The acronym of SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis) combines a cluster of cutaneous and musculoskeletal manifestations, such as hyperostosis of bones of the anterior chest wall associated with acne fulminans and hidradenitis suppurativa. There are no validated diagnostic criteria in children. Nonsteroidal anti-inflammatory drugs are not always sufficient, and the use of corticosteroids, disease-modifying agents, tumor necrosis factor-α inhibitors or bisphosphonates may be necessary.
We present the case of a child with polyarticular involvement, osteoarthritis of the sternoclavicular joint with severe inflammatory disorders and acne conglobata, with an excellent response to intravenous pamidronate.
El acrónimo síndrome SAPHO (sinovitis, acné, pustulosis, hiperostosis y osteítis) engloba tanto manifestaciones cutáneas como muculoesqueléticas, entre ellas hiperostosis de los huesos y de las articulaciones de la pared torácica anterior, asociado a manifestaciones cutáneas; acné fulminans e hidradenitis supurativa. Los criterios diagnósticos no han sido validados en niños. El tratamiento inicial con antiinflamatorios no esteroideos en ocasiones es insuficiente y puede ser preciso asociar corticoides, fármacos modificadores de la enfermedad, antagonistas del factor de necrosis tumoral o bifosfonatos.
Presentamos el caso clínico de un escolar con afectación poliarticular, osteoartritis de articulación esternoclavicular con importante componente inflamatorio y acné conglobata, con buena respuesta al tratamiento con pamidronato por vía intravenosa.
SAPHO syndrome was proposed for the first time in 1987 by Chamot et al.1 It encompasses a series of skin and osteoarticular manifestation that include synovitis, acne, pustulosis, hyperostosis and osteitis.2 These manifestations are the basis from which the acronym was coined and enable us to unify clinical disorders that had previously been described independently.
The prevalence of this condition is not clearly established, although the majority of the series estimate it to be less than 1 per 10,000 population.2 It mostly affects children and young adults. The predominance in terms of sex is controversial at the present time, there being series with a female predominance3 and others in which there is no difference between the two sexes.4
The origin of this disorder is still unknown. A multifactorial cause has been proposed, in which Propionibacterium acnes, an anaerobic bacterium implicated in acne lesions, has been isolated in cultures from areas of osteitis. To a lesser extent, other bacteria of lower virulence have also been isolated, and could provoke a dysfunction or activation of either the innate immune system or that mediated by T cells in genetically predisposed individuals.2,5,6
Case ReportThe patient was a 13-year-old boy, with constitutional symptoms that had begun 1 month earlier and a weight loss of up to 7kg. He had low-grade fever in the evenings, morning stiffness and osteoarticular pain affecting different sites that woke him up during the night and impeded him from engaging in daily activities. He had marked inflammation in right sternoclavicular joint and involvement of both sacroiliac joints. It was associated with acne conglobata on his face, back and axillae, which developed 2 months prior to the musculoskeletal symptoms. He had no significant personal or family history.
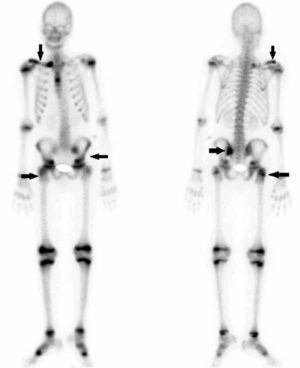
Bone scintigraphy demonstrated pathological deposits of localized uptake at the level of both epiphyses of right clavicle (more evident in the proximal region), in elbow and greater trochanter of right femur, left sacroiliac joint and the base of the first metatarsal bone of both feet (Fig. 1). Conventional radiography showed hyperostosis at the end proximal to right clavicle. Magnetic resonance imaging (MRI) revealed extensive subcortical bone marrow edema on both sides of the left sacroiliac joint, highly indicative of sacroiliitis. There was subcortical bone marrow edema in both acetabula, in greater trochanter and in right intertrochanteric region, indicative of osteitis (Fig. 2). Ultrasound examination of the joint revealed synovitis in right elbow and knee. Blood test showed elevated inflammatory markers, with an initial erythrocyte sedimentation rate of 80mm/h and C-reactive protein of 18.8mg/L, and human leukocyte antigen (HLA) B27 was negative, as were autoimmunity and rheumatoid factor. The level of alkaline phosphatase was normal for the boy's age. Cultures and serological tests were negative.
The patient underwent bone biopsy of right greater trochanter as it was the most accessible region with a pathological result compatible with fibrosis of the cortical bone, but no other finding, thus ruling out tumor and an infectious process.
