We report a case of acute-onset multifocal vertebral osteitis with a marked impact on the patient's general health. The radiological, scintigraphic and magnetic resonance findings made it necessary to carry out a differential diagnosis to distinguish it from an infiltrative neoplastic process and determine whether it had an infectious or an inflammatory etiology. The presence of noninfectious multifocal osteitis and sternoclavicular arthritis and the subsequent development of plantar pustulosis pointed to SAPHO syndrome. Treatment with infliximab led to improvement in the clinical symptoms, laboratory values and radiological abnormalities.
Se expone un caso de osteítis vertebral múltiple de presentación aguda con marcada afectación del estado general. Los hallazgos radiológicos, gammagráficos y de resonancia magnética obligaron al diagnóstico diferencial de un proceso neoplásico infiltrativo y de un origen infeccioso vertebral frente a la etiología inflamatoria. Por la presencia de osteítis múltiple no infecciosa, artritis esternoclavicular y la ulterior aparición de pustulosis plantar, se orientó como síndrome SAPHO. El tratamiento con infliximab consiguió la mejoría clínica, analítica y de las alteraciones radiológicas.
SAPHO syndrome has different clinical forms of presentation, which combine the manifestations of arthritis, acne, pustulosis, hyperostosis and osteitis, in a variable manner. The most common bone involvement is that observed in anterior chest wall, followed by the vertebrae and the sacroiliac joints.1,2 Its classification continues to be a subject of debate, and its limits with regard to some types of psoriatic arthropathy and pustular psoriasis are little defined.3 Although it is an inflammatory disease, the aggressiveness of certain forms of onset are suggestive of an infiltrative neoplastic process or vertebral osteomyelitis, as in the case we report here.
Clinical ObservationThe patient was a 53-year-old woman who came to rheumatology after 2 months of apparently inflammatory cervical pain, which produced a marked functional limitation. The pain had progressively extended to the thoracic and lumbar spine. She had no fever, prior evidence of infection, previous surgery or recent dental procedures. She had come to the emergency department of the hospital 3 times, where she had received analgesic and anti-inflammatory treatment, with no clinical improvement. Her primary care physician prescribed prednisone (10mg/day) and referred her to rheumatology for evaluation. The patient arrived with her general health undermined, with a marked limitation of the mobility of her cervical spine, and was admitted to the hospital to be studied.
The physical examination at admission showed stiffness and intense pain on any attempt to move her cervical spine. She felt pain in response to pressure on the lumbar spinous processes, with no evidence of radiculopathy and preserved deep tendon reflexes.
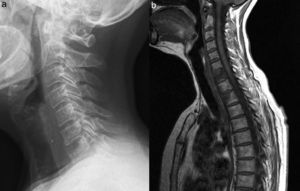
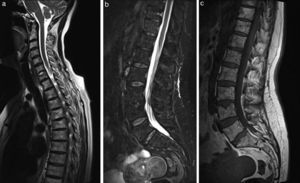
Radiography of the cervical spine showed an osteolytic lesion in the anterosuperior margin of the vertebral body of C7 (Fig. 1a). Radiographies of thoracic and lumbar spine revealed diffuse osteopenia with no vertebral collapses and grade I degenerative spondylolisthesis at L5. The analysis at admission showed an erythrocyte sedimentation rate (ESR) of 72mm/h and C-reactive protein (CRP) of 13.4mg/L (normal <5mg/L), and a complete blood count, liver function tests, creatinine, creatine kinase, lactate dehydrogenase, cholesterol, triglycerides, electrolytes and proteins were normal. Serologic tests for hepatitis B and C viruses and Brucella were negative. Tumor markers (CEA, CA 15-3, CA-125, CA 19-9) and β2-microglobulin were within normal limits. Serum calcium and phosphate were normal, parathyroid hormone was 27.8pg/mL and calcidiol was 7.8ng/mL.
