Cases of acute myocarditis have been after administration of the BNT162b2 and Ad26.COV2.S vaccine.
ObjectiveDescribe another possible mechanism of myocarditis after COVID-19 vaccination.
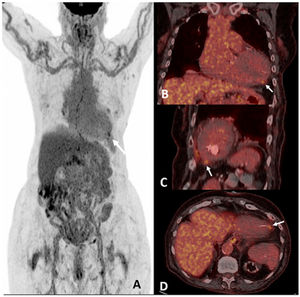
Case presentationWe describe the clinical case of a 72-year-old female with pleuritic chest pain one week after the third of the BNT162b2 mRNA vaccine. Serological tests for cardiotropic pathogens were negative, and autoimmunity screening was positive with anti-nuclear antibody (ANA) in 1:160 dilution, Anti-double-stranded DNA (anti-dsDNA), and anti-histone antibodies. 18F-fluoro-deoxy-glucose (FDG) positron emission tomography/computed tomography (PET/CT) showed a focal myocardial and pericardial inflammatory process in the cardiac apex.
Results and discussionSystemic lupus erythematosus (SLE) diagnosis was made with myocardial affection. As far as we know, this is the first report of a case of lupus myocarditis after the COVID-19 vaccine.
ConclusionGiven the pathogenic rationales, the association between SLE and myocarditis should be considered.
Se han presentado casos de miocarditis aguda tras la administración de las vacunas BNT162b2 y Ad26.COV2.S.
ObjetivoDescribir otro posible mecanismo de miocarditis posterior a la vacunación contra el COVID-19.
Presentación del casoDescribimos el caso clínico de una mujer de 72 años con dolor torácico pleurítico una semana después de la tercera vacuna de ARNm BNT162b2. Las pruebas serológicas para patógenos cardiotrópos fueron negativas y el cribado de autoinmunidad fue positivo con anticuerpos antinucleares (ANA) en dilución 1:160, anticuerpos anti-ADN de doble cadena (anti-dsADN) y antihistonas. La tomografía por emisión de positrones/tomografía computarizada (PET/TC) con 18F-fluorodesoxiglucosa (FDG) mostró un proceso inflamatorio miocárdico y pericárdico focal en el ápex cardíaco.
Resultados y discusiónSe realizó el diagnóstico de lupus eritematoso sistémico (LES) con afectación miocárdica. Hasta donde sabemos, este es el primer reporte de un caso de miocarditis lúpica después de la vacuna contra el COVID-19.
ConclusiónDadas las justificaciones patogénicas, se debe considerar la asociación entre lupus eritematoso sistémico (LES) y miocarditis.
After the emergency use authorization of the BNT162B2 messenger RNA (mRNA) vaccine (Pfizer-BioNTech) against coronavirus disease 2019 (COVID-19), several authors have reported an increase in myocarditis incidence after initiating the vaccination campaign. Recently, autoimmune phenomena after COVID-19 vaccination have been reported increasingly, such as new-onset SLE.1,2
Clinical observationA 72-year-old female underwent kidney transplantation in 2004 due to a chronic kidney failure secondary to membranoproliferative glomerulonephritis. Autoimmune diseases, neoplasms, and infections were ruled out as causes of glomerular injury. The patient has been in chronic hemodialysis since 2017 after renal graft dysfunction due to chronic rejection. She presented to the emergency room with pleuritic chest pain one week after vaccination with the third dose of BNT162b2 mRNA. Physical examination was unremarkable. Her blood tests showed: haemoglobin 12.4g/dl (12–16g/dl), total leucocyte count 4.86×10E9/L (4.8–10.8×10E9/L), total lymphocyte count 0.58×10E9/L (1.2–4.5×10E9/L), urea 91mg/dl (16.6–48.5mg/dl), troponin I 231.5ng/L (0–14ng/L) -peak value-, erythrocyte sedimentation rate 17mm/h (0–10mm/h), C-reactive protein 0.58mg/dl (≤0.5mg/dl). SARS-CoV-2 PCR test was negative. Serological tests for cardiotropic pathogens were negative. She had ANA IFA (indirect immunofluorescence assay) positive in 1:160 dilution, anti-dsDNA, and anti-histone antibodies were positive with low serum C3 level (75.50mg/dl, NV: 79–152mg/dl), normal C4 level (27.50mg/dl, NV: 16–38mg/dl) and normal CH50 level (537U/ml, NV: 392–1019U/ml). The patient denied alopecia, arthralgias/arthritis, skin lesions, vasculitis, or a family history of autoimmune diseases. Without significant findings, an electrocardiogram, chest X-ray, continuous electrocardiographic monitoring, echocardiogram, and invasive coronary angiogram were performed. FDG PET/CT was requested, showing a focal myocardial and pericardial inflammatory process in the cardiac apex (Fig. 1). Given the results, a diagnosis of SLE with myopericarditis was established based on the 2019 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) classification criteria.3 She was immediately started on oral prednisone (1mg/kg) and beta-blockers improving clinically. At the three-month follow-up visit, the patient was asymptomatic; blood test results showed a low C3 level (65.60mg/dl), normal C4 level (30.60mg/dl), normal CH50 level (900U/ml) and positive anti-dsDNA.
DiscussionAn increasing number of cases of myocarditis after mRNA COVID-19 vaccination have been reported. The mechanisms of myocarditis after COVID-19 mRNA- vaccination are still unclear. The immune system might detect the mRNA in the vaccine as an antigen, resulting in the activation of proinflammatory cascades and immunological pathways in the heart.4 Molecular mimicry between the spike protein of SARS- CoV-2 and cardiac self-antigens is another possible mechanism.4 Myocarditis associated with COVID-19 mRNA vaccination occurs within one week of viral antigen-induced immune activation.5
SLE is an autoimmune disease of unknown cause that can affect virtually any organ of the body and is associated with the production of autoantibodies (ANA, anti-dsDNA) against different autoantigens forming immune complexes. SLE results from the interaction of certain factors (genetics, hormonal, environmental) that may trigger an autoimmune response.6
Cases of SLE have been described in the literature after the COVID-19 vaccination.1,2 Among the related cases, one defines a 22-year- old-female with polyarthralgia and skin rash ten days after the second dose of the AZD1222 ChAdOX1 nCoV-19 vaccine. ANA immunoblot test showed positive for anti-dsDNA and anti-histones antibodies.7 Zavala et al. reported a 23-year-old woman who developed class V glomerulonephritis with low C3 levels, positive ANA, and anti-dsDNA antibodies one week after the first dose of the AZD1222 ChAdOX1 nCoV-19 vaccine.8 We present a case of a new-onset SLE with myopericarditis after COVID-19 vaccination. The cause-effect relationship between COVID-19 vaccines and SLE-myopericarditis is not fully understood. More studies are required to clarify the proposed mechanisms. The purpose of our publication is to award attention to this rare phenomenon. Fortunately, these events occur in a minority of patients, and the benefits of mass COVID-19 vaccination in morbidity and mortality outweigh the possible post-vaccine autoimmune syndromes.
ConclusionThis case reflects a possible mechanism of myocarditis triggered by vaccination that caused the onset of SLE in an immunologically predisposed individual.
FundingNone.
Conflicts of interestNone.
None.