Simulation is frequent in spinal disease, resulting in problems for specialists like Orthopedic Surgeons, Neurosurgeons, Reumatologists, etc. Simulation requires demonstration of the intentional production of false or exaggerated symptoms following an external incentive. The clinician has difficulties in demonstrating these criteria, resulting in misdiagnosis of simulation or misinterpretation of the normal patient as a simulator, with the possibility of iatrogenic distress and litigation.
We review simulation-related problems in spine, proposing a terminological, as well as a diagnostic strategy including clinical and complementary diagnosis, as a way to avoid misinterpretation and minimize the iatrogenic distress and liability.
Based on the clinical-forensic author's expertise, the literature is analyzed and the terminology readdressed to develop new terms (inconsistencies, incongruences, discrepancies and contradictions). Clinical semiology and complementary test are adapted to the new scenario. Diagnostic strategy relies on anamnesis, clinical and complementary tests, and adapting them to a uniform terminology with clear meaning of signs and symptoms.
La columna es terreno abonado para la simulación, involucrando a diferentes Especialistas (traumatólogos, neurocirujanos, rehabilitadores, médicos de familia, etc.). La simulación requiere la producción intencional de síntomas exagerados o falsos respondiendo a un incentivo externo. Sin embargo, en la práctica, hay dificultades en la demostración de dichos requisitos. Esto origina que algunos simuladores no resulten identificados y que pacientes no simuladores con actitud incongruente sean etiquetados de rentistas, originando distrés iatrógeno y exposición a litigación.
Se analiza la simulación en el raquis, proponiendo una modificación terminológica, así como una nueva estrategia de diagnóstico, para evitar errores y reducir tanto el distrés iatrógeno como la ligitabilidad.
Basándonos en la experiencia clínico-forense de los autores, se analiza la bibliografía y se propone una semiología uniforme. El abordaje es multidimensional y la estrategia de diagnóstico basada en: anamnesis, exploración y pruebas complementarias, adaptando sus resultados a una terminología uniforme con significado preciso de signos y síntomas.
One of the main problems with simulation is the lack of terminology to avoid, on the one hand, derogatory epithets (“liar, simulator, etc.”), and, on the other, to properly classify suspicious behavior.1
The international classification of mental disorders (DSM)2 defines simulation as the “intentional production of disproportionate or false physical or psychological symptoms, motivated by external incentives.” This definition does not serves to characterize many patients with spinal problems because, first, it requires checking a ‘lack of proportion’ or ‘falsehood’ in the symptoms, which is not easy. Furthermore, it is common that the doctor cannot be sure that there is “willful” or “intentional” pretense by a given patient.
Other classifications, such as the International Classification of Diseases (ICD-10),3 also serve to characterize these cases. In fact, these terms remain in the “rent neurosis”, a diagnosis that requires demonstration, always difficult, of an expectation of economic gain.4
Other commonly used terms are ambiguous when not derogatory (compensation neurosis, sinistrosis, etc.).
This scenario is compounded by the scarcity in the literature of reviews on systematic simulation, having, at most, small series or studies with a single disorder. Similarly, there are few studies to establish the validity of the simulation detection systems. It has been suggested, therefore, that there is a need to foster research on the matter and that medical professionals critically examine this.5
For these reasons, we propose to review the controversial topic of simulation in spinal diseases, where the suspected style responses or magnification of the ailments are very common.
We intend to propose an integrated terminology in both clinical assessment and reporting. We believe that a conceptual redirection of the problem as well as a unified terminology may be the key to correctly diagnose each case, reduce iatrogenic distress and minimize potential legal qualifiers linked to stigmatizing the real patient or lead to material damage.
Materials and MethodsA review of the literature was performed and possible changes of terminology based on the multidisciplinary expertise of the authors, who combine accreditation and experience in clinical and spinal surgery, as well as Legal, Forensic Medicine and evaluation of the problem are discussed. New terminology, as well as a set of clinical maneuvers whose significance is critically analyzed, is proposed. This aims to achieve a test report based on the meaning of interrogation, patient history and clinical examination. This terminology also extends to additional tests, mainly the so-called functional or biomechanical testing.
ResultsThe results of the literature review, critical analysis and professional review, led to a number of key elements, which are given below.
Need for Appropriate TerminologyIt is necessary to refer to a unified language when referring to simulation.
As a model for the approach to these questions, we part from the terminology proposed by Rogers et al.6 This author speaks of “non-credible response style” (NCRS) to describe behavior that seems unlikely in its presentation to the clinician.
However, in practice, most of the time, it is not clear that if the patients distort their symptoms. What we usually see is inappropriate or discordant responses in comparison with the entity's objective disorders. We could talk of a “style of abnormal or distorted response” (SADR).1
The real simulation (RS) implies the existence of intended exaggeration or falsehood responding to external incentives, which implies checking those criteria. That is, the fraudulent presumption should be endorsed by objective factors. This concept is equivalent to the terminology used in ICD-10.3
Multidimensional Screening Strategy for the Detection of the Patient With a Distorted Response StyleIt should be based on clinical and complementary elements. One of the best studies to date regarding simulation of spinal disorders was written by Hernandez Conesa.7 In this paper, 4 simulation clinical markers (inconsistencies, incongruity, discrepancies and contradictions) were identified. We propose these as signs of SADR. In addition, these markers can also be applied to the results of laboratory research. It may be the number, but, above all, the nature of these factors that can guide us to a style of unreliable responses (NCRS) or a real simulation (RS).