First-line treatment was initiated with nonsteroidal anti-inflammatory drugs (NSAID), starting with ibuprofen (15mg/kg body weight [bw]/dose) and later with indomethacin (25mg/8h), with a partial response. During the study, the patient also received a cycle of intravenous cloxacillin, followed by oral administration. After the biopsy, given the suspicion of SAPHO syndrome, therapy was begun with intravenous pamidronate, for a total of 5 cycles (1cycle/month). Although the drug was well tolerated, during its administration, the patient developed adverse effects such as fever and diarrhea. Both the constitutional symptoms and the osteoarticular pain and stiffness disappeared after treatment with pamidronate was begun, enabling a reduction in the anti-inflammatory dose and their ultimate discontinuation after a second cycle. The levels of inflammatory parameters were also normalized.
DiscussionSAPHO syndrome is a rare, chronic, recurrent condition. The diagnosis requires a high index of suspicion, especially when atypical joints are affected or the skin manifestations are absent.
Osteoarticular involvement is usually insidious, in the form of osteitis, hyperostosis, synovitis, arthropathy or enthesopathy, accompanied by pain that can occasionally be disabling and worsens with mobilization. There can also be swelling, redness, warmth or decreased range of motion in the affected region, as well as morning stiffness or a limp if the long bones are included. Likewise, osteitis, understood to be inflammation of the bone, can affect the cortical bone, bone marrow or both, whereas hyperostosis can provoke joint fusion due to excessive bone growth.6 On the other hand, systemic manifestations are uncommon, although fever or elevations of acute-phase reactants may be observed.2
The distribution of osteoarticular lesions depends on the age of the patient at onset, with predominance of the sternoclavicular region throughout adolescence, whereas in children it mainly affects long bones and, with a wide variability, the lumbar spine and pelvis.7
Arthritis is present in more than 90% of the cases and usually occurs in joints adjacent to the affected bones, both in children and in adults. The sternoclavicular and sternocostal joints are those most frequently affected, followed by knees, hips and ankles, and, less commonly, the small joints of the hands and feet.5,6 Finally, there are reports of a few patients with involvement of the temporomandibular joint.6
Synovitis is seldom encountered in children5 and enthesopathy can result in ossification of the ligament and, ultimately, the development of bony bridging across the joints.6
Skin manifestations can develop at the same time as the osteoarticular symptoms and signs, but also years before or after or even fail to appear at all, although the interval is usually less than 2 years. Palmoplantar pustulosis is the most common manifestation, followed by acne conglobata (predominantly in boys) and hidradenitis suppurativa (predominantly in girls). They are quite resistant to therapy and have a chronic, prolonged course.2,5,6
The diagnosis may be straightforward when the typical bone lesion localizations are involved in the presence of radiographic findings, such as hyperostosis and osteitis, together with the skin manifestations. Likewise, there are no validated diagnostic criteria, although in some cases, physicians utilize the inclusion and exclusion criteria established by Benhamou et al. (Table 1) or those of Kahn, modified in 2003 (Table 2).6
Inclusion and Exclusion Criteria for SAPHO Syndrome.
| Inclusion criteria | Osteoarticular manifestations with acne conglobata, acne fulminans or hidradenitis suppurativa Osteoarticular manifestations with palmoplantar pustulosis Hyperostosis with or without dermatosis Chronic recurrent multifocal osteomyelitis affecting the axial or peripheral skeleton, with or without dermatosis |
| Possible criteria | Psoriasis vulgaris Inflammatory enteropathy Characteristics of ankylosing spondylitis Presence of low-virulence bacterial infections |
| Exclusion criteria | Septic osteomyelitis Septic arthritis affecting the chest wall Infectious palmoplantar pustulosis Diffuse idiopathic skeletal hyperostosis, except for fortuitous association Osteoarticular manifestations caused by retinoid therapy |
SAPHO: synovitis, acne, pustulosis, hyperostosis and osteitis.
Diagnostic Criteria Proposed by Kahn and Modified in 2003.
