To develop expert-based recommendations on physical activity and exercise for patients with spondyloarthritis (SpA).
MethodsTwo discussion groups, one of physical therapists, rehabilitation physicians, and professionals of physical activity and sports, and another of rheumatologists interested in SpA, were held to discuss the results of a survey of rheumatologists on exercise and two focus groups with patients on barriers to exercise. Preliminary recommendations were drafted. These were submitted to the opinion of the experts in both groups according to a two round Delphi methodology.
ResultsTwenty-one recommendations covering general aspects of exercise, adaptation to patient, how to deliver messages, pain management, and type of exercise and monitoring were issued. The level of agreement varied slightly between expert groups but it was high overall. Items with poor agreement were removed from the consensus.
ConclusionsWe present recommendations on when and how to prescribe and monitor exercise in patients with SpA based on the opinion of experts in exercise and in SpA. We must now test whether these recommendations are useful for clinical practice and have an effect on patients with SpA seen by rheumatologists.
Desarrollar recomendaciones sobre la actividad física y el ejercicio para pacientes con espondiloartritis (EspA) basadas en la opinión de expertos.
MétodosDos grupos de expertos, uno de fisioterapeutas, rehabilitadores y profesionales de la actividad física y deporte y otro de reumatólogos con interés en EspA, se reunieron para discutir los resultados de grupos focales con pacientes sobre barreras al ejercicio y de una encuesta a reumatólogos sobre ejercicio en EspA. A continuación se redactaron unas recomendaciones preliminares que fueron sometidas a la opinión de los expertos de ambos grupos mediante metodología Delphi a dos rondas.
ResultadosSe emitieron 21 recomendaciones que cubren el ejercicio físico, la adaptación al paciente, el modo de dar los mensajes, el manejo del dolor, el tipo de ejercicios indicado y el seguimiento. El grado de acuerdo varía ligeramente entre los grupos de expertos pero en general fue alto. Los ítems discordantes o con poco acuerdo fueron eliminados del consenso.
ConclusionesSe han emitido recomendaciones sobre cuándo y cómo prescribir ejercicio físico y monitorizarlo en pacientes con EspA basadas en la opinión de expertos en espondilitis y en la prescripción de ejercicio. Deberemos confirmar si estas recomendaciones son útiles para la práctica clínica y tienen efecto en los pacientes con EspA atendidos por reumatólogos.
Spondyloarthritis (SpA) produces a clear limitation of mobility and functional capacity in the patients who develop this disease.1 Although drug treatment is the basis of the therapeutic management of SpA, non-drug treatment is a fundamental complement. Among these treatments, physical exercise has been shown to improve activity, symptoms, functional capacity, cardiorespiratory function and quality of life, and it has been suggested that it could prevent the development of deformities, with a synergistic effect with drug therapy.1,2 In fact, the importance of exercise in SpA is such that is has led to the inclusion of recommendations concerning physical activity in the consensus for the management of SpA and even in specific consensuses involving physical activity in SpA reached by diverse international oganisms.3–7
A Cochrane review on the efficacy of physical therapy in SpA patients, which included 11 clinical trials performed up to January 2007 and involved a total of 763 patients, found beneficial effects of exercise on mobility, functional capacity and overall patient well-being.8 The efficacy proved to be greater with supervision, the utilization of specific programs and global postural re-education, among other findings.8 The results of an update of this systematic review demonstrate that, in general, exercise programs in SpA do not meet the most recent recommendations for exercise suggested by the international organisms, the measuring of the physiological response for evaluating their efficacy is not adequate and, moreover, few of the reports evaluated adherence to the exercise program.9
An important part of the efficacy of exercise programs in SpA is due to the degree to which correct adherence is assured. This largely depends on the facility and accessibility of the program that has been designed and its adaptation to the individual. Distributing brochures without any explanation, for example, as an educational program on home exercise, improves knowledge of the disease and promotes exercise, but adds only marginal benefits to drug therapy in terms of activity, functional capacity and quality of life.1,10 On the other hand, the barriers to exercise perceived by SpA patients should be considered when it comes to designing exercise programs, and include, among others, the inconsistency among the messages of the different professionals and the lack of adaptation of the exercises to the phases of the disease and their preferences.11
A previous study by our group demonstrated that rheumatologists consider exercise to be a fundamental part of the treatment of rheumatic patients; however, they require greater knowledge and the development of specific prescription strategies for exercise in rheumatology.12 More than occasionally, there are difficulties for the prescription and implementation of exercise interventions or programs in routine clinical practice, since rheumatologists do not see themselves as qualified to provide guidelines for and perform the follow-up of an exercise program. Moreover, it is perceived that there continue to be negative messages about the risks of exercise in SpA patients.