We now consider the elements of clinical and complementary detection.
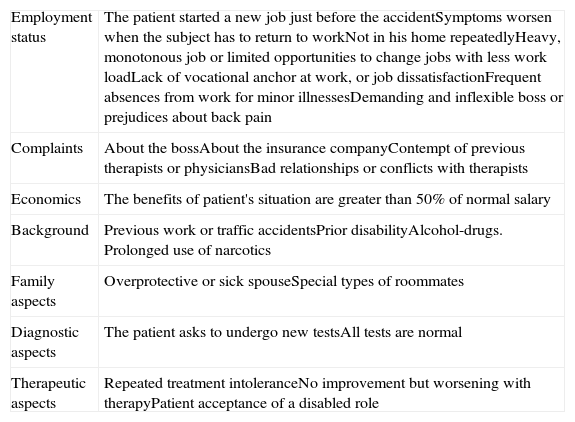
Clinical Signs of an Abnormal Response or Distorted Style/unreliable Response Style1. “Yellow and Red Flags”They are obtained from the history and deal with certain occupational variables that can be seen summarized in Table 1.8–10 They have been cited in the literature as “yellow” or “red flags” of simulation.
Signs of Suspicion. Yellow and Red Flags.
| Employment status | The patient started a new job just before the accidentSymptoms worsen when the subject has to return to workNot in his home repeatedlyHeavy, monotonous job or limited opportunities to change jobs with less work loadLack of vocational anchor at work, or job dissatisfactionFrequent absences from work for minor illnessesDemanding and inflexible boss or prejudices about back pain |
| Complaints | About the bossAbout the insurance companyContempt of previous therapists or physiciansBad relationships or conflicts with therapists |
| Economics | The benefits of patient's situation are greater than 50% of normal salary |
| Background | Previous work or traffic accidentsPrior disabilityAlcohol-drugs. Prolonged use of narcotics |
| Family aspects | Overprotective or sick spouseSpecial types of roommates |
| Diagnostic aspects | The patient asks to undergo new testsAll tests are normal |
| Therapeutic aspects | Repeated treatment intoleranceNo improvement but worsening with therapyPatient acceptance of a disabled role |
All are part of the so-called bio-psycho-social model.11,12 In it, the biological factors (lesions) interact with other psychological (e.g. misconceptions about the spine, fear of pain, fear of job loss),13,14 social and labor aspects (education, family factors, type of work, career, etc.).
2. Features of the Patient's CompanionOne characteristic of a style of distorted response is the need to highlight the sick role. Thus, the analysis of the patient's companions can be a key factor.
Frequently, they highlight the magnitude of the conditions (“enhancer”). Other times, the attitude is derogatory. Thus, the “liberated husband” of Rotes Querol15 tends to downplay or reinterpret the sufferings of the sick. Comments like “ignore him/her doctor,” “he/she is exaggerating” or “what he/she means is that it hurts there,” are common.
Other companions are “instructed or aware” and “coercive.” They boast an extensive knowledge of the disease or exhibit hostility or mistrust that appears to lead directly to the medical intervention, “Maybe something was wrong with the operation?”. In general, it is useful to explore the extent of knowledge about the disease showed by the companion. The concept of metasimulation regards monitoring by the subject of the guidelines or the script of a case similar to theirs and, not infrequently, the real patient is his or her companion.
Sometimes the patient appears “in need of support.” In this sense, it is not usually very reasonable for adult and autonomous patients to attend, visit after visit, constantly accompanied by their parents.
The presence in the clinic of an inordinate number of escorts can also be expressive of the desire or need for reinforcement company in the visit.
3. InconsistenciesThey are clinical manifestations lacking entity. Obtained through interrogation.
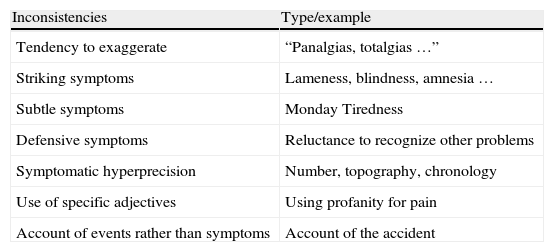
Examples are the following (Table 2):
SADR/NCRS/RS Markers.
| Inconsistencies | Type/example |
| Tendency to exaggerate | “Panalgias, totalgias …” |
| Striking symptoms | Lameness, blindness, amnesia … |
| Subtle symptoms | Monday Tiredness |
| Defensive symptoms | Reluctance to recognize other problems |
| Symptomatic hyperprecision | Number, topography, chronology |
| Use of specific adjectives | Using profanity for pain |
| Account of events rather than symptoms | Account of the accident |
| Inconsistencies | Type/example |
| Hysterical Romberg | Oscillating, strange |
| Cogwheel phenomenon | Disharmonic or hesitant movement |
| Inverted answers | Heat to cold, or vice versa |
| Phenomenon of abrupt relaxation | Not slow and harmonical as normally found |
| Exploration of resisted movement | Onset of pain |
| Hoover maneuver | Lack of pressure in healthy heel |
| Goldthwaite sign | Pain just putting the hand under the lumbar region |
| Mankopf test | Increase of 5% or more of heart rate by palpating the painful area |
| Discrepancies | Example |
| Clinical-interrogation | Collarette with tan underneath |
| Clinical and exploratory | Loss of strength, but increased resistance to passive movementIndirect mobility (looking at a wristwatch, estimating the height of the room, etc.)Orthesis with no stains or wear. No marks, dermatitis or evidence of supportDifferent results between the forms of the Lasègue maneuver |
| Clinical behavioral | Follow up of behavior |
| Discrepancies of causality | Adequately investigating the accident |
| Contradictions | Example |
| In the same visit | Documentation of examinations |
| On different visits | Test of body drawing |
3.1 A tendency to exaggeration. It can affect any aspect of the symptoms: number, intensity, quality, magnitude, etc. Total pain (“panalgia” or “totalgia”) is inconsistent.
