Whipple's disease was first described by George Hoyt Whipple in 1907. It is a multisystem infectious disease, produced by Tropheryma whipplei, which was identified for the first time in 1991. The name is of Greek origin (trophe nutrient+eryma barrier) and is related to the defective absorption of nutrients characteristic of this disorder. The clinical signs include arthralgia, weight loss, diarrhea and abdominal pain, although the clinical manifestations can vary widely. Thus it may take up to 6 years to be diagnosed. We report 2 cases in which the final diagnosis was Whipple's disease.
Case no. 1The patient was a 47-year-old man, a farmer, who had a 15-month history of polyarthritis in knees, ankles and hands. He was admitted by the gastroenterology department because of abdominal pain, vomiting and fever. Physical examination revealed pain in left abdomen and there appeared to be a mass on palpation. Ancillary tests showed an erythrocyte sedimentation rate of 100mm/h and normochromic anemia, and thoracoabdominal computed tomography (CT) disclosed mesenteric infiltration and lymph nodes in the jejunal loops. Exploratory laparotomy was performed, as was biopsy of the lymph nodes and bowel mesentery. The pathological study resulted in a diagnosis of Whipple disease, with the presence of periodic acid Schiff (PAS)-positive macrophages with intracellular inclusions. The patient was treated with cotrimoxazole for 2 years, accompanied by tetracycline for the first 3 months. Twenty years later, the patient is asymptomatic.
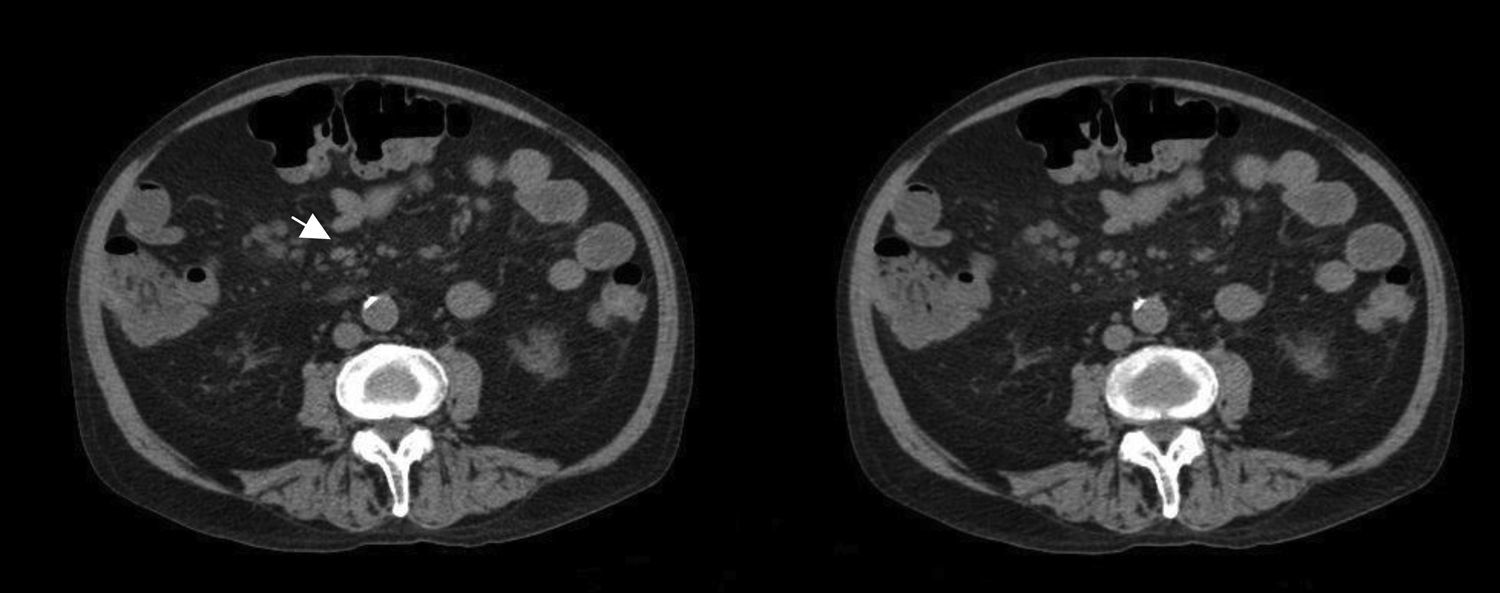
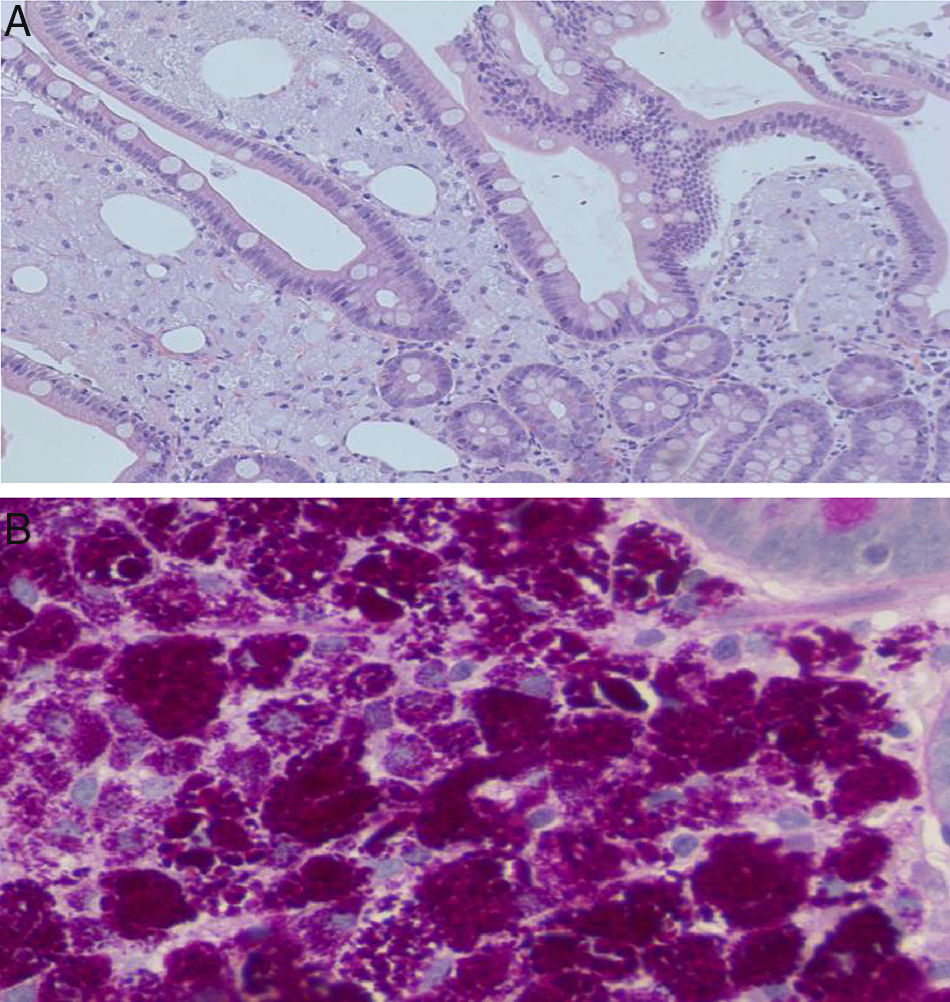
Case no. 2This patient was a 63-year-old man with systemic hypertension, renal failure, arthritis and a 9-year history of low back pain, with a diagnosis of spondyloarthritis. He had posterior uveitis and vitritis affecting right eye and had had 3 episodes of pancreatitis requiring hospital admission in the gastroenterology department. Computed tomography revealed nonspecific mesenteric lymph node enlargement (Fig. 1). Gastroscopy, during which a specimen was removed for biopsy, disclosed erosive disease involving the duodenal bulb. One month later, the patient was readmitted in the gastroenterology department with fever, diarrhea and abdominal pain. According to a duodenal biopsy (Fig. 2) that had been carried out during the earlier hospital stay, the diagnosis was Whipple's disease. Treatment was begun with ceftriaxone and imipenem, and included cefixime during the first 2 months. He was subsequently treated for 2 years with trimethoprim/sulfamethoxazole.
Small bowel (duodenal) biopsy. (A) Intestinal villi with expansion of the lamina propria by numerous pink-colored foamy macrophages (hematoxylin & eosin 20×). Occasional “empty spaces” correspond to extracellular lipid deposits. (B) Macrophages loaded with periodic acid Schiff (PAS)-diastase-positive intracytoplasmic granules (20–40×).
