In our specialty the use of local corticosteroids is an extended practice, with the ones most commonly used being triamcinolone-acetonide and betamethasone disodium phosphate.1 There are many factors which may affect corticosteroids having undesirable systemic effects such as hyperglycaemia.2 This complication is of particular interest in diabetic patients who are candidates for these medical procedures.
Recently our team conducted a longitudinal historical cohort study to compare the hyperglycaemic effect of intra-synovial corticosteroid infiltrations.
Records of patients with locomotion pains attended between 2014 and 2015 in our hospital were reviewed. During this period our unit had a specific patient register which included a post infiltration follow-up programme which had been partially documented in a previous communication.3
The diabetic patient records were analysed where an ultrasound-guided infiltration had been performed and a follow-up file had been completed at least one month after. Only records of intra-articular and intrabursal infiltrations were included.
The available corticosteroids during this period were triamcinolone-acetonide (C24H31FO6, PM=434.5g/mol)4 and betamethasone disodium phosphate (C22H28FNa2O8P, PM=516.4g/mol)+3mg of betamethasone-acetonide (C29H33FO6, PM=496.6g/mol).5
The patients were grouped together depending on the corticosteroid administered. The dependent variables were the number of hyperglycaemias that required emergency medical assessment, changes to their antidiabetic treatment guidelines or the need for hospital admission.
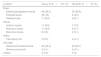
Two hundred and fifty eight infiltrations performed on 210 patients were analysed. Of these 210 patients 116 (55.2%) were male. The mean age was 50.3 years, SD: 7.8 (range: 19–92 years). The proportion of patients with a diagnosis of diabetes of over 10 years onset was 61.4%. During the follow-up period 161 infiltrations with betamethasone-acetonide (group A) were performed and 97 with betamethasone disodium phosphate and betamethasone-acetonide (group B). Table 1 shows the anatomical location of the infiltration distribution.
Distribution of infiltrations according to anatomical location. The magnitudes are expressed in absolute and percentile values with regards to their category.
| Location | Group A; N=161 (%) | Group B; N=97 (%) |
|---|---|---|
| Knee | ||
| External parapatellar recess | 46 (28.5) | 30 (30.9) |
| Popliteal bursa | 29 (18) | 9 (9.2) |
| Patellar bursa | 11 (6.8) | 6 (6.1) |
| Elbow | ||
| Anterior recess | 11 (6.8) | 7 (7.2) |
| Olecranon fossa | 11 (6.8) | 6 (6.1) |
| Olecranon bursa | 9 (5.5) | 5 (5.1) |
| Ankle | ||
| Tibia-talus joint | 9 (5.5) | 4 (4.1) |
| Shoulder | ||
| Subacromial deltoid bursa | 26 (24.2) | 23 (23.7) |
| Glenohumeral joint | 5 (3.1) | 4 (4.1) |
| Carpus | 4 (2.4) | 3 (3) |
Simple hyperglycaemia was recorded in 19 patients from group A (11.8%) and 11 patients from group B (11.3%) Simple hyperglycaemias which required emergency medical attention were recorded (P>.05). It was not necessary to change oral or insulin antidiabetic guidelines in any case. None of the patients were hospitalized.
Out of the total patients who received an infiltration at shoulder level with any corticosteroid (49), 11 presented with simple hyperglycaemia which required medical assessment. Of these 11 patients, 3 (37.5%) had been immobilised with the use of a sling and 8 had not. Of the 38 patients who did not present with simple hyperglycaemia and who were infiltrated at shoulder level, 34 (89.4%) were immobilised and 4 were not (P=.0001; exact Fisher's test). The age of the patients on infiltration administration, the date of diagnosis of diabetes, the type of antidiabetic treatment and the concomitant use of anaesthetics were not associated with the development of hyperglycaemias in the patients who were followed up (data not shown).
Recommendations for the use of low corticosteroid doses in infiltration to diabetic patients are the result of observational studies which did not exclusively include this type of patient.6,7 Systemic diffusion depends on several factors, including the molecular weight of the substance infiltrated, the integrity of the synovial membrane, its vascularity and the pressure within the synovial fluid cavity.2,8 We have only included ultrasound guided infiltrations aimed at reducing the possibility of extra synovial deposit, increasing procedural precision.9,10
We understand that both triamcinolone and betamethasone are comparatively safe corticosteroids since the proportion of hyperglycaemias that have required medical assessment was below 12% and also no hospital admissions were required.
Finally, it appears that immobilisation of the shoulder reduces the risk of hyperglycaemias, probably because the increase of pressure within the subacromial bursa is avoided, and this procedure could therefore be included within the recommendations for diabetic patients.
Please cite this article as: Guillen Astete CA, Diaz Garcia N, Laso Jimeno B, Luque Alarcon M. Seguridad de la administración de corticoides locales en pacientes diabéticos: estudio de cohortes históricas comparando el uso de triamcinolona y betametasona. Reumatol Clin. 2020;16:370–371.