The objective of this study is to develop a series of recommendations based on expert opinion and the available scientific evidence, which would be utilized as indications for the performance of physical activity and exercise in patients with SpA and their management in the different phases of the disease.
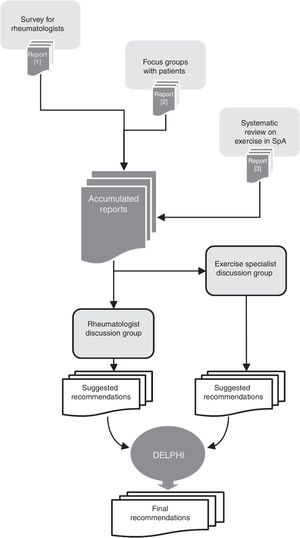
MethodsThese recommendations are based on previous research carried out sequentially, and the objective was to achieve an in-depth knowledge of the problematic, as well as to know the opinion of different professionals and the patients implicated, to subsequently carry out the discussion of the results and issue recommendations. Fig. 1 shows a general vision of the EJES-3D project and the procedures followed to reach these recommendations.
In a first phase, we distributed a survey sent by e-mail utilizing an online platform of the 106 professionals who are members of the SpA working group of the Spanish Society of Rheumatology (GRESSER), the results of which have been published.12
To learn the opinion and evaluation of the patients, we considered that the most adequate technique was to form focus groups. For the recruitment of the participants we contacted with the Spanish Coordinator of Spondylitis and the Spanish League of Rheumatology. The results of these groups have also been published.11
Discussion of the Results and the Basis of the RecommendationsThe results of the survey and of the focus groups were presented in 2 discussion groups. To the first group, we invited specialists in exercise, physical activity and sports and physiotherapists, who were familiar to the scientific committee, who, in turn, invited others (snowball sampling). In all, 9 individuals were invited (see the description in Table 1). In the meeting, we established the discussion forum and the bases for the most technical recommendations were determined (report of the meeting is available upon request). The second group was attended by rheumatologists selected from the participants of the GRESSER group due to their interest in the subject, and they were explained the preceding material. In this second group, we discussed the recommendations provided by the first group and determined the bases for the overall recommendations for indication, follow-up and their adaptation to the rheumatology services.
Description of the Participants in the Panels.
| Descriptors | Panel of exercise specialistsa | Panel of rheumatologists |
|---|---|---|
| Guests | 10 | 12 |
| Participants | 8 (80%) | 7 (58%) |
| Age (range) | 37–57 | 37–64 |
| Gender (% women) | 10% | 10% |
| Years of experience (range) | 9–32 | 9–40 |
| No. of SpA patients attended to each month (mean) | 3 | 30 |
| Percentage of patients treated in public health care centers | 50% | 100% |
| Geographic region | Community of Madrid, Castile-La Mancha | Andalusia, Principality of Asturias, Canary Islands, Catalonia, Community of Madrid, Region of Murcia |
The group was composed of 2 physiotherapists, 3 doctors in Sciences of Physical Education and Sports, one with two other degrees (apart from nursing and teaching) and 2 rehabilitators (one of the coordinators, MF, is also a rehabilitator). Those who failed were a rehabilitator and a physiotherapist.
The preliminary recommendations were voted in a first Delphi round to establish the level of agreement with the proposals. The level of agreement was expressed by voting according to a Likert scale from 1 (totally in disagreement) to 5 (totally in agreement). This was defined if the mean in the two groups and overall mean was over 4 and the standard deviation did not exceed 1. The recommendations with a level of agreement of less than 4 were rewritten, taking into account any comments received, and were voted on in a second Delphi round. It was possible to include new recommendation between the two Delphi rounds, which were voted on in the second round.
