To identify clinical or immunological features in patients with undifferentiated connective tissue disease (UCTD) associated interstitial lung disease (ILD), in order to group them and recognize different functional and high resolution computed tomography (HRCT) behavior.
MethodsRetrospective cohort study. Patients meeting Kinder criteria for UCTD were included. We defined the following predictive variables: ‘highly specific’ connective tissue disease (CTD) manifestations (Raynaud's phenomenon, dry eyes or arthritis), high antinuclear antibody (ANA) titer (above 1:320), and ‘specific’ ANA staining patterns (centromere, cytoplasmic and nucleolar patterns). We evaluated the following outcomes: change in the percentage of the predicted forced vital capacity (FVC%) during the follow-up period, and HRCT pattern.
ResultsSixty-six patients were included. Twenty-nine (43.94%) showed at least one ‘highly specific’ CTD manifestation, 16 (28.57%) had a ‘specific’ ANA staining pattern and 29 (43.94%) high ANA titer. Patients with ‘highly specific’ CTD manifestations were younger (mean [SD] 52 years [14.58] vs 62.08 years [9.46], P<.001), were more likely men (10.34% vs 48.65%, P<.001) and showed a smaller decline of the FVC% (median [interquartile range] 1% [−1 to 10] vs −6% [−16 to −4], P<.006). In the multivariate analysis, the presence of highly specific manifestations was associated with improvement in the FVC% (B coefficient of 13.25 [95% confidence interval, 2.41 to 24.09]). No association was observed in relation to the HRCT pattern.
ConclusionThe presence of ‘highly specific’ CTD manifestations was associated with female sex, younger age and better functional behavior. These findings highlight the impact of the clinical features in the outcome of patients with UCTD ILD.
Agrupar a los pacientes con enfermedad pulmonar intersticial (EPI) asociada a enfermedad indiferenciada del tejido conectivo (EITC) según la presencia o no de ciertas manifestaciones clínicas o inmunológicas, esperando encontrar diferentes expresiones tomográficas o funcionales.
MétodosEstudio de cohortes retrospectivas. Se incluyeron pacientes que cumplían criterios de Kinder para EITC. Se consideraron variables predictoras: manifestaciones «altamente específicas de enfermedad del tejido conectivo (ETC)» (Raynaud, xeroftalmia o artritis), títulos altos de anticuerpos antinucleares (ANA) (mayores a 1:320) y patrones específicos de ANA (centromérico, citoplásmico y nucleolar). El cambio en la capacidad vital forzada % (CVF%) en el tiempo y el patrón en TCAR fueron las variables de resultado estudiadas.
ResultadosSe incluyeron 66 pacientes. Veintinueve presentaron al menos una manifestación «altamente específica de ETC» (43,94%), 16 ANA específico (28,57%) y 29 ANA alto título (43,94%). Aquellos con manifestaciones «altamente específicas de ETC» presentaron menor frecuencia de sexo masculino (10,34% vs 48,65%, p<0,001), menor edad en años (media 52 [DE14,58] vs 62,08 [9,46], p<0,001) y menor mediana de declinación de CVF% (1[RIC −1 a 10] vs −6 [RIC −16 a −4], p<0,006). En el análisis de regresión lineal múltiple la presencia de manifestaciones «altamente específicas de ETC» se asoció con mejoría en CVF% (coeficiente B de 13,25 [IC 95% 2,41 a 24,09]). No encontramos asociaciones en cuanto al patrón en TACAR.
ConclusionesLa presencia de manifestaciones «altamente específicas de ETC» se asoció con sexo femenino, menor edad al inicio y una evolución más favorable en cuanto a la CVF%, lo cual evidencia el impacto de las manifestaciones clínicas en la evolución de estos pacientes.
