To study the frequency of retinal toxicity and associated risk factors in a cohort of patients treated with antimalarials and seen at a tertiary level hospital.
Material and methodsRetrospective study of 40 patients treated with antimalarials, who were referred to ophthalmology for the study of retinal toxicity during 2011. Data collection included type of antimalarial prescribed, daily and cumulative doses, presence of rheumatic disease, corticosteroid use, associated diseases and ophthalmologic examination. Retinal toxicity was confirmed if two of the following tests were altered: fundus examination, visual field with a macular pattern, changes in spectral domain optical coherence tomography (SD-OCT) and full-field electroretinography (ERG).
ResultsToxic retinopathy was detected in 13.1% of patients (95% confidence interval 5%–21%) and a trend for a higher risk was observed in case of chloroquine (CQ) treatment. Among the patients with retinopathy, the mean cumulative dose was 229g for CQ and 111g for Hydroxychloroquine (HCQ), and the mean daily dose of CQ was 250mg and 333mg for HCQ. Arterial hypertension had a statistically significant effect on retinopathy development.
ConclusionsToxic retinopathy defined by ophthalmological evaluation was detected in 13.1% of patients. A trend for a higher risk was observed in case of chloroquine treatment.
Estudiar la frecuencia de toxicidad retiniana y factores de riesgo asociados en una cohorte de pacientes tratados con antipalúdicos de un hospital comarcal.
Material y métodosEstudio retrospectivo de 40 pacientes. Se recogieron: tipo de antipalúdico, dosis diaria y acumulada, enfermedad reumatológica de base, patología concomitante y estudio oftalmológico. Se definió toxicidad retiniana como alteración en 2 de las 4 siguientes pruebas: examen de fondo de ojo, campo visual con patrón macular, tomografía de coherencia óptica de dominio espectral (SD-OCT) y electroretinografía de campo completo (ERG).
ResultadosLa frecuencia de toxicidad retiniana fue 13.1% (95% intervalo de confianza [IC] 5-21%) con tendencia a un mayor riesgo en los pacientes en tratamiento con cloroquina. En estos pacientes con toxicidad retiniana, la dosis media acumulada de Cloroquina (CQ) fue de 229g y la de Hidroxicloroquina (HCQ) de 111g. La dosis media diaria de CQ fue de 250mg y la de HCQ fue de 333mg. Encontramos asociación positiva entre toxicidad retiniana e hipertensión arterial.
ConclusionesLa frecuencia de toxicidad retiniana, valorada objetivamente mediante técnicas oftalmológicas, fue alta, con una mayor tendencia en pacientes en tratamiento con cloroquina.
Hobbs in 1959 first reported retinal toxicity due to long term use of chloroquine (CQ).1 Currently, sulfate hydroxychloroquine (HCQ) is the most widely used antimalarial agent in the treatment of autoimmune diseases because of its lower incidence of adverse reactions although, like CQ, may produce ocular toxicity due to corneal and retinal deposition. Retinal involvement produces irreversible changes in vision and the patient may not perceive this, so regular eye tests are recommended.
Due to the difference found in the various studies and their frequent use in rheumatology, we is study to analyze the frequency of retinal toxicity and to identify associated risk factors in patients treated with antimalarials in the rheumatology clinic.
MethodsPatientsWe performed a retrospective study of 40 patients treated with antimalarials (CQ and HCQ) in the Rheumatology clinic and who were referred for consultation to Ophthalmology in 2011 followed systematically after a year of treatment to rule out ocular toxicity.
Inclusion criteria were: patients older than 18 years, current treatment with antimalarial due to rheumatic disease and who underwent an ophthalmologic examination in 2011. 2 patients were excluded prior to retinal disease (one was a drug user and another had a macular pseudoulcer), so the sample was 38 patients.
All patients signed informed consent and the study was conducted according to the Declaration of Helsinki.
