Uveitis occurs within the first year of arthritis onset in 73% of patients with juvenile idiopathic arthritis (JIA) considered at risk. The intraocular inflammation is characterized by an insidious onset and a silent and chronic clinical course capable of producing significant visual loss due to complications such as: cataract formation, secondary glaucoma, maculopathy and optic neuropathy. The absence of initial signs and symptoms, along with a deficient ophthalmic monitoring produces a delay in diagnosis with serious consequences. It has been estimated that 47% of JIA patients at risk for developing uveitis are legally blind (20/200 or worse) at least in one eye at the time of their first visit to the ophthalmologist. To reduce ocular complications and improve their visual outcome, it is necessary that rheumatologists refer all patients recently diagnosed (within the first month) with JIA for an ophthalmic evaluation, and maintain periodical follow-up visits based on classification and risk category of the disease.
La uveítis ocurre dentro del primer año del inicio de la artritis en hasta el 73% de los pacientes con artritis idiopática juvenil (AIJ) considerados en riesgo. La inflamación intraocular se caracteriza por un inicio insidioso y un curso clínico silencioso y crónico, capaz de producir pérdida visual significativa debido a complicaciones como: formación de cataratas, glaucoma, maculopatía y neuropatía óptica. La ausencia de signos y síntomas oculares iniciales, aunado a una deficiente monitarización oftalmológica, producen un retraso diagnóstico de graves consecuencias. Se ha reportado ceguera legal (20/200 o peor) en al menos un ojo en hasta el 47% de aquellos pacientes en riesgo para desarrollar uveítis durante la primera visita oftalmológica. Para reducir las complicaciones oculares y mejorar el pronóstico visual, es necesario referir inmediatamente a pacientes recién diagnosticados con AIJ por el reumatólogo a evaluación oftalmológica y mantener visitas periódicas de seguimiento basadas en la clasificación y la categoría de riesgo de la enfermedad.
Juvenile idiopathic arthritis (JIA) is a chronic, debilitating inflammatory disease, which primarily affects the joints, and in varying degrees presents extra-articular involvement, affecting mainly children.1
Reports on the incidence and prevalence of JIA are difficult to compare between populations due to the heterogeneity of the disease, the different classification criteria employed, the nature of the ethnic groups studied and the diagnostic certainty in each case.2 Consequently, the results shown in various studies vary significantly, with an incidence ranging from 0.8 to 22.6/100 000 persons <16 years per year and a prevalence ranging from 7 to 400/100 000 children and adolescents.3
In Mexico, there are no current figures for the prevalence of JIA; however, it is inferred that it could be at least 2 cases per 100 000 population and with an estimated annual incidence of 0.7–0.8 new cases per 100 000 population.3
JIA is a heterogeneous group of chronic arthropathies with an onset before age 16 and that must have a duration of at least 6 weeks. According to the classification of the International League of Associations for Rheumatology (ILAR), there are 7 subtypes of the disease (Table 1).1 These subtypes differ in clinical manifestations, autoimmune features, genetic and prognostic determinants.2 These clinical variants, along with some demographic characteristics, have been considered as risk factors for the development of uveitis,4–6 the most frequent extraarticular manifestation of JIA 7. In patients with oligoarticular forms, and particularly in the presence of antinuclear antibodies (ANA), the occurrence of uveitis is approximately 20%, decreasing to 10.5% in patients with polyarticular disease with negative rheumatoid factor, being almost nonexistent in patients with systemic variants and with a positive rheumatoid factor.8,9 In Mexico, prevalence of uveitis associated with JIA has been reported as 16.3%, being more frequent in girls (87.5%) at an early age (5.7 years) with oligoarticular forms (75.0%) and with the presence of ANA in 80% of cases.10 These findings are consistent with the risk factors most associated with the occurrence of uveitis in JIA reported in the literature, namely: female gender, younger age of onset of arthritis, oligoarticular forms and the presence of ANA.4,9 Finally, a meta-analysis of JIA studies published between 1980 and 2004 concluded that early age at onset, positive ANA and oligoarticular and polyarticular forms are the highest risk factors for developing uveitis, while ANA-negative patients with disease onset at 4 years of age are at a moderate risk category, regardless of the presentation of JIA.11
Classification of JIA According to the International League of Associations for Rheumatology (ILAR).
| JIA |
| Systemic onset JIA |
| Oligoarticular JIA |
| Persistent |
| Extended |
| Polyarticular JIA RF (−) |
| Polyarticular JIA RF (+) |
| Psoriatic arthritis |
| Enthesitis related arthritis |
| Undifferentiated |
| Does not fall into any category |
| Enters into more than one category |
JIA, juvenile idiopathic arthritis; RF, rheumatoid factor.