The diagnosis of idiopathic interstitial pneumonia requires the exclusion of other known causes of interstitial lung disease (ILD), among them connective tissue diseases (CTD). The most conservative recommendations suggest the determination of rheumatoid factor (RF) and antinuclear antibodies (ANA) together with a questionnaire for the purpose of ruling out a CTD, although it is considered that screening for the presence of other antibodies (anti-Ro/SS-A, anti-La/SS-B, anti-Jo-1, etc.) could be useful in selected cases.1,2 As a consequence of these recommendations, it is common to encounter positive findings in the physical examination, questionnaires and/or immunology laboratory tests in patients that do not meet the classification criteria for a particular CTD, but are diagnosed as having a syndrome that has had many names, one of which is undifferentiated connective tissue disease (UCTD).3 This disorder is characterized by a considerable heterogeneity in terms of the demographic, clinical and morphological (histological and tomographic) characteristics as well as the outcome.4–8 The existence of highly sensitive classification criteria proposed by a number of authors has contributed to the heterogeneity.4,5,9,10 An intersociety consensus was recently published that attempts to clarify the definition of this disorder referred to as “interstitial lung disease (or interstitial pneumonia) with autoimmune features”, although the proposed criteria have not been validated.11 Beneath the hypothesis there is an underlying idea that this condition affects at least 2 different groups of patients. First, there would be a group of patients with inflammatory ILD, associated with an incomplete CTD that might or might not be detected throughout the course of the disease. Secondly, there would be another group of patients with fibrotic ILD, with a clinical profile similar to that of idiopathic pulmonary fibrosis (IPF), with false positive results according to the immunology laboratory, accompanied by nonspecific extrapulmonary clinical manifestations that are prevalent in the general population.12 In this context, the main objective of our study was to group the patients according to the presence or absence of certain clinical manifestations or immunological features, hoping to observe that these groups had different tomographic and/or functional expressions.
Materials and MethodsThis is an observational study involving retrospective cohorts. We reviewed the medical records of all the patients hospitalized in the ILD clinic of the Instituto Nacional de Enfermedades Respiratorias Ismael Cosio Villegas (INER) (Mexico) between January 2012 and December 2014, and of all of the outpatients attended to in the ILD unit of Hospital María Ferrer (HMF) in Buenos Aires, Argentina, between January 2012 and June 2015. The patients provided their written consent. We included those patients with ILD who met the Kinder criteria for UCTD (Table 1).3 We excluded patients who met the criteria for a defined CTD in accordance with the criteria of the American College of Rheumatology or for some other cause of known interstitial disease.
Kinder Criteria for Patients With Interstitial Lung Disease Associated With Undifferentiated Connective Tissue Disease.
| Diagnostic criteria | Presence of |
|---|---|
| Symptoms associated with connective tissue disease | At least one of the following symptoms |
| 1. Raynaud's phenomenon | |
| 2. Arthralgia/multiple joint swelling | |
| 3. Photosensitivity | |
| 4. Unintentional weight loss | |
| 5. Morning stiffness | |
| 6. Xerostomía or xerophthalmia (sicca symptoms) | |
| 7. Dysphagia | |
| 8. Recurrent unexplained fever | |
| 9. Gastroesophageal reflux | |
| 10. Skin changes (rash) | |
| 11. Oral ulceration | |
| 12. Nonandrogenic alopecia | |
| 13. Proximal muscle weakness |
| Evidence of systemic inflammation in the absence of infection | Positive findings for at least one of the following |
|---|---|
| 1. Antinuclear antibodies (ANA) | |
| 2. Rheumatoid factor (RF) | |
| 3. Anti-Scl-70 | |
| 4. Anti Ro/SS-A or La/SS-B | |
| 5. Anti-Jo-1 | |
| 6. Erythrocyte sedimentation rate (more than twice the normal value), C reactive protein |
We recorded demographic data (age, sex, smoking behavior), clinical findings (respiratory signs/symptoms and those associated with CTD), data provided by the immunology laboratory (ANA, RF and anti-Ro/SS-A, anti-Jo-1, anti-Scl-70, anticentromere and anti-U1 ribonucleoprotein [RNP] antibodies), data on respiratory function (percentage of predicted forced vital capacity [FVC%] and percentage of predicted diffusing capacity of the lung for carbon monoxide [DLCO%] at baseline, as well as changes in FVC% during follow-up), high-resolution computed tomography (HRCT) and surgical lung biopsy. Follow-up included respiratory function test every 4–6meses. With respect to the clinical manifestations, this being a retrospective study, we analyzed those that are usually dealt with in visits to the pulmonologist specialized in ILD in the participating centers (those included in the Kinder criteria). Other more specific manifestations that require the presence of another specialist for their evaluation (for example, mechanic's hands or Gottron's papules) were not analyzed. Data related to treatment were also recorded. In every case, this was indicated by the treating physician according to his or her criteria.