3.2 Flashy symptoms.6 Constituted by those who a lay person would consider typical of the disease or disability. Examples: lameness, motor weakness, anesthesia of a region, loss of vision or hearing. These symptoms are greatly increased in frequency in the SADR.
3.3 Subtle symptoms.6 Constituted by those that are considered common or ‘normal’ in life (getting tired on Monday, ending the day tired, dulling headache in closed spaces or dizziness in a vehicle). Are more numerous and they come to the foreground in SADR.
3.4 Defensive symptoms. The patient denies symptoms of having symptoms in the past that are common in the population (sore throat, headache, morning fatigue, stomach pain, etc.). For example, in more than one case, there is a marked reluctance to acknowledge any problems before the accident.
3.5 Symptomatic hyperprecision and detail. For example, pain that began on a certain day and at a certain hour and reappear in a fixed interval, or at the same time. Writing down all diseases (“Maladie des petits papiers” Rotes Querol).15 In this same line we find the contribution, sometimes obsessively, of all kinds of tests or reports made before the current visit.
3.6 Use of specific adjectives. In SADR, the patient uses a particular language.16 Expressions as follow abound: “as if” (“It's as if I was wounded inside”). The use of profanity to refer to pain is also very typical.
3.7 Account of events rather than symptoms. Patients with SADR like to recreate or recount the events (accident, medical visits, fighting with insurers, etc.) more than the condition that was the reason for the visit.
4. InconsistenciesThese are impossible physical signs. They appear under examination. Some examples are listed in Table 2. The most relevant are mentioned below.
4.1 Reversed answers. When exploring thermal sensitivity, the patient says cold instead of hot, and vice versa. Clearly, this sign indicates NCRS or RS.
4.2 Exploration of resisted movement.7 Patient who believes that resisted movement must be painful, when in fact, this is unusual. Patients with RS or NCRS will tell us that spinal pain on resisted flexion–extension increases significantly. Normally, the point of fatigue is achieved gradually and is seen as the resistance gradually weakens. In SADR, the extremity relaxes abruptly (phenomenon of abrupt relaxation), sometimes with a snort at the end of the scan. Resisted movement can also be seen as disharmonic or faltering, with a touch reminiscent of a gear, as the patient acts voluntarily contracting and relaxing agonists and antagonists, indicating NCRS or RS.
4.3 Hoover maneuver.17 Performed with the patient supine and the heels out of the plane of the table, with the examiners hand on the healthy heel. The patient is asked to elevate the affected leg. If easily done, the test is considered negative. If the movement is difficult, the patient with no pathology will push the other leg against the examiners hand. Otherwise, it is an inconsistency. Similar maneuvers have been described, such as the abductor sign.18
4.4 McBride test.19 The patient is asked to hold on one leg while bending the other on the chest. As the knee is bent, no sciatic stretching occurs. In addition, the maneuver slightly flexes the spine, so facet pressure is relieved. Thus, this position should decrease back pain. An increase in pain is an incongruity.
4.5 Goldthwait sign.19 With the patient supine, a hand is placed under the lumbar spine and the examiner raises the lower extremity with the other. If there is pain before moving the lumbar region (perceived by the hand), this indicates sacroiliac involvement. If it appears later, then it indicates pathology of the L5-S1 joint.
4.6 Mankopf test.19 Palpation of the painful area should increase the heart rate by 5% or more. If this response does not occur (Mankopf positive), it would be incongruous.
4.7 Other incongruities. They are Lasègue positivity with maneuvering of less than 10°; lumbosciatic onset of pain, rather than crural pain in the reverse Lasègue, etc.
5. DiscrepanciesThese can be defined as the lack of agreement between 2 or more different elements of the clinical history. Discrepancies point more to a NCRS or RS than a SADR. There are different types (Table 2):
5.1 Clinical-interrogation. A permanent collarette does not allow a tanned neck. If it exists, this would be a discrepancy. Another example is patients who report disabling pains but live alone and unaided.
5.2 Clinical and exploratory. There are differences between the symptoms and examination (clinical or complementary).1 The patient reports loss of strength and yet the examiner appreciates increased passive resistance. The patient holds antigravity attitudes if the examiner suddenly drops the patient's hand and leaves the extremity in the air. The patient complains of decreased cervical mobility, but flexes the neck to look at his watch, or makes a perfect cervical extension if asked to calculate the height of the room. The patient complains of lack of movement of the limb for weeks, but no atrophy is evident. Hand calluses usually go away after 3 weeks of inactivity. Their presence in a “fixed” extremity may be another discrepancy. If a collarette (or other orthotics) is worn it shows signs of wearing, stains or tarnish, this should be considered a discrepancy. Using canes should produce callused hands. A person with cervical or lumbar disk herniations (and no motor deficit) appearing in a wheelchair is a discrepancy. The chair-bound patient usually gains weight and, in the areas of contact, develops dermatitis, signs of chafing, eczema and skin discoloration.
