA-B27+ y una mayor tendencia a la cronicidad en la cohorte HLA-B27–. Tampoco se aprecian diferencias en cuanto al uso de tratamiento sistémico ni al desarrollo de complicaciones oculares de forma global.
ConclusionesA diferencia de lo descrito con anterioridad, en este trabajo no encontramos un mayor predominio masculino en la cohorte de uveítis asociada a HLA-B27. Tampoco se aprecian diferencias en edad media, lateralidad, presencia de complicaciones ni frecuencia de uso de corticoides sistémicos.
Uveitis is inflammation of the middle layer of the eye (uvea), located between the sclera and the retina, which is comprised of the iris, ciliary body, pars plana and/or choroid. In some cases, by extension, it can also affect the retina.
The incidence of uveitis is 45–52 cases per 100,000population/year, it peaks between the ages of 20 and 44 years, and the prevalence of the disease is 70 cases per 100000 population.1,2 It is the third leading cause of blindness in the working age population in developed countries, and 10% of the cases of total loss of vision are due to uveitis.
Anterior uveitis is the most common form of intraocular inflammation, representing between 50% and 92% of all cases of uveitis reported in a Western population.3 Anterior uveitis associated with HLA-B27 accounts for between 18% and 32% of the cases of anterior uveitis found in that population.4
It has been reported more frequently in men, in whom onset is earlier (20–40 years), it tends to be unilateral and there are higher rates of recurrences and complications. Anterior uveitis is more severe when associated with the HLA-B27 antigen, with a higher degree of inflammation and a more frequent use of systemic corticosteroids.5
ObjectivesThe purpose of this article is to describe the clinical features, the need for systemic therapy and the frequency and types of ocular complications in a cohort of patients with anterior uveitis associated with HLA-B27 and in a cohort of patients with endogenous noninfectious anterior uveitis not associated with HLA-B27.
We also proposed to establish whether there were differences between the 2 cohorts in terms of clinical features, frequency and types of ocular complications, and the frequency of the use of systemic corticosteroids and other systemic immunosuppressive agents.
Material and MethodsStudy Design and PatientsWe conducted a retrospective descriptive cohort study with analytical components, including patients diagnosed with anterior uveitis associated with HLA-B27 with follow-up in a multidisciplinary uveitis clinic at Hospital Universitari Doctor Peset in Valencia, Spain (HLA-B27+) and patients diagnosed with endogenous noninfectious anterior uveitis not associated with HLA-B27 with follow-up in the same multidisciplinary uveitis clinic at Hospital Universitari Doctor Peset (HLA-B27−).
Inclusion Criteria- –
HLA B27+ cohort: patients diagnosed with anterior uveitis (acute, recurrent or chronic) associated with HLA-B27, with a follow-up of at least 1 month in the multidisciplinary uveitis clinic at Hospital Universitari Doctor Peset.
- –
HLA B27− cohort: patients diagnosed with endogenous noninfectious anterior uveitis (acute, recurrent or chronic) not associated with HLA-B27, with a follow-up of at least 1 month in the multidisciplinary uveitis clinic at Hospital Universitari Doctor Peset.
- –
Anterior uveitis associated with other locations (intermediate, posterior, panuveitis).
- –
Traumatic uveitis.
- –
Infectious uveitis.
The data were obtained from an electronic registry (.sav format) that includes patients who underwent follow-up between 1 January 2008 and 17 March 2015.
The variables considered in the study were: length of follow-up, age, sex, diagnosis, clinical course according to the criteria of the Standardization of Uveitis Nomenclature (SUN) Working Group,6 laterality, use of systemic immunosuppression, use of systemic corticosteroids, and presence and type of complications.
Data ManagementDescriptive StatisticsWe calculated proportions for the categorical variables and mean±standard deviation (or median and interquartile range if the data for the sample did not follow a normal distribution) for continuous variables.
Inferential StatisticsThe chi-square statistic was used to compare proportions, applying the continuity correction if necessary.
Student's t statistic was utilized to compare means. If the data of the sample did not follow a normal distribution, the Kruskal–Wallis statistic was utilized.
A P value <.05 was considered to indicate statistical significance.
The statistical analysis was performed using the SPSS software package (version 13).
ResultsWe included a total of 162 patients, 58 with anterior uveitis associated with HLA-B27 (HLA-B27+) and 104 with endogenous noninfectious anterior uveitis not associated with HLA-B27 (HLA-B27−).
Of the HLA-B27+ patients, 30 had a diagnosis of spondyloarthritis and 1 had a diagnosis of juvenile idiopathic arthritis (JIA). The different types of spondyloarthritis are shown in Table 1. We wish to point out the fact that 64.5% of these patients were diagnosed with spondyloarthritis after having been referred from the ophthalmology department to the rheumatology department after a first episode of uveitis. Most of these patients described symptoms characteristic of long-standing spondyloarthritis.