Definition of the VariablesImmunology laboratory: the determination of the RF of the patients of the HMF was performed by nephelometry with a cut-off point of 35U/mL, and in the INER by immunochemiluminescence with a cut-off point of 20U/mL. Indirect immunofluorescence (IIF) was used to detect ANA, with a cut-off titer of 1:80. The determination of anti-Ro/SS-A, anti-Jo-1, anti-U1 RNP and anti-Scl-70 antibodies was done with the enzyme-linked immunosorbent assay (ELISA), with a cut-off value of 20U/mL. Anticentromere antibody was measured using IIF, with a cut-off titer of 1:80. Respiratory function tests: spirometry, plethysmography and DLCO measurements were performed at baseline and every 4–6months in accordance with standardized acceptability and reproducibility criteria.13–16
High-resolution computed tomography was performed with a slice width of 1mm at intervals of 10mm. The results were evaluated by a radiologist who was an expert in interstitial disease. The findings were classified according to standardized criteria as being typical of usual interstitial pneumonia (UIP), possible UIP and inconsistent with UIP.1 Lung biopsies were evaluated by a pathologist with experience in ILD. The results were classified as indicative of UIP, nonspecific interstitial pneumonia (NSIP), organizing pneumonia (OP), NSIP with OP, lymphoid interstitial pneumonia (LIP) and unclassifiable ILD.2 The presence of lymphoid follicles, follicular bronchiolitis, pleural involvement and vascular involvement were also recorded.
A multidisciplinary group defined a priori the signs that should be considered. They consisted of a set of clinical manifestations (Raynaud's phenomenon, xerophthalmia or arthritis), included in the criteria proposed by Kinder, as being highly specific for CTD. The patients who had at least one of them were considered to show highly specific manifestations of CTD. High titers of ANA were considered to be those greater than 1:320, and the patterns specific for ANA were centromere, cytoplasmic and nucleolar. The choice of these ANA patterns as “specific” is linked to their strong association with CTD in which ILD constitutes a common manifestation, which makes it less likely that the test results in a false positive.17,18 These 3 variables (highly specific manifestations of CTD, specific ANA patterns and a high ANA titer) were considered to be major predictive variables. We considered changes in the FVC% over time and the HRCT pattern to be major outcome variables. Sex and age were also evaluated. These variables were chosen as they are characteristics that are expressed differently in an “IPF-like” disease and an inflammatory ILD associated with a CTD.5 Potential confounders were included in a multivariate analysis in the attempt to correct the effect of eventual selection biases.
Statistical AnalysisThe categorical variables were expressed in terms of frequency and the continuous variables as the mean and standard deviation (SD) or median and interquartile range (IQR), depending on whether or not there was a normal distribution, respectively. The univariate analysis was performed using the chi-square test, Fisher's exact test, Student's t test or Wilcoxon rank-sum test, depending the type of variable. Multiple logistic regression analysis was carried out to define the variables that were associated with the presence of a HRCT pattern that was inconsistent with UIP. As covariates in the model, we included the sex, age under 60years, the presence of manifestations that were highly specific for CTD, a specific ANA pattern and a high ANA titer. The adjusted odds ratio (OR) and the 95% confidence intervals (CI) were recorded. Multiple linear regression was utilized to determine which variables were associated with changes in FVC% over time. As independent variables, we included age over 60years, sex, the presence of manifestations that were highly specific for CTD, a specific ANA pattern, high ANA titer, the presence of a pattern that was inconsistent with UIP in the HRCT and whether or not the patient had received a specific treatment. The β coefficients and 95% CI were recorded. A P<.05 was considered to indicate statistical significance. The STATA 13.0 software package was used for the statistical analysis.