Although the highest prevalence of JIA has been reported in Scandinavian countries, followed by countries in northern Europe and North America it is unknown whether uveitis associated with JIA dominates in a particular ethnic group.2 Moreover, to understand the role of genetic traits in the occurrence of uveitis associated with JIA, a large number of pairs of siblings with the disease has been analyzed12 without sufficient evidence for a specific genetic component linked to the pathogenesis of uveitis associated with JIA.13,14 However, the findings do not rule out a modest association with a specific genetic marker (relative risk genotype) because its frequency is relatively high.15
Regarding the association with alleles of major histocompatibility complex antigens (HLA), HLA profiles have been studied in patients with oligoarticular JIA associated to early uveitis. Some series found a significant increase in the frequency of HLA-DRB1*1104 (a fragment of HLA-DR5) in patients with chronic uveitis, compared with those without intraocular inflammation.16,17 However, other studies have failed to demonstrate this fact.18 Moreover, in all series examined, the frequency of HLA-DRB1*0118 was reduced.
Intraocular Inflammation Associated With Juvenile Idiopathic ArthritisUveitis is one of the leading causes of preventable blindness in the world. In the pediatric population, the annual incidence of uveitis has been estimated between 4.3 and 6.9/100 000.19–21 When analyzed in the context of the various causes of childhood uveitis, uveitis associated with JIA represents up to 47% of cases in the United States and Europe,19,22 and from 1% to 11% of anterior uveitis in highly specialized centers worldwide.23,24 It has been reported that up to 10% of cases, anterior uveitis is the first manifestation of JIA.11 An important point to consider is that anterior uveitis is often detected during the first ophthalmology visit, early in the clinical course of JIA.25 In a multicenter study conducted in 2007, in which 3271 patients with JIA from 35 centers were analyzed, it was found that 406 patients (12%) had uveitis, of which 115 (28%) patients with a documented clinical course of uveitis were analyzed. The vast majority (79%) had an oligoarticular form of arthritis, started early and were predominantly women with positive ANA. This study revealed that up to 73% of patients with JIA had uveitis before or within the first 12 months of the onset of arthritis, and 77% and 90% occurred within the first 2 and 4 years after its onset,26 respectively. Moreover, at the time of presenting JIA, complications had been reported in 67% of uveitis affected eyes.27
The intraocular inflammatory process in patients with JIA is characterized by an insidious anterior uveitis, as well as a chronic silent clinical course which leads to a significant visual loss due to many serious complications, including formation of calcium band keratopathy, posterior and anterior iris synechia, cataract, secondary glaucoma, vitreitis, maculopathy and chronic optic neuropathy and ocular cyclitic hypotony by forming a membrane and complete loss of function with bulbar phthisis.28–30
Initially, the patient with intraocular inflammation associated with JIA shows no classic signs or symptoms associated with uveitis, specifically: red eye, eye pain, photophobia and blurred vision 9. This stage is critical in developing eye disease, because the lack of events can last from several months to years, and it is not until the first complications of uveitis appear that patients, their families or the attending physician detect its presence.31,32
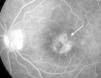
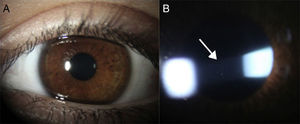
It is during this stage of the disease that regular ophthalmologist visits are key for the early detection of intraocular inflammation, which can only be noted through careful observation under slit lamp examination which shows inflammatory cells floating in the aqueous humor of the anterior chamber10,31 (Fig. 1A and B).
(A) Eye with chronic anterior uveitis associated with JIA without showing evidence of inflammation upon superficial examination. (B) Same eye under slit lamp examination showing Tyndall phenomenon (protein exudation) and inflammatory cells (arrow) floating in the aqueous humor of the anterior chamber.