Association With Spondyloarthritis in the HLA-B27+ Cohort.
| Type of spondyloarthritis | n (%) |
|---|---|
| Ankylosing spondylitis | 19 (63.3) |
| Nonradiographic axial spondyloarthritis | 6 (20) |
| Peripheral spondyloarthritis | 1 (3.3) |
| Psoriatic spondyloarthritis | 1 (3.3) |
| Spondyloarthritis associated with inflammatory bowel disease | 1 (3.3) |
| Undifferentiated spondyloarthritis | 2 (6.6) |
| Total | 30 (100) |
Most of the HLA-B27− patients had been diagnosed with idiopathic uveitis. The various diagnoses included and their frequency in this cohort can be seen in Table 2.
Diagnoses in the HLA-B27− Cohort.
| Diagnosis | n (%) |
|---|---|
| Idiopathic uveitis | 81 (77.9) |
| Uveitis associated with juvenile idiopathic arthritis | 7 (6.7) |
| Uveitis associated with spondyloarthritis | 6 (5.8) |
| TINU syndrome | 3 (2.9) |
| Sjögren's syndrome | 2 (1.9) |
| Behçet's disease | 2 (1.9) |
| Fuchs’ heterochromic iridocyclitis | 2 (1.9) |
| Relapsing polychondritis | 1 (1) |
| Total | 104 (100) |
TINU, tubulointerstitial nephritis and uveitis.
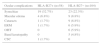
The demographic and clinical characteristics of both cohorts are shown in Table 3.
Patient Characteristics and Clinical Features.
| Characteristics and features | HLA-B27+ (n=58) | HLA-B27− (n=104) | P value |
|---|---|---|---|
| Age (years), mean±SD | 41±13.03 | 47.24±20.24 | .071 |
| Sex, n (%) | M 31 (53.4) | M 42 (40.4) | .109 |
| W 27 (46.6) | W 62 (59.6) | ||
| Length of follow-up in months, median (interquartile range) | 34.5 (4.75–54) | 13.5 (3–47) | .074 |
| Laterality, n (%) | U 36 (62.1) | U 55 (52.9) | .259 |
| B 22 (37.9) | B 49 (47.1) | ||
| Clinical course, n (%) | A 19 (32.8) | A 53 (51) | <.001 |
| R 39 (67.2) | R 29 (27.9) | ||
| C 0 | C 22 (21.2) |
A, acute; B, bilateral (simultaneous or alternating); C, chronic; M, men; M: women; R, recurrent; SD, standard deviation; U, unilateral.
The mean age of the patients in the two cohorts was between 40 and 50 years, and there were no statistically significant differences between them.
We did not observe a significant predominance of one sex over the other in either of the 2 cohorts, although there was a somewhat higher number of men in the HLA-B27+ cohort and of women in the HLA-B27− cohort.
The median length of follow-up was greater in the HLA-B27+ cohort, but the difference did not reach statistical significance when compared with the HLA-B27− cohort.
Likewise, no significant differences were found with regard to laterality; unilateral involvement was more frequent in both cohorts.
However, differences were observed in terms of the clinical course. In the HLA-B27+ cohort, somewhat more than 2 thirds of the patients experienced recurrences and there were no cases of chronic uveitis. In the HLA-B27− cohort, half of the patients had had only 1 episode of uveitis, somewhat more than a fourth of the patients had a recurrent course, and the remainder, chronic.
The proportion of patients who developed some type of complication was similar in both cohorts, there being no statistically significant differences (P=.686). However, when the types of complications that were documented for the patients in the 2 cohorts were analyzed, we observed differences, but the statistical significance could not be determined because the sample size was not large enough (Table 4), except in the case of synechiae, which were more common in the HLA-B27+ cohort, although the difference was not statistically significant (P=.07). One patient in this cohort developed central serous choroiditis related to the use of systemic corticosteroids. In the HLA-B27− cohort, band keratopathy was observed in 6 patients, all of whom had been diagnosed with JIA. We also found a higher frequency of cataracts and ocular hypertension (OHT) in the HLA-B27− cohort. This fact was not associated with a more widespread use of systemic corticosteroids given that, as was seen in the case of cataracts, the higher frequency in the HLA-B27− cohort can be explained by a greater trend toward chronicity. In the case of OHT, the differences can be explained by the greater trend toward hypertension in some of the types of uveitis, such as Fuchs’ heterochromic iridocyclitis, included in the HLA-B27− cohort. The presence of OHT coincided with ocular inflammatory activity in all the patients.