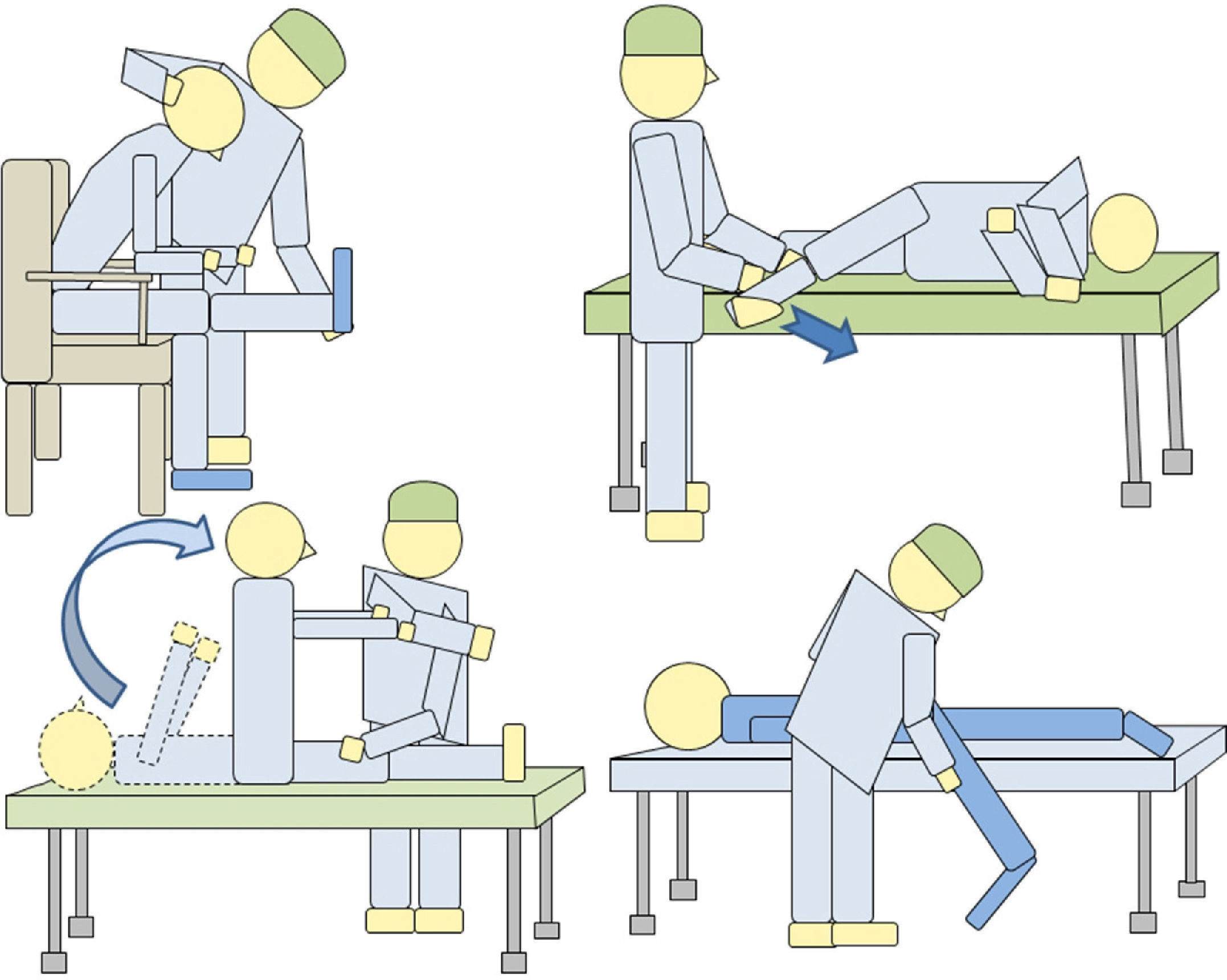
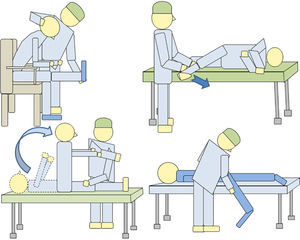
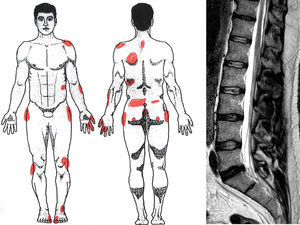
Nerve stretching maneuvers are used to detect inconsistencies. Thus Lasègue maneuver can be performed in various ways (Fig. 1) and can be assessed for discrepancies between them. If the patient has a positive Lasègue sign, for example at 30°, and feels no pain when performing the indirect Lasègue maneuver, the examiner is faced with a discrepancy.
Another way is to ask the prone patient to relax the painful extremity, dropping by the side of the examiners bed to the floor (Barraquer-Ferré sign). Lasègue maneuver on the patients’ side is also helpful. Neri I and II maneuvers, stretching neural roots in different positions, allow the examiner to detect discrepancies.
The Bench test involves the patient kneeling on a low stool (20cm in height approximately) and told to lean forward to touch the ground. This can usually be made without low back pain because it only involves the hip joint. The test is considered positive when the patient says it cannot be performed because of back pain.19
Lower back pain upon rotation of the hip in both supine and prone positions can also be considered a discrepancy.