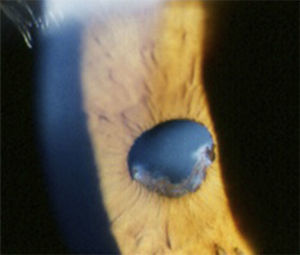
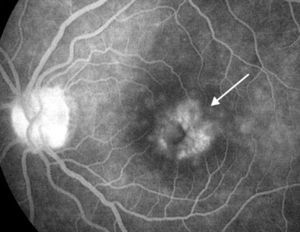
The first complications, such as calcium band keratopathy, the appearance of the posterior iris synechiae and the onset of cataract formation, can then produce photophobia and visual loss27–29,33 (Fig. 2). In the only report of Mexican patients with uveitis associated with JIA, eye exams in the first visit found 55.2% of affected eyes with complications, the most common being formation of posterior synechiae of the iris (56.2%), followed by calcium band keratopathy (50.0%) and cataract formation (31.2%).10 Then, if uveitis was still undetected, or if medical treatment was inadequate, more serious complications appeared, in addition to the progression of cataracts, such as vitreitis, cystoid macular edema, glaucoma secondary to pupillary blockage or angular closure through the formation of posterior and anterior iris synechia, respectively, and ischemic or inflammatory optic neuropathy, among others5,33 (Fig. 3). In a study of 89 children with JIA-associated uveitis, maculopathy (edema and scarring) was found in 26% of affected eyes, as well as epiretinal or neovascular membranes in 10% of eyes, ocular hypotony in 10%, papilledema and optic neuritis in 3%, and retinal detachment in 3% of the eyes.30 The results of another study that analyzed the ocular complications that seriously threaten the vision of patients with uveitis associated with JIA are equally disappointing, showing high rates of cataract formation (70%), macular edema demonstrated by angiography (32%), vitreous opacity (25%), glaucomatous optic neuropathy (21%) and ocular hypotonia (17%)34 (Table 2).
Ocular Complications Most Frequently Reported in Patients With Uveitis Associated With JIA.
| Ocular complication | Kotaniemi et al.,25% (No.=104) | Woreta et al.,27% (No.=75) | Kump et al.,30% (No.=89) | Heiligenhaus et al.,26% (No.=100) | López-Rubio et al.,10% (No.=16) |
|---|---|---|---|---|---|
| Band keratopathy | 7.0 | 31.5 | 46.0 | 21.0 | 50.0 |
| Posterior synechiae | ND | 27.5 | 58.0 | 31.0 | 56.2 |
| Glaucoma | 8.0 | 15.3 | 20.0 | 6.0 | 31.2 |
| Cataract | 22.0 | 45.6 | 64.0 | 26.0 | 31.2 |
| Maculopathy | 8.0 | 6.4 | 26.0 | 4.0 | ND |
| Optic neuropathy | ND | 4.5 | 3.0 | 7.0 | ND |
| Othersa | ND | 9.3 | 10.0 | 9.0 | ND |
ND, not determined.
These figures are compelling clinical evidence that the occurrence of ocular complications is not uncommon in JIA, especially considering that uveitis is often overlooked by the rheumatologist, pediatrician and even the patient, and only becomes apparent until substantial and permanent visual loss occurs.34 In this regard, it is important to re-emphasize that the vast majority of these uncommunicative children do not present with ocular signs and symptoms that demonstrate the presence of intraocular inflammation. This causes parents and other relatives to not notice the presence of ocular pathology, contrary to what happens with articular and systemic manifestations.9,35 This fact makes it imperative to identify the risk factors for onset of uveitis in children with JIA, as well as implement the best strategy for their early detection.
Visual Impact of Uveitis Associated With Juvenile Idiopathic ArthritisThe visual impact of uveitis associated with JIA has been studied and reported by many authors. However, awareness of its importance among multidisciplinary groups involved in the care of these patients has not been sufficiently effective to this day. Substantial visual loss, 47% of legal blindness patients (20/200 or worse) in at least one eye, has been reported during the first visit of patients with uveitis associated with JIA.27,36
The severity of ocular disease during the initial eye examination has been considered as a risk factor for a poor long-term visual prognosis in these patients.34,36 Other predictors of poor visual prognosis in these cases include: the onset of uveitis before or at the time of diagnosis of JIA; a short period between the onset of arthritis and uveitis, and male gender.34,37–39
Ophthalmologic Monitoring in Patients With Juvenile Idiopathic ArthritisMonitoring guidelines for the early detection of uveitis in JIA vary across countries and are based on the perception of risk for intraocular inflammation.6 As previously mentioned, the risk factors for developing uveitis in JIA patients that have been considered in most publications include: the pattern of initial presentation of arthritis; gender, status of the ANA and age at onset of arthritis.4,7,34 However, most of the guidelines established so far do not address the risk of visual loss in these patients, and reducing blindness must be the primary purpose of monitoring programs and follow-up of31 patients with JIA.
