Temporal arteritis is an uncommon disorder in young people. A 39-year-old woman with juvenile temporal arteritis is described and we performed a literature review of all cases of juvenile temporal arteritis described to date.
Case presentationA 39-year-old woman presented with a subcutaneous temporal nodule in the right temple with no other associated symptoms or background and unremarkable physical examination. Ultrasonography of the nodule revealed an anechoic perivascular halo surrounding the temporal artery. The nodule was excised resulting in the patient’s recovery. The results of the histopathological study showed features of juvenile temporal arteritis.
ConclusionsJuvenile temporal arteritis is a very uncommon disorder. Systemic manifestations should be ruled out by physical examination and complementary tests. Histopathology establishes the definitive diagnosis. Treatment is surgical excision and a follow-up should be conducted to rule out complications.
La arteritis de la temporal es un proceso infrecuente en paciente jóvenes. Se presenta el caso de una paciente de 39 años con arteritis de la temporal con revisión de casos descritos hasta el momento.
Presentación del casoMujer de 39 años sin antecedentes de interés que consulta por un nódulo subcutáneo temporal derecho, sin otros síntomas ni hallazgos a la exploración. En las pruebas realizadas destacaba la presencia de signo del halo ecográfico alrededor de la arteria temporal en la localización del nódulo. Se realizó escisión con curación de la paciente y la histopatología mostró hallazgos de arteritis temporal juvenil.
ConclusionesLa arteritis temporal en pacientes jóvenes es una entidad infrecuente, ante la cual siempre hay que descartar manifestaciones sistémicas mediante una anamnesis, exploración física reglada y pruebas complementarias. La anatomía patológica establecerá el diagnóstico definitivo. El tratamiento suele ser quirúrgico. Tras dicho tratamiento, se deberá seguir a la paciente por el posible desarrollo posterior de otras enfermedades.
We present a review of the cases to date of temporal artery vasculitis in young patients in relation to a case in a 39-year-old patient.
Presentation of the caseThis is an obese female, smoker of 25 packs/year and with hypoventilation-obesity syndrome treated with continuous positive airway pressure (CPAP). She was under treatment with fluoxetine and chlordiazepoxide for reactive depression and had no personal or family history of rheumatological disease.
A tumour was found of 1 cm in diameter in the left temporal region, not painful with local bleeding after scratching and minimal growth over the last three months. She reported bitemporal headache of tension characteristics of one year’s duration. She did not present girdle weakness, impaired vision, joint symptoms, or other signs of systemic disease. On examination this nodule was slightly sensitive and with a palpable pulse, with no other findings.
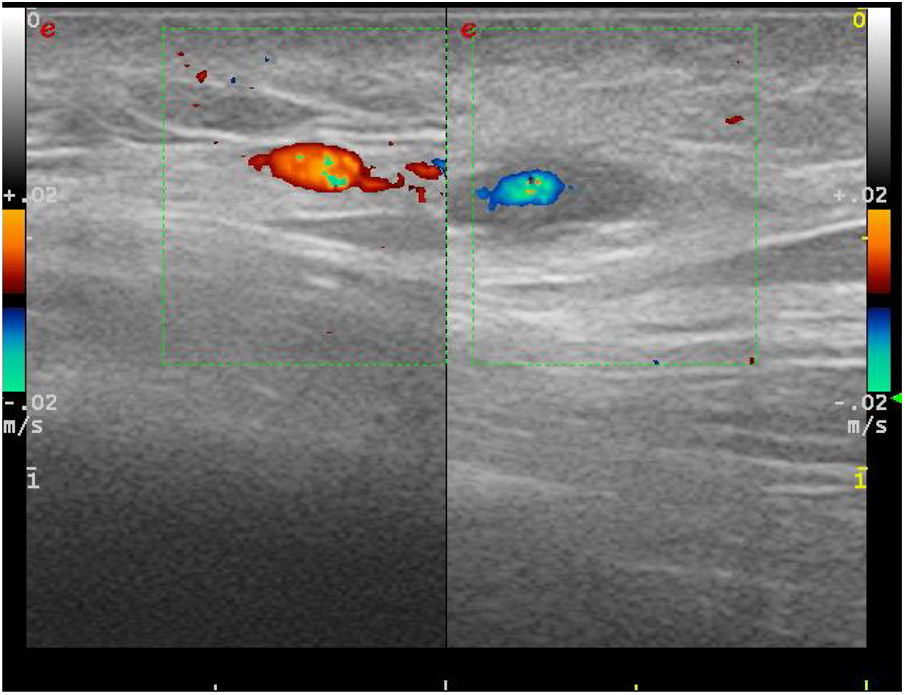
