Inhibitors of tumor necrosis factor-alpha (anti-TNF-alpha) are widely used in different medical specialties. The main adverse effect of these agents is the increased risk of infection. We report the case of a 30-year-old man with ankylosing spondylitis who had begun receiving golimumab two weeks earlier. He presented with a 10-day history of salmon-colored lesions on trunk, palms and soles. The clinical suspicion was secondary syphilis. Treponemal and nontreponemal tests confirmed the diagnosis of syphilis. Lumbar puncture was also performed, although there was no neurological involvement, to rule out neurosyphilis. Cases of syphilis in patients in treatment with TNF-alpha inhibitors are uncommon in the literature and there are no established protocols.
Los fármacos inhibidores del factor de necrosis tumoral alfa (anti-TNF alfa) son ampliamente utilizados en diversas especialidades médicas. El principal efecto adverso de estos fármacos es el aumento del riesgo de infecciones. Presentamos el caso de un varón de 30 años con espondilitis anquilosante, en tratamiento desde hacía 2 semanas con golimumab, que consulta por lesiones asalmonadas en tronco, palmas y plantas de 10 días de evolución. Con la sospecha de un secundarismo luético se solicitaron pruebas treponémicas y no treponémicas que confirmaron el diagnóstico. Asimismo se solicitó una punción lumbar, aunque no existía sintomatología neurológica, para descartar neurosífilis. Los casos de sífilis en pacientes en tratamiento con anti-TNF alfa son excepcionales en la literatura y no hay protocolos establecidos que nos guíen sobre cómo actuar ante esta situación.
Syphilis is an infection known as the “great imposter” for the diversity of signs and symptoms it presents with. There has recently been an upsurge in its incidence and we must therefore be particularly alert to clinical situations, especially to special clinical situations. One example of this are patients being treated with anti-TNF alpha drugs. These drugs have many indications at present and a good safety profile, but we must remember that their main adverse effect is the increase in the risk of infections.
Clinical observationA Spanish male aged 30, with ankylosing spondylitis of 8 months duration, had been in treatment for 2 weeks with golimumab, and was referred to the dermatology department due to a 10-day history of salmon colored lesions on trunk, palms (Fig. 1) and soles of feet. He stated he had not taken any other drugs, except NSAIDS. He did not recall having had previous lesions on genital or oral mucosa before. During anamnesis he stated that he had had unprotected sexual relations. Due to suspicion of secondary syphilis we requested treponemal tests (FTA-ABS) and non treponemal tests (VDRL and RPR), which tested positive. The serologies for HIV and hepatitis B and C viruses tested negative. Due to the diagnosis of syphilis of indeterminate duration the patient was treated with intramuscular benzathine G penicillin, 2.4 million units, in a total of 3 separate doses for one week. Neurological examination was normal, but since the patient had been previously treated with an anti-TNF alpha agent we decided to perform lumbar puncture, requesting the PRP test, cellularity and biochemistry in cerebrospinal fluid, which resulted non pathological. Other sexually transmitted diseases were tested for, resulting in the polimerase chain reaction (PCR) as positive for Neisseria gonorrhoeae in the pharynx and the patient therefore received treatment with 250mg ceftriaxone by intramuscular route and 1g of oral azitromicin in a single dose. The patient is currently undergoing periodic clinical and serological controls, and evolution has been favourable.