Ocular Complications.
| Ocular complications | HLA-B27+ (n=58) | HLA-B27− (n=104) |
|---|---|---|
| Synechiae | 19 (32.7%) | 23 (22.3%) |
| Macular edema | 4 (6.8%) | 9 (8.8%) |
| Cataracts | 1 (1.7%) | 9 (8.8%) |
| ERM | 1 (1.7%) | 6 (5.9%) |
| OHT | 0 | 6 (5.9%) |
| Band keratopathy | 0 | 5 (4.8%) |
| CSC | 1 (1.7%) | 0 |
CSC, central serous choroiditis; ERM: epiretinal membrane; OHT, ocular hypertension.
Regarding the use of corticosteroids or other systemic immunosuppressive agents, again, there were no statistically significant differences, as these treatments were seldom required in either cohort (Table 5).
Most of the patients treated with systemic corticosteroids began the therapy with a dose of 30mg a day of prednisone or the equivalent. In every case, immunosuppressive therapy was introduced due to ocular inflammatory activity that could not be controlled with other treatments, in general, to prevent recurrences or chronicity.
The immunosuppressive agents utilized were sulfasalazine, methotrexate, adalimumab and tocilizumab (Table 6).
DiscussionThere are a considerable number of publications dealing with the clinical features and prognosis of HLA-B27-associated anterior uveitis.7–16
The description of the clinical features coincides in the majority of the publications, but the prognosis does not. We found articles in which the authors reported a better prognosis for uveitis associated with HLA-B27,7 whereas others affirmed the opposite,8 and still others who observed a prognosis similar to that of anterior uveitis not associated with HLA-B27.9–13
In contrast to earlier publications,4,5 in the present study, we did not observe male predominance in the cohort of patients with anterior uveitis associated with HLA-B27, an earlier onset or a greater trend toward unilaterality in that cohort. However, we did find a greater trend toward recurrence in the patients with anterior uveitis associated with HLA-B27, similar to that reported in previous publications.4,12 The rest of the clinical features were similar in both cohorts.
One noteworthy finding is the high percentage of patients who were diagnosed with spondyloarthritis after being referred from the ophthalmology department to the rheumatology department due to an episode of uveitis. This circumstance demonstrates the importance of the collaboration between the two specialties.
In this study, we did not take into account the degree of inflammatory activity at the time of the onset of the episode of uveitis because of the difficulty in standardizing the information, since the episodes were evaluated by different ophthalmologists and there was wide variability in terms of the establishment of the degree of inflammation.
Likewise, we did not take into account the visual prognosis of the patients, as we considered that the study design was not the most appropriate for that assessment or for establishing prognostic factors. We would like to continue the study, carrying out a prospective evaluation of the patients for the purpose of clarifying this point.
The fact that we found no statistically significant differences between the two cohorts in terms of the use of corticosteroids—in contrast to results published elsewhere5—and other systemic immunosuppressive agents, and the presence or absence of complications could indicate that the severity and the visual prognosis is comparable in the two groups, but we cannot reach any further conclusions because of the limitations of the study, which include the unavailability of data on the changes in the visual acuity of the patients. Moreover, in the HLA-B27− cohort, we observed an incidence of chronic uveitis of 21% and not a single case in the HLA-B27+ cohort. This difference would mean that, although the uveitides in the HLA-B27+ cohort were more severe, no significant differences were observed in terms of the use of systemic therapy on comparing the two cohorts, because in the patients with chronic uveitis, even if the activity was lower, systemic therapy would be initiated more often.
With respect to the differences observed in the various types of ocular complications, which, as we mentioned above, cannot be measured accurately because of the small sample size, we should consider the influence of the heterogeneity in the HLA-B27− cohort, which includes 8 different diagnoses. This would explain, for example, the elevated presence of band keratopathy, observed only in those patients of the sample with a diagnosis of JIA.
If we exclude synechiae, whose influence on the visual prognosis of the patient is low, the rate of complications is low in both cohorts.
In conclusion, in the present article, there are no significant differences between the clinical features of uveitides associated with HLA-B27 and those of uveitides not associated with HLA-B27, with the exception of a greater trend toward recurrence.
The study design does not enable us to establish differences with respect to the visual prognosis.
We would like to increase the sample size of the study and carry out a prospective follow-up to obtain information on the differences in the development of different types of ocular complications, and on differences and possible factors that intervene in the prognosis.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Valls Pascual E, Fontanilla Ortega P, Vicens Bernabeu E, Martínez-Costa L, Blanco Alonso R. Características clínicas, tratamiento y complicaciones oculares de uveítis anterior asociada y no asociada a HLA-B27. Reumatol Clin. 2016;12:244–247.