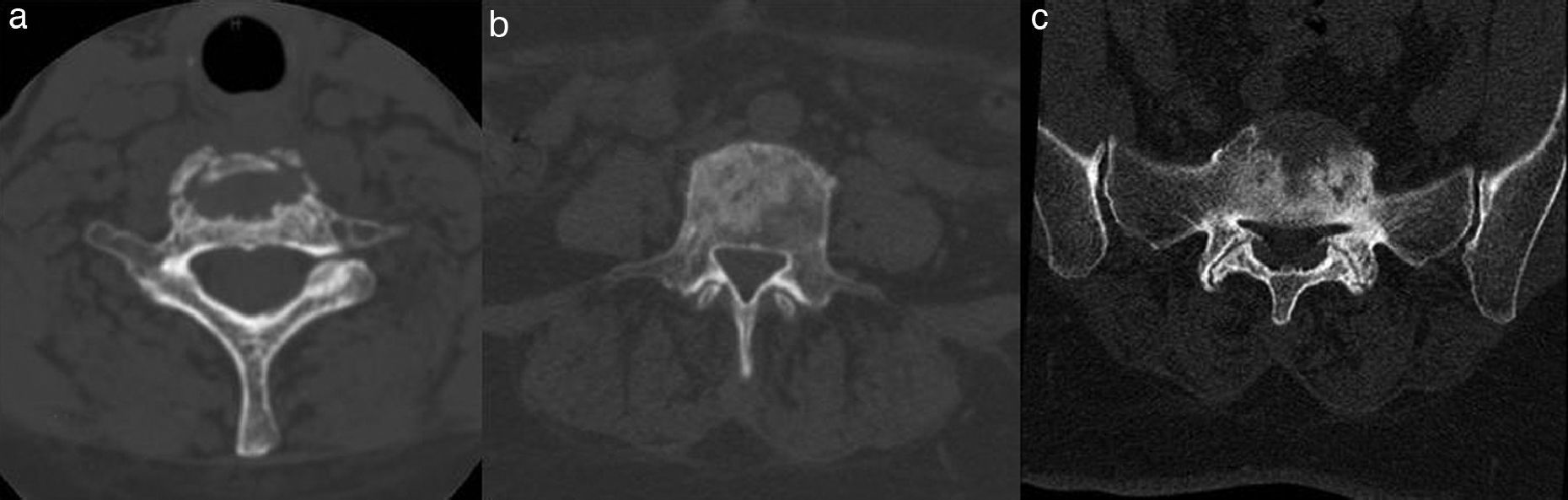
Osteolytic lesion of the anterosuperior segment of the vertebral body of C7 (a). Sagittal magnetic resonance T1-weighted image of the cervicothoracic spine (b). Diffuse abnormality of the bone marrow signal of vertebral body C7, with collapse and probable erosion of the superior vertebral endplate. Focal involvement of a similar signal intensity and involvement of the anterior half in vertebral bodies of thoracic T1 and T2. We observe the component of soft tissue aligned in front of vertebral bodies from C4 to C7. The signal pattern is compatible with substitution of normal bone marrow.
Bone scintigraphy showed foci of moderately increased uptake in C7, and in thoracic, lumbar and sacral spine, there were no foci with uptake outside the spinal column.
Magnetic resonance imaging (MRI) of the spine revealed an abnormality in the vertebral body signals, which was diffuse in C7 (Fig. 1b) and patchy in the anterior half of T1 and T2, with collapse of the superior endplate of C7 (Figs. 1a and 2a), and soft tissue components in front of the vertebral bodies that extended from C4, aligned like a column, to T1/T2, with the most marked involvement in front of C7. An alteration was observed in the bone marrow signal of the left pedicle-lamina of T4 (Fig. 2b). We also detected an abnormality in the signal in different vertebral bodies of the thoracolumbar spine (T11, T12, L1, L3, L4, L5, S1), as well as in left pedicle of L1 (Figs. 2c and 3a and b). The distribution of the lesions was related to the joint surfaces in every case.
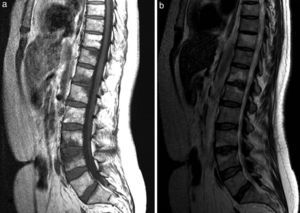
Sagittal T1-weighted image of thoracolumbar spine (a). Abnormality of the focal bone marrow signal, in relation to superior vertebral endplates at T11, and endplates at T12/L1 and L3/4. Involvement of L3/4 is associated with collapse of the superior vertebral endplate, with irregular margins. Sagittal T2-weighted image of thoracolumbar spine (b), which shows T2-weighted hyperintensity corresponding to the abnormal areas in the T1-weighted signal, compatible with a pattern of substitution of normal bone marrow due to reactive/inflammatory edema given the relationship to joint surfaces.
Thoracoabdominal computed tomography (CT) and ultrasound were normal.