If it is seen that passive range of joint mobility is greater than active, the clinician could be facing a discrepancy (O’Donoghue maneuver).19
5.3 Clinical-behavioral. Between symptoms and behavior. These must be documented. Detective investigation is of widespread use as of lately and could document a discrepancy, although it is not clear as to it proving the existence of SADR or RS, although it is associated with RS.
5.4 Discrepancies regarding causality. Between the traumatic event and clinical outcome (lack of proportionality between cause and effect).
6. ContradictionsOpposition between verbal, graphic, documentary or other related disease productions.
May occur in a single visit or on successive visits or interviews. In SADR it is usual to find difficulty in maintaining the constant subterfuge. Many times, the version that was previously mentioned is not remembered. Therefore, it is necessary to document the manifestations and physical findings. It is also recommended to increase the frequency of visits.
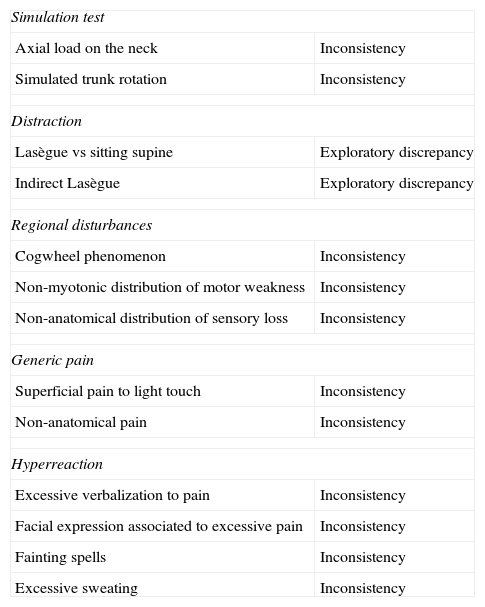
7. Waddell SignsIn 1980, Waddell et al.,20 reported 8 signs that, according to the authors, identified LBP patients with no structural problems. In our opinion, the Waddell signs are actually inconsistencies, incongruities or discrepancies, as can be seen in Table 3.
Signs of Waddell and Their Equivalence in Our System.
| Simulation test | |
| Axial load on the neck | Inconsistency |
| Simulated trunk rotation | Inconsistency |
| Distraction | |
| Lasègue vs sitting supine | Exploratory discrepancy |
| Indirect Lasègue | Exploratory discrepancy |
| Regional disturbances | |
| Cogwheel phenomenon | Inconsistency |
| Non-myotonic distribution of motor weakness | Inconsistency |
| Non-anatomical distribution of sensory loss | Inconsistency |
| Generic pain | |
| Superficial pain to light touch | Inconsistency |
| Non-anatomical pain | Inconsistency |
| Hyperreaction | |
| Excessive verbalization to pain | Inconsistency |
| Facial expression associated to excessive pain | Inconsistency |
| Fainting spells | Inconsistency |
| Excessive sweating | Inconsistency |
Additional tests provide information that can also be adapted to the proposed terminology. Here are some examples.
1. Definitions and Interpretation Imaging TechniquesThese allow for the detection of discrepancies. Thus, for a lumbar disk herniation on an MRI that does not correspond to the clinical evidence, there would be a clinical-radiologic discrepancy.21,22
2. Functional Biomechanical SystemsIts foundations are different. Some are based on the analysis of variability in23 successive scans. Thus, in patients with NCRS/RS it is difficult to accurately reproduce the symptoms in the same way or in the same range of motion.
In the biomechanics laboratory of our hospital, the functional study of spinal pathology is performed using the following tests:
2.1 Dynamometry: It is designed to measure the range of motion of the cervical spine and the maximum isometric force in flexion-extension and lateral-flexion at 0°, 25° and 45° rotation. A normal finding when there are normal strength values (compared to a normality database), a flexor-extensor ratio between 1/1 and 5-1/2, more force in neutral position than at 25° rotation and when the coefficients of variation are all under 15°.
2.2 It can detect discrepancies between strength and mobility in the cervical physical examination, obtained with the dynamometer and range of motion in the laboratory. One can also find contradictions, if repeat testing is performed on 2 different days and got different results.