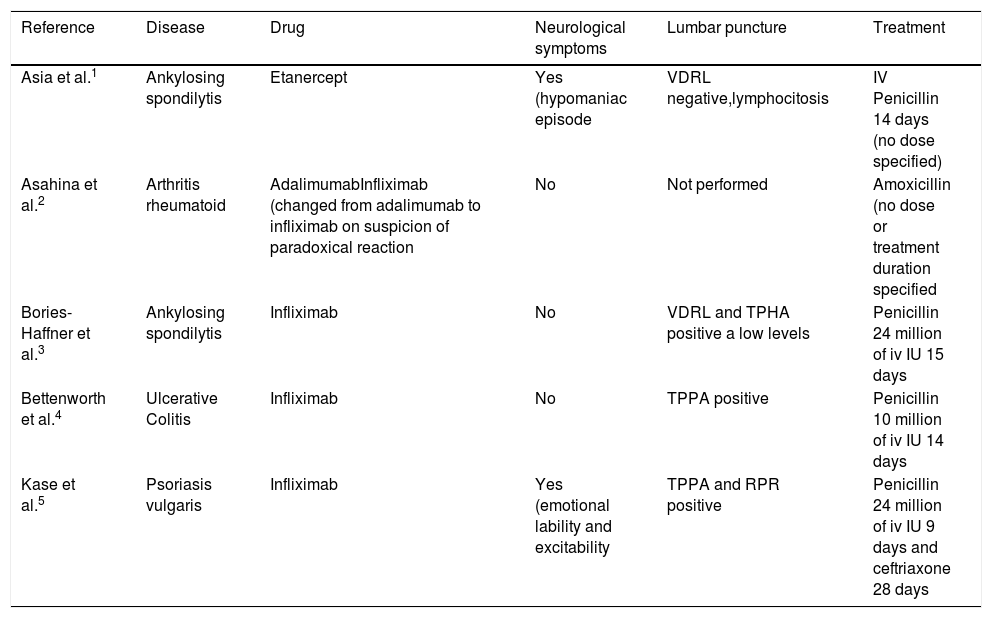
DiscussionGolimumab is a recombinant human IgG1 monoclonal antibody, the mechanism of action of which consists of blocking TNF alpha. It is used in several rheumatological diseases, including rheumatoid arthritis, ankylosing spondylitis or psoriatic arthritis. As with the other anti-TNF alpha drugs, there is a well-established protocol of testing for infections and comorbidities before and during treatment. However, cases of syphilis in patients in treatment with anti-TNF alpha are rare in the literature, and there are therefore no established protocols to follow in this exceptional circumstance. Of the 5 cases described in the literature (Table 1), 2 had neurological symptoms, including emotional lability and excitability and 4 had a pathological lumbar puncture (VDRL positive or raised cellularity). In our case, despite the absence of neurological dysfunction symptoms we reached a multidisciplinary consensus to perform lumbar puncture to rule out subclinical neurological involvement, observed more commonly in immunodepressive patients. The majority of cases described were in treatment with infliximab. This is the first case of syphilis described in the literature in the context of treatment with golimumab.
Cases of syphilis in the context of treatment with anti-TNF alpha agents described in the literature.
| Reference | Disease | Drug | Neurological symptoms | Lumbar puncture | Treatment |
|---|---|---|---|---|---|
| Asia et al.1 | Ankylosing spondilytis | Etanercept | Yes (hypomaniac episode | VDRL negative,lymphocitosis | IV Penicillin 14 days (no dose specified) |
| Asahina et al.2 | Arthritis rheumatoid | AdalimumabInfliximab (changed from adalimumab to infliximab on suspicion of paradoxical reaction | No | Not performed | Amoxicillin (no dose or treatment duration specified |
| Bories-Haffner et al.3 | Ankylosing spondilytis | Infliximab | No | VDRL and TPHA positive a low levels | Penicillin 24 million of iv IU 15 days |
| Bettenworth et al.4 | Ulcerative Colitis | Infliximab | No | TPPA positive | Penicillin 10 million of iv IU 14 days |
| Kase et al.5 | Psoriasis vulgaris | Infliximab | Yes (emotional lability and excitability | TPPA and RPR positive | Penicillin 24 million of iv IU 9 days and ceftriaxone 28 days |
iv: intravenous; IU: international units.
Accurate diagnosis and treatment of syphilis is essential to avoid contagion and sequelae. If patients are going to receive treatment with anti-TNF alpha agents this entity should be taken into consideration and an anamnesis should be undertaken to assess factors such as unprotected sex and the number of sexual partners. Periodical skin examination is required and if risk factors exist then luetic serological tests should be requested prior to initiation of biological treatment and regularly during treatment. There is currently no well-established diagnostic and therapeutic protocol for these patients.
Conflict of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Iglesias-Plaza A, Iglesias-Sancho M, Quintana-Codina M, García-Miguel J, Salleras-Redonnet M. Sífilis en el contexto de tratamiento con anti-TNF alfa. Reumatol Clin. 2019;15:e108–e110.