Whipple's disease is frequently associated with rheumatic manifestations (60% of the cases), which precede the gastrointestinal signs in three fourths of the patients. They are often the first symptoms of the disease. They commonly appear in the form of polyarthritis, generally chronic, intermittent, seronegative and nonerosive,1 although cases have been reported in which there are atypical rheumatic symptoms such as spondylodiscitis,2 erosive arthritis,2 and even osteonecrosis of the hip. The joints most frequently affected are the carpi and large joints of the lower limbs. When the diagnosis is uncertain, it is important to rule out this disease in patients with seronegative arthritis and signs associated with the digestive tract prior to initiating biological therapies, since the use of the latter can have a negative effect on the disease course.3
The improvement of the symptoms with the administration of antibiotics taken for another reason, as well as the lack of improvement or clinical deterioration with immunosuppressive therapy should lead to the suspicion of Whipple's disease.
Biopsy of the synovium and intestinal mucosa may reveal a PAS-positive monocytic infiltrate.4 The development of the technique of polymerase chain reaction has made it possible to identify the genetic material of the bacteria in different tissues and body fluids,4,5 which suggests that the cause of the arthritis in this disease is septic. It is also possible to culture the bacteria once isolated from synovial fluid. On occasion, the study of the joints may be diagnostic, even if the examination of the intestine is negative.4
Although the genetic material of T. whipplei has been demonstrated in the joints of healthy individuals, there is no clear consensus regarding the treatment of Whipple's disease. The most widely accepted approach is the administration of intravenous ceftriaxone or another broad spectrum β-lactam antibiotic for 2 weeks, followed by oral trimethoprim/sulfamethoxazole over a variable period of time, which is usually 1 year. A recent study recommends the combination of doxycycline and hydroxychloroquine for 1 year, and the maintenance of doxycycline for life, to avoid relapses that can occur with the preceding regimen. The clinical improvement is sweeping, the gastrointestinal recovery takes place before changes are observed in the joints, and the neurological findings are less predictable.6,7
In short, Whipple's disease is an uncommon disorder that should be taken into account because of its potential fatal outcome in the absence of treatment and because of its wide variety of clinical manifestations. We wish to stress the importance of the rheumatic signs because they develop quite frequently, as well as the need to establish the correct differential diagnosis with regard to other rheumatic diseases, to avoid therapeutic measures that can be detrimental to the patient.
Please cite this article as: Moreno García MS, Casorrán Berges M, del Río-Martínez PS, Bosque Peralta MT. Enfermedad de Whipple, la gran desconocida. Reumatol Clin. 2017;13:243–244.