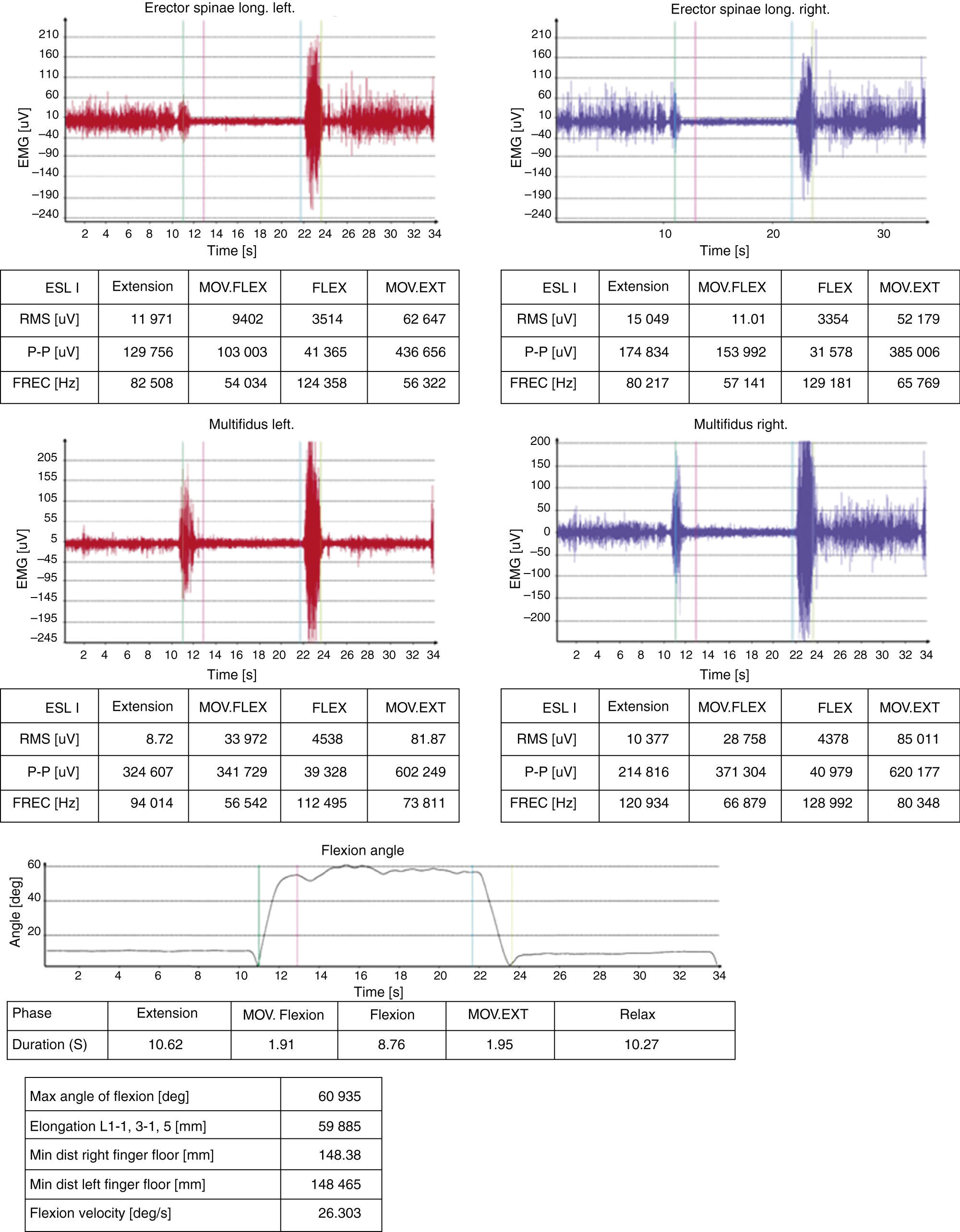
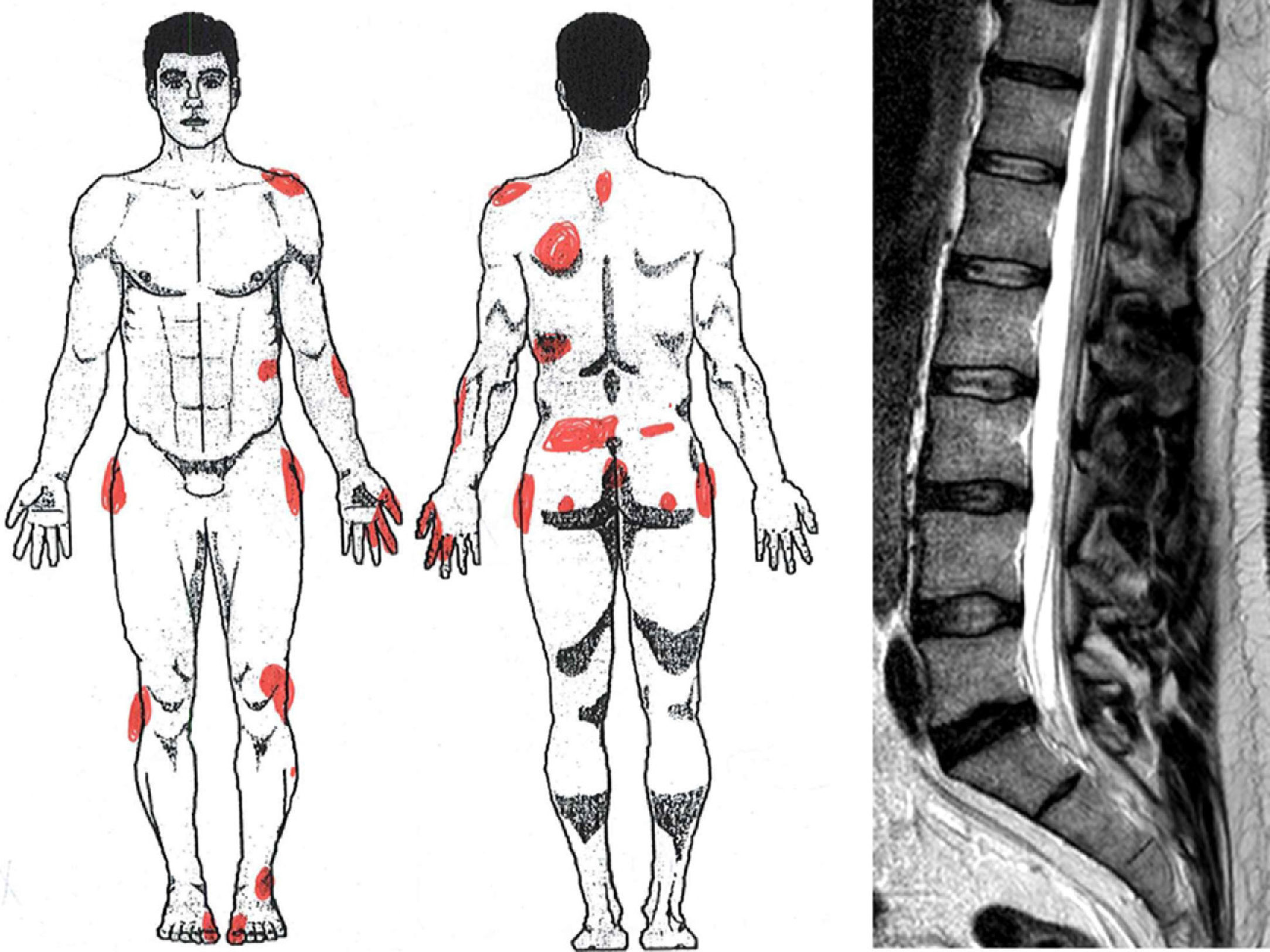
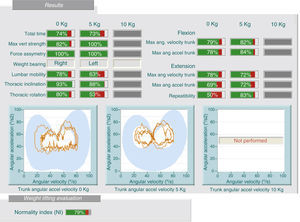
2.3 Kinetic studies (study of forces): These tests analyze kinetic and kinematic motion of the lumbar spine in simple activities. It provides data on lumbar mobility and forces by the person being tested under certain movements and mobilizing various loads. We can detect discrepancies between history and test results, for example, the patient refers limitation related to mobilizing loads and back pain when performing the test, handling loads of 5kg better than 0kg (Fig. 2). Likewise, we can find contradictions when retested on 2 different days and find different results.
2.4 Kinematic studies (analysis of velocity and angular acceleration): These tests can detect discrepancies between the physical examination, medical history and test results, for example, the patient cannot flex his lumbar spine over 30° during the physical examination and yet, can do a complete bend to pick up a box off the floor (Fig. 3).
In this case, the patient performs, on the weight test (same patient as in Fig. 2), a lumbar flexion of 78% and 63% in the seat test (image). There is a lack of consistency in the assessment because very different results are obtained for the same variables (discrepancy).
It has been noted that the normality of motor evoked and/or somato-sensory potentials points toward a conversion syndrome.24–28
It would occur here as with the other examinations. On the one side, the neurophysiologic indemnity can express a discrepancy in a patient who refers important symptoms.
Also, demonstrating neurophysiological chronicity clues the observer into a problem with a history that the patient may deny (through a defensive inconsistency, clinical-exploratory discrepancy).
Some techniques seem more specific of NCRS or RS, such as surface electromyography.29 In our hospital, we use it for the study of the lumbar spine, through the lumbar flexion-relaxation phenomenon. It guides us to a discrepancy if the patient complains of back pain and the flexion-relaxation phenomenon occurs, since this is related to the absence of LBP (Fig. 4).
4. Psychological TestAn interesting aspect of simulation is pain. In a review of the literature, one can find at least 22 different pain scales.30 They can be classified into 3 types: pain intensity, other aspects of pain and mixed scales that measure two items (intensity and affective components).
