We describe below the case of a patient with juvenile dermatomyositis, with extensive calcinosis which was refractory to standard treatment and which improved with the use of rituximab.
Calcinosis distinguishes juvenile dermatomyositis from the adult disease, of unknown pathogenesis. The deposit of calcium hydroxyapatite and phosphates in soft tissues with normal calcaemias form part of the inflammatory process of this disease, where the release of mediators such as interleukin 1 beta, interleukin 6 and anti-TNF alpha appear to play a role.1
Calcinosis occurs in 10%–70% of cases of juvenile dermatomyositis, heightening morbimortality. It usually presents between 1 and 3 years after diagnosis, but on occasions may appear at the beginning and on others 20 years later. Calcium deposits may appear on the skin, subcutaneous tissues, fascias or tendons, and may even form an exoskeleton in the severest of cases.1 Intensive fast treatment at the beginning of the disease with complete control of the inflammation can minimise the appearance of calcinosis.2
Our case was a 6 year old girl who had been previously healthy, who presented at the paediatric department at the beginning of 2009 with myalgias, abdominal pain and difficulty walking. The following were performed: lab tests which revealed elevated transaminases, LDH and CPK and an electromyogram which produced no changes. Clinical judgement diagnosed a non classifiable myopathy, no treatment was administered and medical symptoms spontaneously improved.
In August 2009, medical symptoms worsened, with CPK up to 3000u being detected. She was referred to the rheumatology department where the electromyogram was repeated and was compatible with proximal myopathy. Conclusive muscle biopsy confirmed inflammatory myopathy compatible with juvenile dermatomyositis: perivascular inflammatory lymphocytary infiltration.
Treatment was initiated with 30mg/kg of weight methylpredinisolone boluses for 3 consecutive days and oral prednisone and 15–25mg sc methotrexate per week.
Despite the normalisation of the muscle enzymes, clinical symptoms worsened, proximal muscle strength diminished and cyclosporine was added (up to 4.5mg/kg).
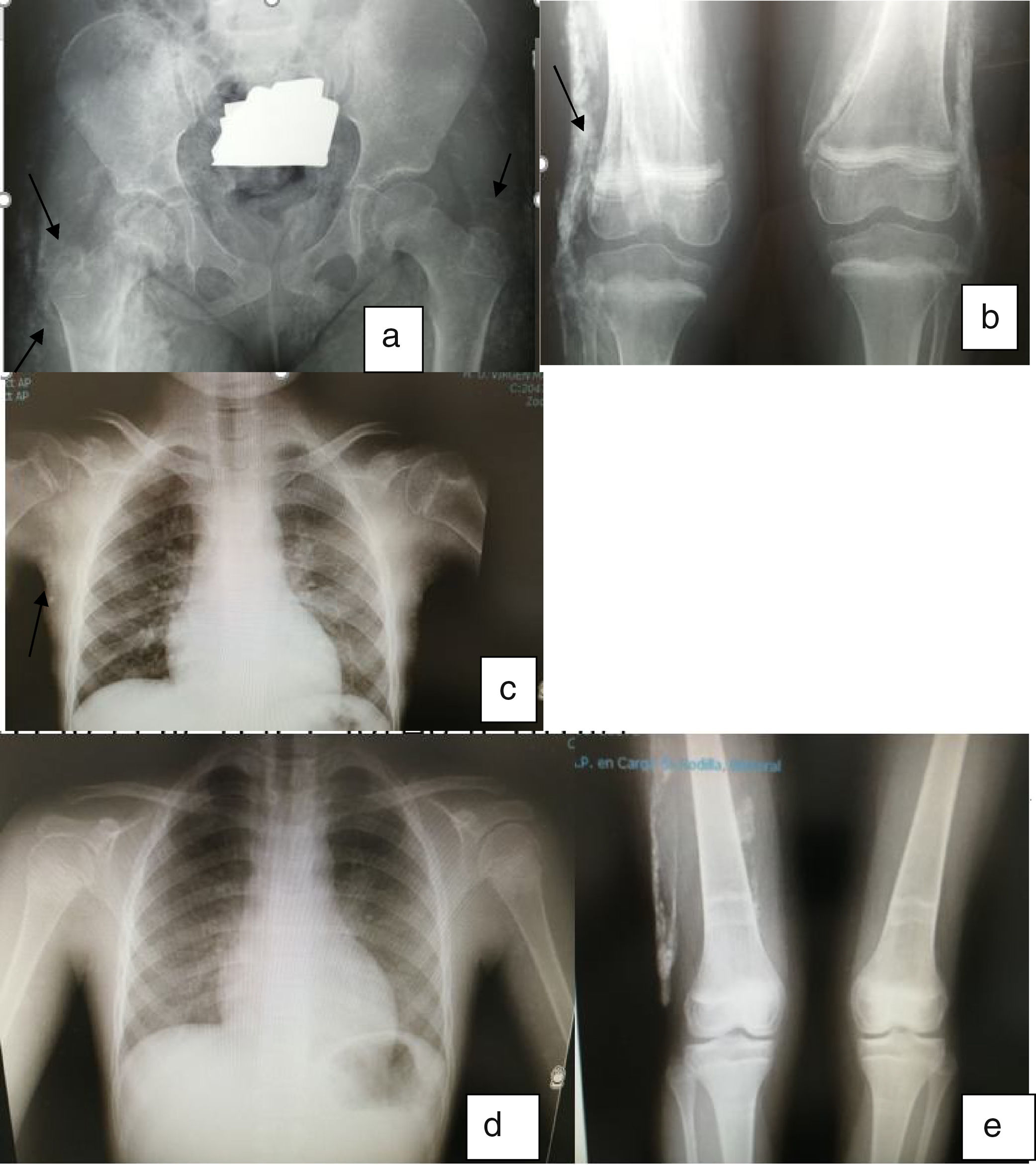