Measurements and Data CollectionThe primary endpoint was defined as retinal toxicity secondary to drug damage, detected by alterations in at least 2 of the following tests: fundus examination, visual field with a macular pattern, optical coherence spectral domain tomography (SD-OCT) and full-field electroretinography or full-field (ERG), following the recommendations of the American Academy of Ophthalmology published in 2011.2
All patients were assessed for visual acuity in both eyes and underwent a slit lamp examination of the fundus under dilation and optical coherence tomography. In patients with suspected antimalarial toxicity using fundus examination and/or SD-OCT, we performed a visual field pattern covering the 10° macular central areas and ERG.
The secondary variables considered were: type of drug, daily and accumulated dose of CQ and HCQ, duration of treatment and renal function by serum creatinine determination.
AnalysisThe analysis of the association between retinal toxicity and antimalarial use was assessed by Chi-square test for qualitative variables and Student's t test for quantitative variables, with a confidence interval (CI) of 95%. The subanalysis of patients with retinal toxicity was performed using Fisher's exact test. Statistical analysis was performed using SPSS version 15.0 (Chicago). Statistical significance was considered at P<.05.
ResultsThe sociodemographic characteristics of the patients are shown in Table 1. 81.6% of patients were treated with HCQ, average daily dose 254mg mean cumulative dose±SD 251.3±182.2g. The average daily dose of CQ was 250mg and the mean cumulative dose was 371.5±377.2g. The mean treatment duration was 3.17±2.5 years. In all cases creatinine levels were normal.
Baseline Characteristics of Patients.
| Total sample | Retinal toxicity | |
| No. | 38 | 5 |
| Mean age, years±SD | 53.2±14.1 | 5.0±10.5 |
| Gender; n (%) | Women, 31 (81.6) | Women, 5 (100) |
| No. treatments of hydroxychloroquine, % | 31 (81.6) | 2 (40) |
| Chloroquine average daily dose, mg | 250 | 250 |
| Mean cumulative dose of chloroquine, g | 371.6±377.2 | 229.9±455.4 |
| Average daily dose of hydroxychloroquine, mg | 254 | 333 |
| Mean cumulative dose of hydroxychloroquine, g | 251.3±182.2 | 110.0±106.1 |
| Duration of treatment, years | 3.2±2.5 | 3.8±4.4 |
| Rheumatic disease | ||
| Rheumatoid arthritis | 16 (41) | 3 (60) |
| SLE, n (%) | 13 (33.3) | 2 (40) |
| Osteoarthritis, n (%) | 3 (7.9) | |
| Sjögren syndrome, n (%) | 2 (5.1) | |
| MCTD, n (%) | 2 (5.1) | |
| Other, n (%) | 2 (5.1) | |
| Concomitant corticosteroid treatment, n (%) | 19 (50) | 3 (60) |
| Hypertension, n (%) | 11 (28.9) | 4 (80) |
| Diabetes mellitus, n (%) | 5 (13.2) | 0 (0) |
| Hepatic/renal disease, n (%) | 0 (0) | 0 (0) |
| Complementary examinations | ||
| Positive SD-OCT, n (%) | 6 (15.8) | 5 (100) |
| Positive ERG, n (%) | 3 (7.9) | 3 (60) |
| Positive fundus, n (%) | 5 (13.2) | 2 (40) |
MCTD, mixed connective tissue disease; ERG, electroretinogram; g, grams; SLE, systemic lupus erythematosus; mg, milligram; SD-OCT, spectral domain optical coherence tomography.
Quantitative variables are expressed as mean±standard deviation (SD) and qualitative variables as n (%).
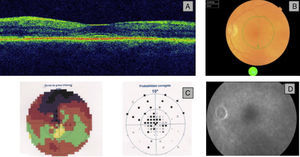
Retinal toxicity was detected in 5 of the patients evaluated (13.1%, 95%, 5%–21%). Three were treated with HCQ, with an average daily dose of 333mg and cumulative dose of 111g, and 2 treated with CQ, with an average daily dose of 250mg and cumulative dose of 230g. Four patients with retinal toxicity had a history of hypertension and 3 were taking corticosteroids at a dose less than 10mg or equivalent of prednisone/day. The 5 patients had an impaired SD-OCT while only 2 cases had the typical fundus image of bull's-eye maculopathy (Fig. 1). In the other 3 patients we detected alterations in the visual field and only 2 of these 3 had alterations in the ERG.