ResultsCharacteristics of the CohortsWe reviewed 648 medical records in the INER and 292 in HMF. We included a total of 66 patients, 21 men (31.82%), with a mean age (SD) of 57.65years (12.91). The median (IQR) follow-up period was 35 weeks (27–50).
The cohorts analyzed (INER and HMF) were different in terms of the proportion of patients who smoked (33.3% vs 66.6%, P<.011) and in the presence of anti-Ro/SS-A antibody (4.55% vs 47.62%, P<.001), of Raynaud's phenomenon (6.67% vs 33.33%, P<.005), of xerophthalmia (15.56% vs 42.86%, P<.016), of highly specific manifestations of CTD (31.11% vs 71.43%, P<.002) and of HRCT findings inconsistent with UIP (64.44% vs 85% [14.29], P<.001), respectively (Table 2).
Cohort of Patients With Interstitial Lung Disease Associated With Undifferentiated Connective Tissue Disease, HMF and INER. Description of the Demographic, Clinical, Immunology Laboratory and Imaging Characteristics. Comparison Between the Two Cohorts.
| INER (n=45) | HMF (n=21) | Total (n=66) | |
|---|---|---|---|
| Demographic characteristics | |||
| Men | 17 (37.78) | 4 (19.05) | 21 (31.82) |
| Age at diagnosis | 57.37 (12.20) | 58.23 (14.61) | 57.65 (12.91) |
| Smoking behaviora | 15 (33.33) | 14 (66.67) | 29 (43.94) |
| Immunology laboratory | |||
| ANA positive | 37 (84.09) | 20 (95.24) | 57 (87.69) |
| RF positive | 20 (48.78) | 9 (42.86) | 29 (46.77) |
| High ANA titer | 17 (37.78) | 12 (57.14) | 29 (43.94) |
| Specific ANA pattern | 9 (25) | 7 (35) | 16 (28.57) |
| Clinical characteristics | |||
| Raynaud's phenomenona | 3 (6.67) | 7 (33.33) | 10 (15.15) |
| Xerophthalmiaa | 7 (15.56) | 9 (42.86) | 16 (24.24) |
| Xerostomía | 15 (33.33) | 12 (57.14) | 27 (40.91) |
| Arthritis | 6 (13.23) | 6 (28.57) | 12 (18.18) |
| Arthralgia | 12 (26.67) | 6 (28.57) | 18 (27.27) |
| Morning stiffness | 4 (8. 89) | 0 | 4 (6.06) |
| GER symptoms | 13 (28.89) | 7 (33.33) | 20 (30.3) |
| Weight loss | 19 (42.22) | 6 (28.57) | 25 (37.88) |
| Photosensitivity | 1 (2.22) | 1 (4.76) | 2 (3.03) |
| Dysphagia | 2 (4.44) | 0 | 2 (3.03) |
| Recurrent unexplained fever | 5 (11.11) | 1 (4.76) | 6 (9.09) |
| Proximal muscle weakness | 0 | 2 (9.52) | 2 (3.03) |
| Alopecia | 0 | 0 | 0 |
| Manifestations highly specific for CTDa | 14 (31.11) | 15 (71.94) | 29 (43.94) |
| Baseline respiratory function test | |||
| FVC (predicted %) | 60.61 (19.5) | 64.4 (19) | 61.86 (19.3) |
| DLCO (predicted %) | 44.36 (23.6) | 45.85 (18.7) | 44.94 (21.6) |
| HRCT pattern | |||
| Typical UIP pattern | 6 (13.33) | 3 (14.29) | 9 (13.64) |
| Pattern inconsistent with UIPa | 29 (64.44) | 3 (14.29) | 32 (48.48) |
ANA, antinuclear antibodies; CTD, connective tissue disease; DLCO, diffusing capacity of the lung for carbon monoxide; FVC, forced vital capacity; GER, gastroesophageal reflux; HMF, Hospital María Ferrer; HRCT, high-resolution computed tomography; INER, National Institute of Respiratory Diseases Ismael Cosio Villegas; RF, rheumatoid factor; SD, standard deviation; UIP, usual interstitial pneumonia.