Complementary tests were performed showing a normal haemogram, with a first-hour erythrocyte sedimentation rate of 8 mm (normal 0–25), C-reactive protein 4.4 mg/L (0–10), coagulation tests with no abnormalities and complete biochemistry with nutritional profile, liver tests, renal function, thyroid function, ions, ferrokinetic profile, vitamin B12, vitamin D and folic acid within normal limits. The proteinogram, quantification of immunoglobulins including IgE, antinuclear antibodies and neutrophil antibody, rheumatoid factor and complement were negative or normal. Syphilis, HIV and hepatotropic virus serologies were negative. Chest X-ray, ophthalmological examination and urinary sediment were performed without findings. An ultrasound scan of the nodular zone was performed, and a halo in the shape of a hypoechogenic perivascular cuff and with arterial flow was obtained, suggesting a branch of the temporal artery (Fig. 1).
The lesion was excised which revealed an artery with hyperplasia and intimal fibrosis, and presence in the periarterial connective tissue of an angiolymphoid hyperplasia with some eosinophils. No multinucleated giant cells were observed. This microscopic description is compatible with juvenile arteritis.
DiscussionUltrasound findings in the presence of giant cell arteritis are described in Maldini et al.1 in patients under 50 years of age and arise in a young patient in the case of Durant et al.2 In the case of a temporal arteritis in a young patient, a differential diagnosis should be considered between juvenile temporal arteritis, giant cell arteritis and temporal arteritis in the context of a systemic vasculitis, due to both prognosis and the different treatment possibilities.3
The most common temporal arteritis is giant cell arteritis. It is a segmental granulomatous vasculitis of large and medium vessels. It is rare in young patients and 99% of cases occur in patients over 50 years of age.
Temporal arteritis has been described in association with different systemic vasculitis: polyarteritis nodosa,4 eosinophilic granulomatosis, granulomatosis with polyangiitis, or even vasculitis secondary to infections (borreliosis, syphilis, human immunodeficiency virus).5 In these cases, it is usually accompanied by manifestations in other locations, analytical findings of an immunological nature or radiological manifestations.
Juvenile temporal arteritis is a condition described for the first time by Lie et al.6 In 1994, Tomlinson described some diagnostic criteria associated with this entity7 that were used for the diagnosis of our patient: onset in children and young people, absence of associated manifestations such as myalgias, visual alterations, fever, anaemia, painless temporal nodule, normal sedimentation rate, eosinophilic panarteritis and thrombosis with or without microaneurysmal rupture of the artery, intimal proliferation, disruption of the media and extensive infiltration consisting of lymphocytes, eosinophils and plasma cells, absence of granulomatous infiltration and giant cells. Described cases of juvenile arteritis have subsequently appeared which as they progressed were associated with different processes, including Kimura's disease8,9 in these cases linked to eosinophilia, lymph node and salivary involvement, T lymphoma and angiolymphoid hyperplasia with eosinophilia (ALHE), a rare disease characterised by single or multiple angiomatous lesions usually located on the scalp and face.