Among the former we find the visual analog scale31 or other numbered scores.32 They intend to gauge the intensity of pain and may be useful in demonstrating inconsistencies between different visits, inconsistencies (exaggeration) or discrepancies (very severe pain, normality tests, conduct, etc.).
Among the latter, there are those that measured the affective component of pain.33,34 Some tests are more specific for back pain.35 Others have turned to simulation in general pain.36–40 Others study somatization in chronic low back pain.41 To detect the possibility that a patient with chronic back pain may return to work, Kool et al.42 advocate employing 4 scores. Other tests measure different work, social and family variables, such as “mass psychogenic illness”.43 Finally, there are psychogenic test simulations, most notably the Minnesota Multiphasic Personality Inventory.44,45 Its role in low back pain has been noted.46 The Wechsler Adult Intelligence Scale has been used to build the so-called Simulation index.47 Using this test, some authors have shown the presence of cognitive impairments they attribute, in the absence of brain damage, to a manifestation of exaggeration.48 Projective tests (such as Rorschach)49 may also be used, geared more toward mental illness50,51 as well as others aimed at the detection of simulating physical disability, such as the Composite Index of Simulation of Disability.52
We have found utility in tests that include body drawing.39,53 Thus, the graphical representation of pain and its nuances can be used to check inconsistencies (exaggeration, neatness, hyperprecision), contradictions (between different drawings) or incongruences (non-metameric distribution of pain) (Fig. 5).
There are tests to detect a low deliberate effort (“faking bad”), as in the so-called forced-choice tests.54-57 It has been said that they allow the examiner to prove untruthfulness in multiple neurological signs such as: touch hypoesthesia, graphesthesia, blindness, deafness and other functions.
DiscussionImportance of TerminologyThe advantages of introducing the terminology that we propose (SADR, NCRS, RS) are several. First, the term SADR in medical records or reports does not characterize the patient directly as a simulator. It simply finds that an inappropriate response style is appreciated. At the same time, this terminology avoids the disparaging epithets that may result (simulation, exaggeration, profiteering, etc.).