Guided by CT, we performed fine-needle aspiration and vertebral bone biopsy (L3–L4), which showed bone and hematopoietic tissue with the presence of plasma cells, but no evidence of malignant cells.
During her hospital stay, the patient developed pustular lesions on the soles of both feet, a sign that she had not shown until then. Acne appeared on her chest and back, with certain scarring lesions. She also felt pain in her sternoclavicular joints, with mild local inflammatory signs.
The tuberculin test, that is, a purified protein derivative (PPD) test, and the detection of interferon gamma in blood for tuberculosis (Quantiferon®) were negative.
The case was managed like noninfectious multiple vertebral osteitis associated with pustulosis (SAPHO). Given the absence of a clinical control with anti-inflammatory therapy (naproxen, indomethacin), she began with intravenous infliximab (5mg/kg in weeks 0, 2, 4 and, thereafter, every 8 weeks).
During follow-up in our outpatient clinic, the patient underwent sacroiliac CT that showed degenerative signs with no evidence of sacroiliitis. A test for HLA B27 was negative.
Rapid clinical improvement was noted from the start of infliximab, with normalization of acute-phase reactants 3 months later. An MRI repeated 1 year after she began her treatment demonstrated the resolution of the abnormality of the signal in cervical, thoracic and lumbar vertical bodies (Fig. 4). The disk at C6–C7 showed residual changes with a hernia in spongy bone. The disappearance of the soft tissue component in front of the vertebral bodies of C4–C5 was observed. The abnormality in the signal of left pedicle and lamina of T4 also persisted. There were no new lesions.
Sagittal T2-weighted image of cervicothoracic spine (a), which shows a diffusely heterogeneous bone marrow signal, with no focal areas of prominent signal in the bodies affected in the aforementioned figure. The focal collapse of superior vertebral endplate at C7 persists. Sagittal short tau inversion recovery (STIR) image of the thoracolumbar spine (b), which shows a homogeneously suppressed bone marrow signal, without the areas of edema described in the legend to Fig. 3(b). Sagittal T1-weighted image of thoracolumbar spine (c), showing a bone marrow signal that is diffusely heterogeneous regarding the predominant T1-weighted hyperintensity pattern, compatible with a predominance of fatty bone marrow in all the vertebral bodies. The focal collapse/and hernia in spongy tissue in the superior endplate of L4 persist as chronic aspects.
Fifteen months after the diagnosis, the patient continues to receive treatment with infliximab, with a good clinical response (visual analog scale, 20/100) and normalization of ESR and CRP, although the plantar pustulosis persists.
DiscussionThe diagnosis of SAPHO is clinical and is eminently reached by exclusion. Given its clinical and radiological expression, the differential diagnosis includes osteomyelitis, lymphoma, osteosarcoma, bone metastases, psoriatic arthropathy, Paget's disease, Tietze's syndrome and Sweet syndrome.4 The diagnosis is a clinical challenge, since frequently the different manifestations that conform the syndrome do not appear at the same time. On the other hand, although it is a benign inflammatory condition, it is prudent to keep in mind certain serious complications, such as associated deep vein thrombosis5 or pachymeningitis.6 In most cases, the disorder is chronic, with episodes of exacerbation, or can follow an indolent course. However, occasionally, the onset of the disease may be acute and disabling, as in the case we report. Factors that have been suggested to be related to chronicity are female sex, involvement of anterior chest wall, peripheral arthritis, skin lesions and elevation of acute-phase reactants at the beginning of the disease.7 On the basis of these criteria and the marked functional involvement of the patient, we decided to initiate treatment with infliximab, in addition to nonsteroidal anti-inflammatory drugs, ruling out the use of intravenous bisphosphonates.
The radiological findings may be characteristic, given the involvement of anterior chest wall. However, the diagnosis may be even more difficult when vertebral lesions predominate, especially if lytic lesions predominate over sclerotic changes. The contribution of radiologists in the diagnosis is fundamental, as unnecessary studies and biopsies can be avoided.8
ConclusionsVertebral osteitis in SAPHO syndrome can present as multiple osteolytic lesions. Treatment with anti-tumor necrosis factor-α drugs is effective in controlling clinical manifestations and can improve the radiological and MRI outcome of the bone lesions.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Mateo L, Sanint J, Rodríguez Muguruza S, Martínez Morillo M, Pérez Andrés R, Domenech Puigcerver S. Lesión osteolítica cervical como presentación del síndrome SAPHO. Reumatol Clin. 2017;13:44–47.