| Inclusion criteria | Osteoarticular involvement associated with palmoplantar pustulosis Osteoarticular involvement associated with severe acne Sterile hyperostosis/osteitis (adults)a Chronic recurrent multifocal osteomyelitis (children) Osteoarticular involvement associated with chronic bowel diseases |
| Exclusion criteria | Infectious osteitis Tumor-like conditions of the bone Noninflammatory condensing lesions of the bone |
With respect to ancillary tests, plain radiography offers little yield in early stages, with series in which only 16% of the lesions visualized by MRI are said to be detected. However, on occasion it enables the detection of osteitis and hyperostosis with cortical thinning, periostitis and ossification of the ligament, which are especially visible in later stages.2,6 Magnetic resonance imaging enables us to monitor the activity of the disease by differentiating between active and chronic lesions, as well as to visualize bone marrow edema and soft tissue inflammation.6 On the other hand, it avoids subjecting children to ionizing radiation.5 Bone scintigraphy has a fundamental role for locating clinically silent sites of involvement and, occasionally, it makes it possible to rule out infections and tumors. Moreover, it has a very high sensitivity for the anterior chest wall and, at times, shows uptake in sternoclavicular joints with a typical bull's head aspect, a finding that is very characteristics of SAPHO syndrome.7,8
All of these examinations help to determine the diagnosis and initiate early treatment, avoiding the progression of the osteoarticular lesions. They also make it possible to differentiate other processes, such as osteomyelitis, bone metastases or other spondyloarthropathies, although, on occasion, it is necessary to resort to biopsy to establish the definitive diagnosis and rule out other conditions. Chronic recurrent multifocal osteomyelitis is a particular case. It is still debated whether it is a pediatric form of SAPHO syndrome or do the two constitute distinct disorders, as is shown by the series of Kaiser et al.2,5–7,9
Standard treatment consists of NSAID, corticosteroids and disease-modifying antirheumatic drugs, like methotrexate, sulfasalazine and azathioprine, which have been found to be effective in certain cases. Whereas, biological agents such as infliximab and bisphosphonates are reserved for refractory disease. Of the latter, pamidronate, with its anti-osteoclastic and anti-inflammatory activity, suppresses the production of proinflammatory cytokines like interleukin (IL)-1, IL-6 and tumor necrosis factor (TNF)-α. It is the most widely utilized drug of this class and responds very rapidly by reducing pain and improving function with few adverse effects.5,6 This was demonstrated in the series reported by Kerrison et al.10 in 2004 and that of Miettunen et al.11 in 2009. The dose of pamidronate and the dosage interval have not been established, although it is generally administered in intravenous cycles at doses of 1mg/kg bw with a maximum of 30–60mg/day. The cycles are administered on a single day or 3 consecutive days at intervals that range between 1 and 3 months, although, on occasion, there may be periods during which the patient notes the absence of symptoms.5,10,11
On the other hand, due to the possible participation of P. acnes in SAPHO syndrome, antibiotic therapy is also part of the conventional treatment. It usually involves azithromycin because of its antimicrobial, anti-inflammatory and immunomodulatory activities, and doxycycline, although, in general, they have not shown to have a great effect, except in cases in which there was a positive culture.2,5,6
Tumor necrosis factor-α is a proinflammatory cytokine and a regulator of other cytokines like IL-1, IL-6 and IL-8, which also intervene actively in the inflammatory process.
With respect to infliximab, there have been reports of a number of case series in which the response was good in terms of both the skin and musculoskeletal lesions, with the exception of palmoplantar pustulosis, which does not always respond to treatment. In fact, there have been cases in which the exacerbation of skin manifestations has been detected.6
Other anti-TNF agents, like etanercept and adalimumab, have been utilized with good results. Yet, although in other chronic inflammatory diseases, infliximab is preferred over other anti-TNF drugs, because of its rapid action, no differences have been demonstrated in SAPHO syndrome.12 On the other hand, 2 isolated cases of subcutaneous administration of certolizumab pegol and ustekinumab, both as monotherapy, with improvement in joint and skin manifestations and, to date, no clinically relevant adverse effects, although more extensive experience will probably still be necessary.
Likewise, the demonstration of patients who respond to anakinra opens the door to drugs that neutralize the IL-1 pathway, especially for those who do not improve with anti-TNF agents. Thus, we are very interested in reading the publication of the medium-to-long-term results with this drug.13
In any case, biological agents have mostly been utilized in patients with chronic SAPHO syndrome, generally once conventional treatments have failed.
Surgery is reserved for the treatment of deformities secondary to the progression of the disease and for patients with a poor response to medical treatment.
The course of the disease is generally highly variable, although the majority of the patients have a chronic pattern with exacerbations separated by short periods of improvement or a course of relapses and remissions, more typical in children, with intervals of weeks to months, even years. The factors identified as predictors of a chronic course are female sex, involvement of anterior chest wall, peripheral arthritis, skin lesions and high levels of acute-phase reactants at the time of diagnosis.3
The prognosis is relatively good, even in patients with chronic involvement, who also tend toward a progressive improvement, and disabling complications are rare.5
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe present report has not received any type of funding.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Vargas Pérez M, Sevilla Pérez B. Síndrome SAPHO en la infancia. Presentación de un caso clínico. Reumatol Clin. 2018;14:109–112.