Sweet's syndrome or acute neutrophilic febrile dermatosis is a systemic disease of unknown etiology characterized by the appearance of skin lesions produced by a neutrophilic dermal infiltrate, fever, and peripheral leukocytosis. It may be associated with hematologic diseases, including leukemia, with immune diseases as rheumatoid arthritis, or can occur in isolation. The myelodysplasias are hematological disorders characterized by one or more cytopenias secondary to bone marrow dysfunction. We present the case of a patient with Sweet's syndrome associated with myelodysplastic syndrome and treated with glucocorticoids who did not present a good clinical outcome. We discuss the different treatment of these diseases because in most cases glucocorticoids, which are the treatment of choice in Sweet's syndrome, may be insufficient.
El síndrome de Sweet o dermatosis neutrofílica febril aguda es una enfermedad sistémica de etiología desconocida, caracterizada por la aparición de lesiones cutáneas producidas por un infiltrado dérmico neutrofílico, fiebre y leucocitosis periférica. Puede estar asociado a enfermedades hematológicas, incluida la leucemia, inmunológicas como la artritis reumatoide o presentarse de forma aislada. Las mielodisplasias son trastornos hematológicos caracterizados por una o más citopenias secundarias a la disfunción de la médula ósea. Se presenta el caso de un paciente con síndrome de Sweet asociado a un síndrome mielodisplásico que ha seguido tratamiento con glucocorticoides y no ha presentado una buena evolución clínica. Se discuten los diferentes tratamientos de estas enfermedades porque en la mayoría de las ocasiones los glucocorticoides, que son el tratamiento de elección en el síndrome de Sweet, pueden ser insuficientes.
Sweet's syndrome (SS) is a skin disease of unknown etiology1,2 which is characterized by fever, leukocytosis, and painful erythematous skin plaques. Histology shows dense neutrophilic infiltrates. The presence of anemia and thrombocytopenia may be associated with an underlying neoplastic.3
We present the case of a patient with SS and anemia diagnosed as a myelodysplastic syndrome (MDS), worsening the prognosis.
MDS are hematologic diseases characterized by cytopenias that result in dysmorphic states of the cells of the bone marrow. One type of MDS is refractory anemia with blast excess (RABE), with the number of blasts being greater than 5% and less than 10% in type 1, and between 10% and 20% in type 2. These diseases are refractory to chemotherapy and stem cell transplant offers a cure. In RABE, supportive treatment is performed with red blood cell transfusions.
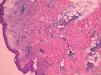
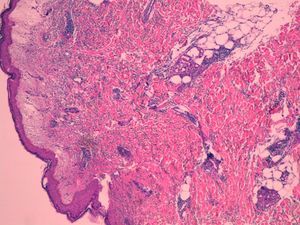
Case ReportThe patient is a 70 years old male with no history of interest, who had recurrent episodes of 2 weeks with high fever, leukocytosis, and erythematous papules and plaques on the extremities, with dense neutrophilic infiltrates in the biopsy (Fig. 1). The patient had asymmetric oligoarthritis affecting the wrist and knees. Analytically, there was an elevated sedimentation rate (ESR), leukocytosis, and anemia. Episodes were treated with glucocorticoids at 0.5mg/kg, with little response. The disease became chronic and recurrent. Indomethacin was prescribed a dose of 150mg/day and potassium iodide was added, without improvement. In parallel, the patient was diagnosed with a type 1 RABE after the study of persistent anemia. We performed multiple red blood cells transfusions.
Patient outcome was not favorable, with persisting episodes of fever, and arthritis. His anemia worsened and underwent a bone marrow transplant. While waiting for a compatible donor, the patient died, possibly due to a complication of the hematologic process, worsening of cytopenias or transformation to leukemia.
DiscussionSS can be classified into 3 groups: idiopathic, associated with malignant disease and drug-induced. Up to 54% of patients may have a tumor or hematologic disease.4 Joint involvement may occur (33%–62%), as well as lung, eye, kidney, liver, or central nervous system compromise. Chronic recurrent disease occurs in around 15%.1 The disease is more common in women in the fifth decade of life. The ESR is elevated and anemia present. It can last from 1 week to 4 years. The differential diagnosis must be made with erythema nodosum, cellulitis and erysipelas, erythema elevatum diutinum, erythema multiforme, leukocytoclastic vasculitis, or pyoderma gangrenosum.
Systemic glucocorticoids are the treatment of choice. Indomethacin5 is effective. Colchicine, potassium iodide, dapsone, cyclosporine, interferon alpha or etretinate6 are therapeutic alternatives. There have been reports of SS and MDS successfully treated with intravenous immunoglobulin,7 glucocorticoids, and doxycycline or stem cell transplantation.8,9
The patient described had a case that progressed despite treatment. Pending the transplantation we were able to use some of the treatments described in the literature, although possibly the transplant would had been the only effective treatment.
ConclusionSS is a rare dermatological entity, which when accompanied by an MDS may worsen the patient's prognosis. The treatment of choice for SS is the use of glucocorticoids, although in most cases this may be insufficient and require alternative therapies.
Ethical disclosuresProtection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of Data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors must have obtained the informed consent of the patients and /or subjects mentioned in the article. The author for correspondence must be in possession of this document.
DisclosureThe authors have no disclosures to make.
Please cite this article as: Reina D, et al. Síndrome de Sweet asociado a síndrome mielodisplásico: a propósito de un caso. Revisión de la literatura. Reumatol Clin. 2013;9:246–7.