With respect to optimal intervals between ophthalmologic evaluations to prevent visual loss, the latest recommendations for monitoring the occurrence of uveitis in JIA patients were published in 2006 by the American Academy of Pediatrics in conjunction with a panel of experts composed of rheumatologists and ophthalmologists.7 A year later the German Uveitis in Children Study Group suggested a number of changes to these guidelines26 (Table 3). The guidelines allow for earlier detection of uveitis in JIA patients, thereby significantly reducing the large proportion of serious ocular complications reported until today during the first visit to specialized clinics. The frequency of ocular complications in children with JIA-associated uveitis has been estimated between 34% and 67% of cases,27,36 reaching an average prevalence of up to 86.3% after 3 years of their initial presentation. The fact that, at the time of her first visit eye, almost half of JIA patients at high risk of developing uveitis present legal blindness in one eye developed from ocular complications secondary to intraocular inflammation is worrysome.36 In addition, the occurrence of ocular complications and sequelae arising from a prolonged clinical course of the disease during long-term monitoring of these patients does not always receive the necessary consideration by the group of specialists caring for patients with this disease, as evidenced by various publications.37,38,40
Suggested Intervals for Ophthalmic Screening of Patients With JIA According to the Classification Criteria of the International League of Associations for Rheumatology (ILAR).
| JIA subgroup | ANA | Home AIJ age (years) | JIA duration (years) | Recommended screening intervals (months) |
|---|---|---|---|---|
| OA; PA RF (−); PsA; other arthritis | + | ≤6 | ≤4 | 3 |
| OA; PA RF (−); PsA; other arthritis | + | ≤6 | >4 | 6 |
| OA; PA RF −, PsA, other arthritis | + | ≤6 | ≥7 | 12 |
| OA; PA RF (−); PsA; other arthritis | + | >6 | ≤2 | 6 |
| OA; PA RF (−); PsA; other arthritis | + | >6 | >2 | 12 |
| OA; PA RF (−); PsA; other arthritis | – | ≤6 | ≤4 | 6 |
| OA; PA RF (−); PsA; other arthritis | – | ≤6 | >4 | 12 |
| OA; PA RF (−); PsA; other arthritis | – | >6 | N/A | 12 |
| Enthesitis related arthritis | N/A | N/A | N/A | 12 |
| PA RF(+); systemic arthritis | N/A | N/A | N/A | 12 |
| Patients with uveitis | N/A | N/A | N/A | According to the course of uveitis |
PsA, psoriatic arthritis; RF (−), seronegative; RF (+), HIV positive; NA, not applicable; OA, oligoarticular; PA, polyarticular.
Obviously, this becomes very relevant when we consider that these consequences can be avoided if these children and adolescents are monitored and receive appropriate and timely treatment by qualified ophthalmologists.
Recommendations for Ophthalmologic Monitoring and Follow-up of Patients With Juvenile Idiopathic ArthritisThe purpose of this report is to reiterate the commitment that healthcare professional and multidisciplinary teams caring for patients with JIA have to provide for adequate care for these patients. To consolidate this strategy, certain recommendations have been made and have to be effectively applied by the medical team involved in the care of children with JIA. These recommendations are listed below:
- 1.
Refer immediately (within one month) the patient newly diagnosed with JIA by the rheumatologist to ophthalmologic evaluation for early detection of uveitis.7,11,26,41
- 2.
After the initial review, regular ophthalmologic visits should be kept, based on the classification and category of risk of the disease (Table 3).26
- 3.
It is recommended to change the clinical follow-up strategy every 6–12 months in patients with positive ANA and onset of JIA >6 years of age who have not presented uveitis within the first 2 years after diagnosis of JIA.26,27,42Note: the risk of developing further complications between the 4–6 years after the onset of JIA is minimal, which justifies the change in the monitoring strategy of these patients.
- 4.
If the patient is older than 6 years old and the rheumatologist has a strong suspicion of JIA or the patient has positive ANA, the specialist must proactively refer the patient to an ophthalmologic examination in search of uveitis.26,27,43Note: Because the greatest risk for developing uveitis is in patients younger than 2 years old and ANA positive, it is beneficial to schedule an eye examination as soon as possible for these patients. This could be before or on the day of rheumatology evaluation.
- 5.
It is advisable that all ophthalmic evaluations are conducted under a slit lamp by experienced ophthalmologist pediatricians or preferably, specialists in ocular immunology and uveitis.6,7,26
However, by themselves, these strategies will not eliminate all of the ocular complications. This is because that although some patients are sent to the ophthalmologist from the onset of the joint disease and early detection of uveitis is carried out, other factors such as improper handling of immunosuppression, adverse economic conditions, poor patient therapeutic compliance and the aggressive nature of intraocular inflammation, results in irreversible visual sequelae in a high percentage of cases. Only a dual strategy based on improving early and periodic screening of patients and the development of more effective treatments for the disease can truly prevent eye complications in these patients.
To complete this dual strategy we still have the difficult task of improving the therapeutic regimens, adherence to treatment and education for patients with JIA and their families in order to reach a comprehensive management of eye and joint disease.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients, and all patients included in the study have received sufficient information and gave written informed consent to participate in the study.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no conflict of interest to state.
Please cite this article as: Rodríguez-García A. Importancia de la evaluación oftalmológica en pacientes con artritis idiopática juvenil. Reumatol Clin. 2015;11:133–138.