As biphosphonates (BP) are powerful inhibitors of osteoclasts, producing a marked reduction in bone reabsorption, they have been attributed with anti-tumoral properties such as contention of tumour cell invasion, inhibition of adhesion of tumour cells to bone tissue, induction of apoptosis in several malignant cell lines and inhibition of proteolytic activity of matrix matelloproteinases.
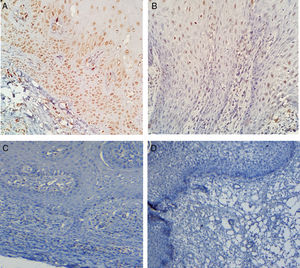
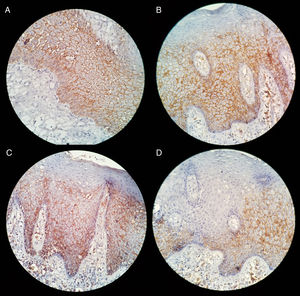
Our group conducted a study which was focused on evaluating intercellular apoptosis and adhesion in oral mucosa keratinocytes associated with osteonecrosis induced by BP. To do this, the expression of Bax, Bcl-2, survivin and syndecan-1(CD138) proteins were studied using immunohistochemistry through indirect staining of capillaries in 10 oral mucosa samples contiguous to BP-associated osteonecrosis. The expression of each marker was assessed using positive cell percentage. Data obtained were analysed with descriptive statistics. Results showed epithelial expression of the pro-apoptotic marker Bax in 100% of the samples, whilst the anti-apoptotic Bcl-2 and survivin markers expressed negatively in all the epithelia studied (Fig. 1). Interestingly, the expression of syndecan-1 was observed as reduced in basal and superficial strata of the lining epithelium (Fig. 2).
Immunohistochemical apoptosis profile of oral mucosa in patients with osteonecrosis induced by BP. (A) Microphotographs (40×) showing nuclear expression of Bax in epithelium, mainly in the basal and parabasal layer. (B) Microphotographs (40×) showing nuclear expression of Bax in spiny epithelium strata. (C and D) Absence of the expression of Bcl-2 (C) and survivin (D) in oral mucosa epithelium.
Recent investigations have focused on the search for the possible existing relationship between alterations produced by the use of BP in the soft tissue of the oral cavity and its relevance in osteonecrosis of the jaw.1–4 Based on this, the study which we carried out showed the changes in the functions of the oral keratinocytes of the mucosa which coats the BP-induced osteonecrosis, as apoptosis and cellular adhesion.
Apoptosis plays an important role in the regeneration of healthy cells and elimination of damaged cells. A de-regulated apoptosis induces tissue damage, which leads to organ failure. The results of this study show obvious activation of oral mucosa keratinocyte apoptosis contiguous to the necrotic bone induced by BP action. Increased apoptosis has also been described in oral fibroblasts compromised by BP.1–4 It has been suggested that the changes in apoptosis in the fibroblasts and the induction of senescence in the keratinocytes impede proliferation and cellular migration, two processes which are important for re-epithelisation of oral mucosa.1
Saracino et al.5 demonstrated the in vitro effect of keratinocytes on osteoblasts when they were jointly exposed to BP. The formation of pro-inflammatory cytokines of the keratinocytes could reduce the proliferation and osteogenic properties of the osteoblast, stimulating greater capacity to induce osteoclastic differentiation.6 This affirmation suggests that the change in proliferation and cellular migration in the soft tissue from the use of BP intervenes as an active step of osteonecrosis of the jaw.5–9
With regard to cellular adhesion, few studies have been conducted on the action of BP in the cell-to-cell adhesion process. The loss of expression of syndecan-1 in the epithelial area observed in this study is interesting, and this may be attributed to a direct consequence of the effect of chemical inflammation markers.
With the use of electronic microscopy, Donetti et al.10 observed a thinning down of the desmosomes in the upper layers of the oral epithelium showing that epithelial adhesion is affected by the therapeutic dose of alendronate in human oral mucosa. The reason why the adhesion between keratinocytes is affected is merely speculative and further in-depth study is required regarding this complex process.
The results of this study show the induction of an apoptosis process in oral keratinocytes induced by BP action, which could constitute the starting point of the bone exposure process in antiresorptive drug-related osteonecrosis of the jaw. Furthermore, this is the first time an alteration of the intercellular adhesion in the epithelium which covers the bone affected by BP has been described, and this could constitute the bone exposure pathway, as a product of the epithelial disruption.
Please cite this article as: Villarroel-Dorrego M, Romero ME, Reyes O, Pereira-Prado V, Bologna-Molina R. Estudio de apoptosis y adhesión intercelular en mucosa oral de pacientes con osteonecrosis inducida por bifosfonatos. Reumatología Clín. 2019;15:e75–e77.