ResultsTaking all the recommendations into consideration, both panels coincided in a series of general principles: (1) a consensus should be reached in terms of the content of messages on exercise and the arguments among all of the professionals who treated each patient, either at the hospital level or in the associations; (2) the attempt should be made not to give negative messages on engaging in exercise; (3) the continued practice of supervised exercise improves the patient's general health and physical capacity, and reduces cardiovascular risk; (4) it is important that patients feel safe when engaging in physical exercise, explaining that there is a great deal of evidence about the benefits in patients with SpA; and (5) to achieve that the patient feels motivated to exercise, it is indispensable that the professionals (rheumatologists) be convinced of its efficacy and advisability and be motivated to provide guidance for it.
Advice on exercise was divided into several sections, from general messages to suggestions for the follow-up of the exercise performed by the patient. The recommendations are based on general evidence concerning exercise.13–15 Special interest was placed on not contradicting the existing international guidelines and expert panels.5,10,13,14Table 1 demonstrates the final recommendations with their level of agreement. We then show the studies and information that support each of the sections.
Messages During Visits to the PhysicianBefore they know all of the complications of the disease, the patients want information on what they can do to improve.11 It must be stressed that exercise is a fundamental pillar of the treatment and these individuals should be informed of the benefits it produces.
Attitude and the level of knowledge of the rheumatologist are essential for the prescription of exercise. If rheumatologists feel that what they prescribe is convenient, because they are familiar with it, it is probable that they devote more time to the office and perform an adequate follow-up.15 Patients confide in verbal and written information provided by their specialists. Thus, it is necessary to design strategies to be employed in the office to provide positive information.16 For example, we allude to a number of studies that have demonstrated the benefit of the combined effect of drug therapy plus exercises devised specifically for SpA versus drug therapy or exercise alone.10,17–20
On the other hand, the patient must be given realistic information, with the specification that, like certain drugs, exercise requires perseverance and time in order to begin to have an effect. This message is important to prevent dropouts for not complying for this reason. In initial phases, it is preferable to give only positive messages to incite the patients to exercise, for the purpose of converting it into a routine.
Exercise and Activity Depending on the Phase of SpondyloarthritisIt is essential to make the message clear that exercise is necessary in all the phases of SpA, given that the general advantages are maintained throughout the disease. However, for an optimal efficacy of the exercise program, it is indispensable to consider the phase of the disease, its activity and progression.10 In the opinion of the experts, an early introduction of the indications following the diagnosis might favor a greater implication and adherence to exercise.
In the initial stages—patients with less severe mobility limitation and functional impact—the recommendation for physical activity is that advised by the American College of Sports Medicine for healthy adults (Tables 2 and 3).13 According to this recommendation, an adult between 18 and 64 years of age should spend a minimum of 150min a week in moderate aerobic physical activity, or a minimum of 75min a week in vigorous aerobic activity or, again, an equivalent combination of moderate and vigorous activity; all this should be distributed over a period of 3–5 days.
Recommendations for the Indication and Follow-up of Exercise in Spondyloarthritis With Level of Agreement.
| Recommendation | Exercise specialists | Rheumatologists | Total | ||
|---|---|---|---|---|---|
| m (SD) | r | m (SD) | r | m (SD) | |
| Messages in the physician's office | |||||
| It is advisable to give advice on engaging in physical activity, regardless of whether or not it is added to a specific exercise program | 5.0 (0.0) | (5–5) | 4.4 (0.5) | (4–5) | 4.7 (0.5) |
| There should be a specific time devoted to consultations on aspects related to exercise | 4.6 (0.5) | (4–5) | 4.6 (0.5) | (4–5) | 4.6 (0.5) |
| It must be stressed that exercise is a fundamental pillar of treatment | 5.0 (0.0) | (5–5) | 4.7 (0.5) | (4–5) | 4.9 (0.4) |
| Exercise according to the stage of SpA | |||||