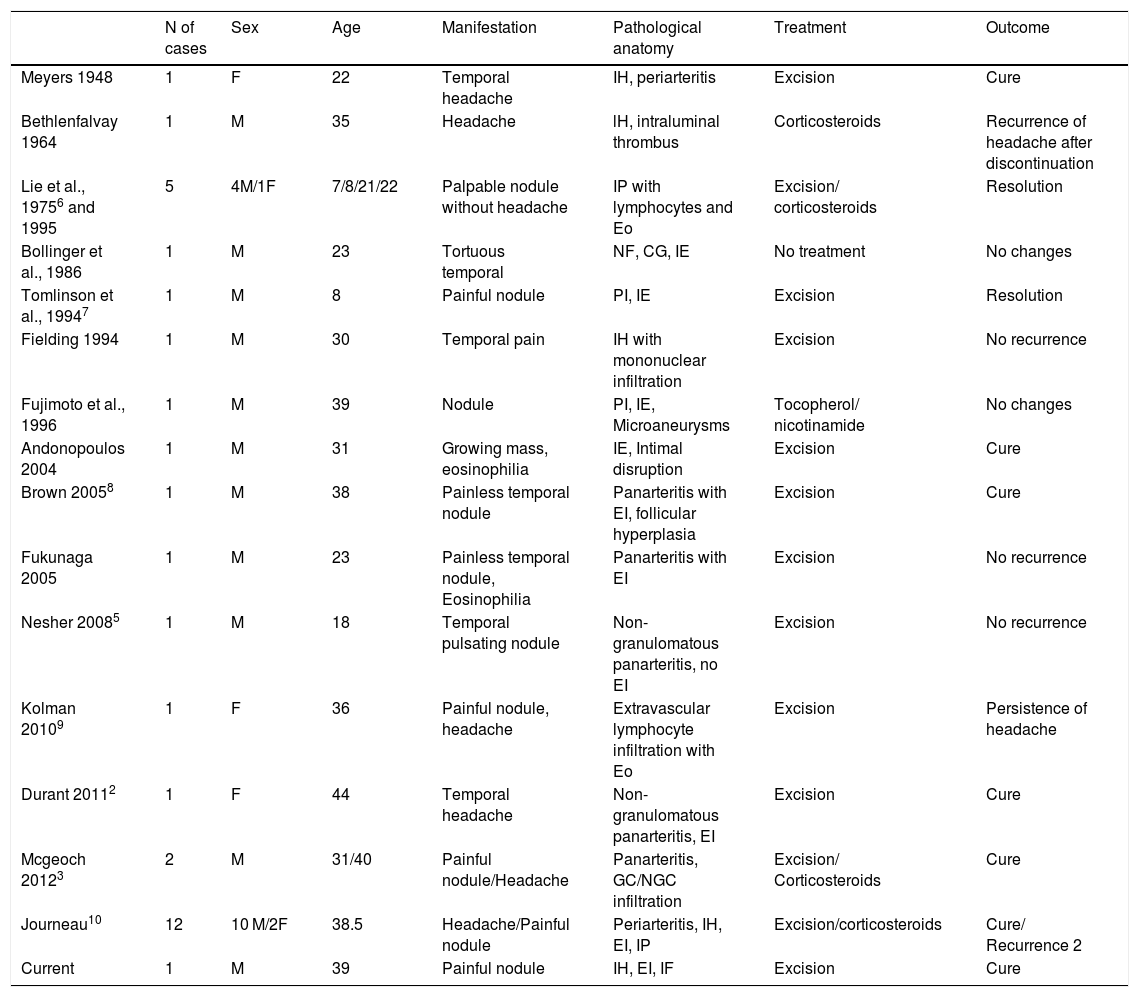
We reviewed the cases of juvenile arteritis described in the literature, including the cases recently described in the French multicentre experience11 (Table 1). A total of 32 patients have been described, the condition being more frequent among males (26 cases) with an average age of 32.5 years (between 7 and 44 years). In terms of clinical presentation, 31.2% debuted with headache and 65.6% with palpation of a nodule. Seventy-five percent were treated with surgical excision without subsequent recurrence, with persistence of headache in one patient. Other treatments were systemic corticosteroids in combination with surgery, or as the only treatment in one case whose headache recurred after the corticosteroids were discontinued. In our case, after surgical excision of the lesion, the patient was asymptomatic, with no other manifestations or development of complications after 18 months of follow-up.