In November 2010 the joint contractures increased and the patient presented with calcinosis. In January 2011 30mg IV pamidronate on 3 consecutive days was administered quarterly and 25mg etanercept per week with no improvement and NMR showed evidence of inflammation in the hip joints. In September 2011 etanercept was suspended and compassionate use of 375mg/m2 rituximab in 4 doses was requested. In April 2012 progressive improvement was made with recovery of muscle strength, disappearance of skin lesions and gradual improvement and disappearance of calcinosis (Fig. 1).
In January 2016 immunosuppresion was suspended after 2 years in clinical and analytical remission. In January 2018 strength was normal, with no joint contractures or skin lesions and with normal lab test results.
There is no one generally accepted treatment for calcicosis secondary to juvenile dermatomyositis. Different drugs have been used including colchicine, warfarin, intravenous inmunoglobulin, thalidomide and calcium channel inhibitors.
Biphosphonates, particularly pamidronate have been shown to be effective in small patient series.3–7 Rituximab depletes positive CD20 lymphocytes, which are abundant in muscles and peripheral blood in patients with myositis. Few cases in the literature describe the effect on calcinosis.
In our patient the inflammatory activity control, which was not achieved with standard treatment protocols, was the underlying reason for the regression of the calcinosis, in the opinion of her doctors.8–10 We were unable to determine how much effect the cycles of pamidronate had.
Although we are unable to advocate the use of rituximab in calcinosis of this or other origins (studies are required to demonstrate its use), we have cited this case due to the temporal relationship of the improvement both of the myositis and the calcinosis with the use of rituximab and the depletion of lymphocytes. At present the patient is 15 years old and has been in remission for over 4 years, the first 2 with methorexate and the last 2 without immunosuppressants.
Please cite this article as: Vargas Lebrón C, Ruiz Montesino MD, Moreira Navarrete V, Toyos Sainz de Miera FJ. Tratamiento con rituximab en dermatomiositis juvenil. Efecto sobre la calcinosis. Reumatol Clin. 2020;16:368–370.