| The patient must receive messages that exercise is necessary in all the phases of SpA, given that the general advantages are maintained throughout all the stages | 5.0 (0.0) | (5–5) | 4.6 (0.5) | (4–5) | 4.8 (0.4) |
| It is recommended that SpA patients in any stage engage in moderately intense aerobic exercise, at least 30min 5 days a week | 4.4 (0.8) | (3–5) | 4.2 (0.4) | (4–5) | 4.3 (0.6) |
| In the initial phases, the recommendation is to prescribe fewer and simpler exercises | 4.0 (1.5) | (1–5) | 4.2 (0.7) | (3–5) | 4.1 (1.2) |
| In the intermediate phases, it is necessary to stress the progression of exercise, being careful not to exceed the limit in which it would not be beneficial; in this respect, it may be recommended to seek professional help from an exercise specialist | 5.0 (0.0) | (5–5) | 4.4 (0.5) | (4–5) | 4.7 (0.5) |
| In advanced phases, it is necessary to maintain the level of physical activity and exercise, avoiding overexertion and working on flexibility | 4.0 (1.1) | (2–5) | 4.4 (0.5) | (4–5) | 4.2 (0.9) |
| If the patient already has ankylosis, aerobic exercises and those designed for strengthening should be recommended, avoiding forced stretching and high-impact exercises as they can be hazardous | 4.8 (0.4) | (4–5) | 4.8 (0.4) | (4–5) | 4.8 (0.4) |
| Exercise type and format | |||||
| Exercises must take into account the patient's preferences and be suitable for his or her age, pain status, fatigue and physical form | 5.0 (0.0) | (5–5) | 5.0 (0.0) | (5–5) | 5.0 (0.0) |
| Before recommending any type of physical activity or exercises, it is necessary to investigate the patient's basal level | 5.0 (0.0) | (5–5) | 5.0 (0.0) | (5–5) | 5.0 (0.0) |
| The selection of the exercise must take into account the current level of the patient; if it is too demanding or the progress is not sufficient, it will be more difficult for the patient to perform it | 5.0 (0.0) | (5–5) | 4.8 (0.4) | (4–5) | 4.9 (0.3) |
| It is recommendable to include a component of postural education in the exercise program | 5.0 (0.0) | (5–5) | 4.6 (0.8) | (3–5) | 4.8 (0.6) |
| Working in groups is recommended as a good option to facilitate adherence and lower costs, although it decreases the personalization of the exercise | 4.8 (0.4) | (4–5) | 4.6 (0.5) | (4–5) | 4.7 (0.5) |
| Exercise in a painful situation | |||||
| Immobilization should be avoided, even in periods of pain | 4.8 (0.4) | (4–5) | 4.4 (0.5) | (4–5) | 4.6 (0.5) |
| Follow-up | |||||
| In follow-up visits, the patient must be asked about the type and dose of exercise, which should be included in the history, and he or she should be urged to maintain it or even increase it | 4.6 (0.5) | (4–5) | 4.6 (0.5) | (4–5) | 4.6 (0.5) |
| Some type of supervision is advisable, for example, sending the patient e-mails and carrying out follow-up, especially in the initial phases of the program | 4.8 (0.4) | (4–5) | 4.2 (0.4) | (4–5) | 4.5 (0.5) |
m, mean; r, range; SD, standard deviation; SpA, spondyloarthritis.
Basic Exercise Principles of the American College of Sports Medicine and Physical Activity.
| 1. Overload and adaptation | If an exercise is performed with overload (greater than normal effort) there is a temporal decrease in capacity, but the system recovers by increasing it to a level that is greater than the original value. This cumulative effect is what we refer to as training |
| 2. Progression | The stimulus of exercise should progress over time (intensity or duration) to continue to improve |
| 3. Specificity | Adaptations induced by exercise are specific for the muscles and for the capacities that become overloaded |
| 4. Recovery | The organism needs time to replace the reserves and to perform adaptive processes |
| 5. Reversibility | The effects disappear gradually if the exercise program is interrupted. The effects can be maintained with a reduction of the frequency |
| 6. Individuality | Individual responses to exercise vary Each person has a different capacity for recovery |
Taken from Garber et al.13
In intermediate phases (patients with limited mobility and functional impact), the progression of exercise should be stressed from the start, with the prevention of exceeding the limit in which it will no longer be beneficial; in this respect, professional help from a specialist in physical exercise can be suggested. In this phase, a combination of adapted aerobic exercise and one of the programs for stretching-strengthening that have shown to be effective in clinical trials should be recommended.21-23
In advanced phases (in patients who are found to have ankylosis), aerobic exercise should continue, avoiding overexertion and working on flexibility. Simple exercises can be added that make it possible to strengthen the major muscle groups (vertebral, diaphragm, abdominal, etc.23,24). Forced stretching and maintained postures do not appear to be effective and rheumatologists should advise against them.