A patient with SADR or NCRS can respond to different models. It may be a normal patient facing adverse situations (adaptive model). There may be other causes, sometimes psychological, distorting the response. It can also occur that it is an RS but without objectifying, by far, the criteria required by the ICD for diagnosis.
We suggest that the clinician should try to find out which model is most likely, since it is rarely possible to intervene therapeutically to redirect the response to normal or to harness the diagnosis of RS.
So, initially, we recommend talking about SADR, reserving NCRS for suspected fraudulent cases, but where the intention of gain is unsubstantiated. NCRS does not qualify the subject as a simulator. It simply refers to the style of response as vague or inaccurate, which subtracts verisimilitude. It would be a degree beyond SADR, but without the burden of meaning it found the fraud required in real simulation.
When the case has medico-legal implications, terminology and the guidelines proposed in this paper facilitate reporting and contributing to the lawyer a proper interpretation of biomedical variables.
Clinical VariablesMost studies indicate that “simulation” should be suspected in 3 circumstances: when there are tangible incentives, when symptoms do not match the examination or when there is no organic basis for them.12,13 Indeed, the existence of a tangible incentive is a ‘red flag’, and both clinical and exploratory discordance, such as the absence of an organic base, are discrepancies.
We argue that these factors and others described in the literature are merely markers for SADR/NCRS/RS and can be classified using terminology proposed in this paper.
The same can be said of Waddells’ sign. It has been noted that, in fact, these signs seem derived from fear in the context of recovery from trauma or the development of a chronic disability, offering only an element of suspicion and not a lie.58 Recently, it has been reported that there is little evidence to even establish a relationship between these signs and secondary gain or simulation. Rather, the evidence points to the contrary, no association.51 In our opinion, all of them can be assimilated to any of the categories proposed here, i.e. inconsistencies, incongruity or discrepancies.
Regarding the value of the proposed semiological elements, some of them deserve special attention. For example, causes for discrepancies are often difficult to discover because the examination is not consistent with imaging. This requires very rigorous screening of structural causes for the patient's complaints. It requires, therefore, specialized assessment before declaring the existence of a clinical-radiologic discrepancy.
As noted above, the clinical examination is essential, but we must know how to evoke non-reliable responses. Perhaps, therefore, when suspecting SADR, examination should be amended to elicit possible inconsistencies or discrepancies. Thus, it is useful to converse with the patient about something unconnected with his illness like while examining, starting the physical examination provided on the unaffected parts, finishing the exploration in antigravity positions, observing the appearance of hesitation, and repeating the examination in different positions.
Additional TestsThe instrumental58 systems described are very useful to discover and document inconsistencies, discrepancies and contradictions. These last 2 characterize the NCRS and RS, so that, objectively, are of remarkable value in detecting those problems. Therefore, rather than use them as proof of simulation, we believe that the results have to adapt to the terminology proposed, so that they objectify the inconsistencies, contradictions or discrepancies if they exist, and these can be placed in a common context with the rest of the signs detected in the history and examination. It would be the only way to standardize the results and know the real value of these tests in the context of RS detection.
This approach is extended to59 biomechanical testing, which should be placed in a multidimensional exploratory clinical context. In our opinion, the results of these examinations could also adapt to the terminology proposed by offering a demonstration stage of the real situation of the patient.
As with the rest, they are still tests that reveal discrepancies between what should be obtained in a normal situation and that of the patient. Sometimes, they can show impossible signs, which would demonstrate inconsistencies. In any case, it has been reported that one must be very cautious with the interpretation of many isolated tests because, on a case-by-case basis, they may show doubtful efficacy.60 Therefore, it is essential to relate these results to the rest of the clinical exploratory semiology commented. In a practical sense, a patient may accumulate inconsistencies, incongruities, discrepancies and contradictions in both the history, and the clinical examination as well as in complementary tests. From the study of these signs the type of response model assimilated by each case can be deduced.
The Multidimensional ApproachUltimately, the detection model proposed by us is a multidimensional system. A patient with a distorted response style accumulates many elements from different axis, both clinical and exploratory, which must be identified and standardized for ease of interpretation.
The adoption of a uniform terminology for coding and interpretation of clinical and exploratory results of the spine provide a basis for future studies supported by a standardized common semiology.
In our opinion, this multidimensional terminology and unification model is useful for identifying an abnormal profile and response style in each patient, and assess whether the profile is bona fide or not, and in the latter case, as in a true simulation. It also allows to appropriately intervene in the biological, psychological and social aspects of it, avoiding iatrogenic distress.
At present, we do not have any system capable of completely denying the existence of pain. Nor do we know the complex mechanisms by which a chronic widespread pain may follow trauma. However, a multidimensional approach to the case, supported by the semiology we propose, may be the best way to approach the thorny issue of simulation.
Semiology and terminology proposals have been modeled on the example of spinal pathology, but are extendable to other skeletal manifestations in suspected simulation or similar cases.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that this research did not perform experiments on humans or animals.
Data privacyThe authors state that patient data does not appear in this article.
Right to privacy and informed consentThe authors state that patient data does not appear in this article.
Conflict of InterestThe authors declare no conflict of interest.
Please cite this article as: Aso Escario J, Martínez Quiñones JV, Aso Vizán A, Arregui Calvo R, Bernal Lafuente M, Alcázar Crevillén A. Simulación en patología espinal. Reumatol Clin. 2014;10:396–405.