Data expressed as n (%) or mean (SD).
The most common clinical manifestations were xerostomia (40.9%), weight loss (38%) and symptoms of gastroesophageal reflux (30.3%).
The most widespread serological finding was the presence of ANA (87.69%) at a titer higher than 1:320 in 44% of the cases. The fine speckled pattern was that most frequently observed in IIF (48.12%). Anti-Ro/SS-A antibody was tested in 43 patients, and was positive in 11 (25.2%), whereas anti-Jo-1 antibody was positive in 7 (23.3%) of the 30 participants in whom it was requested. All of the individuals tested for anti-Scl-70 and anti-U1-RNP antibodies were negative. Surgical biopsy was performed in 15 patients (22.7%). The definitive diagnosis was UIP in 7 of them, but diffuse lymphoid follicles were found in 3. In 7 cases, the diagnosis was NSIP (in 3 combined with features of UIP and in 2 with OP). Three biopsies were defined as “unclassifiable”. The histological findings were involvement of arterioles in 5 biopsies, follicular bronchiolitis in 2 and diffuse lymphoid follicles in 9. In no case was there pleural involvement.
With regard for therapy, only 47 patients received a specific drug (an immunosuppressive or antifibrotic agent). The treatments most widely utilized were azathioprine in 23 (48.94%), mycophenolate mofetil in 14 (29.79%), methotrexate in 3 (6.38%), steroids alone in 3 (6.38%), cyclophosphamide in 2 (4.26%) and pirfenidone in 2 (4.26%).
Defining Patterns. Univariate and Multivariate AnalysisIn the univariate analysis, the patients with manifestations that were “highly specific for CTD” were younger (mean 52 years [SD 14.58] vs 62 years [9.46]; [P<.01]) and the proportion of men was lower (10.34% vs 48.65%; P<.01). Although we observed no differences in the baseline FVC% and DLCO%, the individuals with manifestations that were “highly specific for CTD” had a more favorable course in terms of the respiratory function test. The change in the median (IQR) of FVC% over time was 1 (−1 to 10) in the patients with manifestations that were “highly specific for CTD” vs −6 points (−16 to −4) in those in whom these manifestations were not encountered (P<.01) (Table 3). It is important to clarify the fact that both groups (with and without manifestations that were “highly specific for CTD”) had similar median (IQR) follow-up periods (34 weeks [27–56] vs 36 weeks [27–50]; P=.758).
Cohort of Patients With Interstitial Lung Disease Associated With Undifferentiated Connective Tissue Disease, HMF and INER. Comparison Between Patients With and Without Manifestations “Highly Specific for Connective Tissue Disease”.