It is recommended that the prescription initially include few and simple exercises in all the phases. This will favor adherence of patients who exercise very little, given that the complexity of a therapeutic intervention reduces adherence and programs with a limited number of simple exercises will have greater probabilities of being maintained over time.25
Exercise Type and FormatRegarding the type of physical activity, the experts recommend adapting the frequency, intensity, duration and type of exercise to the preferences of the patient, as well as the results of the physical examination, the aims and lifestyle of each. The international guidelines on physical activity can be utilized, although they will require adaptation. Traditionally, exercises indicated in patients with SpA were for the maintenance of spinal and thoracic mobility, but it has been seen that aerobic exercise should be included in the prescription for these individuals. The performance of cardiorespiratory exercises and those involving muscle strength have demonstrated their efficacy in the prevention of cardiovascular diseases in SpA because of the reduction of classical risk factors and improvement in aortic elasticity,25–27 in addition to increasing the flexibility of these patients.8,9,28
The exercises should be adjusted to the severity of the disease, the short- and long-term objectives, the needs and expectations of the patient and even his or her resources.18 The inadequacy of exercise, either due to its elevated intensity or because its progressivity is limited, is a barrier for the patients who exercise. Thus, it is necessary to adapt physical exercise to the patient who has seen improvement with adherence, which facilitates training.10,22
The exercise programs most widely utilized focus on the improvement of flexibility, thoracic expansion and strengthening of the extensor musculature. They include exercises of the major muscle groups, especially the vertebral and pelvic muscles of the posterior plane.29 There are certain cases in which the recommendations include overall exercises that can also be functional, such as squatting, getting up from a chair, etc. Another alternative involves overall flexibility that consists of stretching at the level of the back and of the lower and upper extremities.30
In initial phases, exercises involving the spine do not provide a significant improvement; whereas aerobic exercise leads to less pain and stiffness. Sveaas et al.26 found that engaging in high-intensity exercise improved the Bath Ankylosing Spondylitis Disease Activity Index score, acting as a complement to drug intervention. If the patient already has ankylosis, aerobic exercises and those designed for strengthening should be recommended, avoiding forced stretching and high-impact exercises as they can be hazardous.21,31
The exercise guidelines can include a component of postural education. Patients in whom postural education is indicated improve in terms of morning stiffness, spinal mobility, thoracic expansion and quality of life.22,23 Sports that promote a good posture and stretching of the torso, such as hiking, swimming, cross-country skiing, tennis, badminton, archery, Nordic walking and volleyball, are especially recommendable.4
With respect to the format, supervised exercise programs seem to be more effective than unsupervised models. This may be the result of an increased adherence or because these exercises have a greater control in terms of intensity and duration.1,8,24,28,32,33 Working in groups is recommended as a good option to facilitate adherence and lower the costs, although it reduces the individuality of the exercise1,2,34 and, as the patients point out, the individual barriers to a given activity must be taken into account.11
Exercise in a Painful SituationWhen there is pain, it cannot be ignored, and it is necessary to avoid any exercise that significantly increases it. During a flare, or when there is pain or inflammation, the range of mobility should be restricted to “unpainful” limits, and there should be a close supervision of exercise to avoid complications.29 Nevertheless, immobilization should be avoided, even in periods of pain, since physical activity helps to relieve the pain, improves spinal mobility and the overall assessment of the patient.9,35 It is necessary to avoid exercise focused on a painful region unless there is a clear objective. For example, exercise involving cervical flexibility would not be indicated in a patient with pain in that region, but with no limitation affecting mobility. It is useful to have variants of certain types of exercise for patients with given characteristics (advanced age, an evident limitation of mobility).36
Follow-upIt is advisable to have some type of supervision, for example, sending e-mails to the patient and carrying out follow-up especially in the initial phases of the process. An adequate way to make patients engage in exercise programs as part of their custom could be the use of motivating messages, or the routine introduction of phrases promoting physical activity. There must be sufficient follow-up and feedback, in an individual manner, to achieve the confidence and proficiency with the performance of physical exercise and to be informed of the necessities of changing the prescription. All of the patient's follow-up visits must include questions on the type and dose of exercise, and the patient should be asked to maintain it or even increase it. Although it would be unusual, the patient may be engaging in more exercise than would be reasonable. In these cases, it is important to detect this fact and modulate it.