Cases of juvenile arteritis described in the literature.
| N of cases | Sex | Age | Manifestation | Pathological anatomy | Treatment | Outcome | |
|---|---|---|---|---|---|---|---|
| Meyers 1948 | 1 | F | 22 | Temporal headache | IH, periarteritis | Excision | Cure |
| Bethlenfalvay 1964 | 1 | M | 35 | Headache | lH, intraluminal thrombus | Corticosteroids | Recurrence of headache after discontinuation |
| Lie et al., 19756 and 1995 | 5 | 4M/1F | 7/8/21/22 | Palpable nodule without headache | IP with lymphocytes and Eo | Excision/ corticosteroids | Resolution |
| Bollinger et al., 1986 | 1 | M | 23 | Tortuous temporal | NF, CG, IE | No treatment | No changes |
| Tomlinson et al., 19947 | 1 | M | 8 | Painful nodule | PI, IE | Excision | Resolution |
| Fielding 1994 | 1 | M | 30 | Temporal pain | IH with mononuclear infiltration | Excision | No recurrence |
| Fujimoto et al., 1996 | 1 | M | 39 | Nodule | PI, IE, Microaneurysms | Tocopherol/ nicotinamide | No changes |
| Andonopoulos 2004 | 1 | M | 31 | Growing mass, eosinophilia | IE, Intimal disruption | Excision | Cure |
| Brown 20058 | 1 | M | 38 | Painless temporal nodule | Panarteritis with EI, follicular hyperplasia | Excision | Cure |
| Fukunaga 2005 | 1 | M | 23 | Painless temporal nodule, Eosinophilia | Panarteritis with EI | Excision | No recurrence |
| Nesher 20085 | 1 | M | 18 | Temporal pulsating nodule | Non-granulomatous panarteritis, no EI | Excision | No recurrence |
| Kolman 20109 | 1 | F | 36 | Painful nodule, headache | Extravascular lymphocyte infiltration with Eo | Excision | Persistence of headache |
| Durant 20112 | 1 | F | 44 | Temporal headache | Non-granulomatous panarteritis, EI | Excision | Cure |
| Mcgeoch 20123 | 2 | M | 31/40 | Painful nodule/Headache | Panarteritis, GC/NGC infiltration | Excision/ Corticosteroids | Cure |
| Journeau10 | 12 | 10 M/2F | 38.5 | Headache/Painful nodule | Periarteritis, IH, EI, IP | Excision/corticosteroids | Cure/ Recurrence 2 |
| Current | 1 | M | 39 | Painful nodule | IH, EI, IF | Excision | Cure |
EI: Eosinophilic infiltration; Eo: Eosinophils; F: Female; FN: Fibrinoid necrosis; GC: Giant cells; IF: Intimal fibrosis; IH: Intimal hyperplasia; IP: Intimal proliferation; M: Male; NGC: Non-giant cells;.
Juvenile arteritis is a rare entity, which requires a high rate of suspicion. It usually manifests with local symptoms such as a nodule or temporal headache and may show ultrasound halo signs like temporal arteritis. The outcome is usually favourable, with recovery in most patients after surgical excision.
Please cite this article as: Blanco-Alonso S, Mellor-Pita S, Alfageme F, Najera Botella L, Duran-Campo P, Tutor-Ureta P. Arteritis de la temporal en paciente joven. A propósito de un caso clínico. Reumatol Clin. 2021;17:297–299.