Using the SD-OCT we found alterations in the inner layers of the retina at the IS/OS line (junction of inner and outer segments of photoreceptors) consisting subfoveal hyperreflectivity with a double image line parallel to retinal pigment epithelium. In the visual field, the observed defect was variable depending on the degree of involvement, finding sensitivity decreased in the Bebie curve in the central visual field and an increase in mean defect and loss of variance. Using the ERG we observed low amplitude bilaterally in the electrical response of the retina.
No statistically significant association was found between retinal toxicity and type of drug. However, when analyzing separately the 7 patients treated with CQ we observed that 42.9% of them had an altered SD-OCT, P=.06.
We found a positive relationship between retinal toxicity and hypertension (P<.05). No significant association between retinal involvement and corticosteroid use, diabetes mellitus, age and sex of the patient, baseline rheumatic disease, duration and cumulative daily dose or treatment with antimalarials was seen.
DiscussionOur study showed a frequency of retinal toxicity in patients treated with antimalarials of 13.1%, with a greater tendency in patients treated with CQ. This frequency was higher than that found in most previous studies except1,3,4 Kobak et al.5 This may be due to the absence of standardized assessments to detect retinal toxicity, unlike our study where we followed the recommendations of the American Academy of Ophthalmology regarding screening of patients treated with antimalarials, and the use of new diagnostic methods of high precision (SD-OCT, ERG) which allow early detection. Thus, all patients underwent a fundus exam and SD-OCT, making it possible to identify a greater number of patients with retinal involvement. Moreover, Kobak et al. recognize that their study population may present a greater severity coming from a clinical research environment, which would explain why the frequency of retinopathy is greater.
Compared to patients in terms of the antimalarial used, we observed that patients treated with CQ tended to have an increased risk of retinal toxicity, and if the group had undergone a broader study it is likely that the difference had reached significance.
Among the factors associated with retinal toxicity, the most important were antimalarial treatment duration and daily dose, although we found conflicting results in different studies. In our study only found a positive association between retinal toxicity and hypertension. The induction of oxidative stress and endothelial dysfunction when there was hypertension6 could explain this finding, as it has been demonstrated that the two processes act as promoters of vascular damage and progressive atherosclerotic and thrombotic complications in vascular walls.
Regarding the clinical implications of our findings, all patients in whom retinal toxicity was detected were removed from antimalarial treatment, changing to other immunosuppressive drug for the underlying disease. In the 3 cases we detected early stage retinal toxicity by SD-OCT, without the typical bulls-eye maculopathy, with no significant changes in visual acuity that could affect the quality of life of patients.
Our study is not without limitations. First is the retrospective design. And, second is the sample size, which could condition the failure to identify risk factors associated with retinal toxicity secondary to antimalarial drugs.
However, the ophthalmologic evaluation sets our study apart from previous studies. Furthermore, in 3 of the 5 patients with retinal toxicity, SD-OCT was crucial because there were no other significant changes. Therefore, early changes in the outer layers of the retina assist the early detection of retinal toxicity and is particularly useful as SD-OCT is available in most hospitals and is highly sensitive and easy to perform in the clinical practice. In patients with SD-OCT and an altered visual field, the ERG helped confirm early stage toxicity.
In summary, the frequency of antimalarial retinal toxicity in our study was high, with a tendency to an increased risk in patients treated with CQ. An associated risk factor was hypertension, although this finding should be confirmed in future studies. We believe that standardized screening of patients treated with antimalarials is essential for early detection of retinal toxicity, although prospective studies are needed with larger sample sizes with new techniques available to confirm the results obtained.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that procedures conformed to the ethical standards of the committee responsible for human experimentation and were in accordance with the World Medical Association Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the author of correspondence.
Conflicts of InterestThe authors have no disclosures to make.
Please cite this article as: Palma Sánchez D, et al. Toxicidad retiniana por antipalúdicos: frecuencia y factores de riesgo. Reumatol Clin. 2013;9:259–262.