DiscussionBased on the experience of the experts in the management and treatment of SpA, in the light of data concerning exercise in patients with SpA, it is necessary to stress the idea of the need to implant programs designed to provide physical exercise in SpA patients as soon as possible to achieve good adherence to these plans. For this document, we did not search for existing primary evidence; rather, the experts on exercise based their comments on existing general recommendations on exercise—which were based on evidence—and on our own data, with a qualitative perspective, or on studies in SpA. With this information, we issued recommendations specific for SpA adapted to the expressions and the competencies of rheumatologists.
These recommendations are not, by any means, the first to be issued for SpA patients. There are guidelines in which exercise has been added as another aspect of the treatment, as for example, in ESPOGUÍA,36 which includes a section on physical therapy and rehabilitation which emphasizes the importance of exercise, or the guidelines of the European League Against Rheumatism (EULAR).3,7 There are also specific guidelines on exercise, like those of the Turkish Society for Rheumatology5—which lead us to understand that the composition of this scientific society includes a large number of physiotherapists—but whose recommendations appear to concern specific exercises. Perhaps the most noteworthy recommendations are those of a spondylitis special interest group of physiotherapists an Australian.10 They are different from those presented above in that they put special emphasis on evaluation and monitoring using measures of mobility and exercise dosage. Although we agree with the proposals of this group, they do not seem feasible for implementation in rheumatology departments, among other things, because they utilize language that is not employed by rheumatologists.
It is interesting to highlight certain recommendations in which there existed some difference of opinion between rheumatologists and exercise specialists, that were eliminated from the final recommendations. For example, the group of exercise specialists coincided in that messages about exercise should be given very soon, even before the diagnosis, whereas the rheumatologists did not coincide, probably because the majority prefer having a clear diagnosis before initiating treatment, even if it does not involve drugs, in view of the fact that exercise, among other things, may be a contraindication. Again, there was not a wide acceptance among the rheumatologists regarding the specification of exercises, like squatting or getting up off a chair, or of utilizing material that is available at home for exercise, recommendations that seemed to receive general approval among the exercise specialists. Likewise, it was surprising to see the difference of opinion between one group and the other with respect to avoiding the prescription of exercises focusing on regions that were painful for the patient, clearly in favor of the exercise specialists, and not so clear among the rheumatologists. These differences of opinion demonstrate the importance of having a common, evidence-based training.
On the other hand, it would be necessary to reach greater consensus among all the users. To some extent, the evaluation and discussion on the part of those involved, both professionals and patients, would enable us to agree by consensus on an efficient implantation of these recommendations. We desisted from utilizing the Delphi technique outside the panel since the majority of the rheumatologists do not know the perspective of the exercise specialists and had not had the opportunity to discuss it with them, although the managing group of the recommendations did. The next phase of this project, which is already underway, is consisting precisely in promulgating the recommendations and to confirm their practical application in rheumatology departments. The perspective of the patient is crucial when it comes to engaging in exercise, given that it is an intervention is which: (1) the patient is part of it and (2) adherence has a significant influence on the effectiveness.9,33,37–42 In the first phase of the project, we asked the patients about exercise and their opinion of the recommendations given to them by different professionals and on the barriers.11 It was precisely the barriers that indicated what we needed to attempt to resolve with these recommendations. We can, however, stress as a limitation of this report, que after these recommendations were issued, the patients did not express any comments in this respect.
While the majority of the studies on exercise in patients with SpA refer to exercises involving the spine,8 these recommendations have not focused only on them. We have emphasized the role of aerobic exercise in all the stages of the disease. This fact makes these recommendations applicable not only to predominantly axial SpA, but to peripheral disease, as well.
The recommendations given in this document could be the outline to be followed in a department attending to patients with SpA. Although in some of the areas dealt with there is little evidence, many of these recommendations are relevant and are highly useful for clinicians, and have been supported by exercise specialists and rheumatologists with special interest in SpA.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingMerck Sharp & Dohme España financed the meetings and the methodological support of this consensus.
Conflicts of InterestNeither drugs or specific instruments from which the participants or financial backer could benefit economically as a cause of their utilization have been recommended in this document.
Please cite this article as: Flórez García MT, Carmona L, Almodóvar R, Fernández de las Peñas C, García Pérez F, Pérez Manzanero MÁ, et al. Recomendaciones para la prescripción de ejercicio físico en pacientes con espondiloartritis. Reumatol Clin. 2019;15:77–83.