| UCTD with manifestations highly specific for CTD (n=29) | UCTD without manifestations highly specific for CTD (n=37) | P | |
|---|---|---|---|
| Men | 3 (10.34) | 18 (48.65) | <.01 |
| Age | 52 (14.58) | 62.08 (9.46) | <.01 |
| Typical UIP pattern on HRCT | 3 (10.34) | 6 (16.22) | .72 |
| Pattern on HRCT inconsistent with UIP | 14 (48.28) | 18 (48.65) | .97 |
| Baseline FVC (predicted %) | 58 (19.78) | 64.97 (18.66) | .15 |
| Baseline DLCO (predicted %) | 43 (19.02) | 46.38 (23.60) | .57 |
| Difference between final and baseline FVC (predicted %) | 1 (− 1 to 10) | − 6 (− 16 to − 4) | <.01 |
| Follow-up period in weeks | 34 (27 to 56) | 36 (27 to 50) | .76 |
CTD, connective tissue disease; DLCO, diffusing capacity of the lung for carbon monoxide; FVC, forced vital capacity; HMF, Hospital María Ferrer; HRCT, high-resolution computed tomography; INER, National Institute of Respiratory Diseases Ismael Cosio Villegas; IQR, interquartile range; SD, standard deviation; UCTD, undifferentiated connective tissue disease UIP, usual interstitial pneumonia.
Data expressed as n (%), mean (SD) or median (IQR).
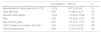
The presence or absence of high ANA titers or with a specific pattern was not associated with differences in terms of sex, age, frequency of manifestations that were “highly specific for CTD”, functional data or that provided by HRCT. In the multiple logistic regression analysis using HRCT pattern inconsistent with UIP as a dependent variable, age under 60years was the only variable that showed a statistically significant association, with an OR (95%CI) of 11.53 (2.7–47.69) (Table 4). In the multivariate analysis employing multiple linear regression, the presence of manifestations that were “highly specific for CTD” was associated with an improvement in FVC% values, with a β coefficient of 13.25 (95%CI, 2.41–24.09), this being the only independent variable to show a statistically significant association (Table 5).
Cohort of Patients With Interstitial Lung Disease Associated With Undifferentiated Connective Tissue Disease, HMF and INER. Multiple Logistic Regression Analysis With High-Resolution Computed Tomography Pattern Inconsistent With Usual Interstitial Pneumonia as Dependent Variable.
| OR (95% CI) | P | |
|---|---|---|
| Manifestations “highly specific for CTD” | 0.35 (0.08–1.46) | .15 |
| High ANA titer | 0.93 (0.24–3.59) | .93 |
| Specific ANA pattern | 0.82 (0.18–3.64) | .80 |
| Men | 0.90 (0.18–4.43) | .90 |
| Age under 60 years | 11.53 (2.79–47.69) | <.01 |
ANA, antinuclear antibodies; CI, confidence interval; CTD, connective tissue disease; HMF, Hospital María Ferrer; INER, National Institute of Respiratory Diseases Ismael Cosio Villegas; OR, odds ratio.
Cohort of Patients With Interstitial Lung Disease Associated With Undifferentiated Connective Tissue Disease, HMF and INER. Multiple Linear Regression Analysis With Change in the Forced Vital Capacity (%) as Dependent Variable.
| β Coefficient | 95% CI | P | |
|---|---|---|---|
| Manifestations “highly specific for CTD” | 13.25 | 2.41 to 24.09 | .01 |
| High ANA titer | 2.94 | −8.49 to 14.37 | .59 |
| Specific ANA pattern | −2.06 | −17.06 to 12.86 | .77 |
| Men | 1.48 | −10.34 to 17.27 | .79 |
| Age over 60 years | 3.57 | −10.12 to 17.27 | .59 |
| HRCT pattern inconsistent with UIP | 1.56 | −9.10 to 12.23 | .82 |
| Received treatment | 3.65 | −7.47 to 14.79 | .49 |
ANA, antinuclear antibodies; CI, confidence interval; CTD, connective tissue disease; HMF, Hospital María Ferrer; HRCT, high-resolution computed tomography; INER, National Institute of Respiratory Diseases Ismael Cosio Villegas; UIP, usual interstitial pneumonia.
In this report, we found that the presence of at least 1 manifestation that was “highly specific for CTD” (Raynaud's phenomenon, xerophthalmia or arthritis) was associated with a higher prevalence of women, lower age at onset and a more favorable course in terms of changes in FVC% over time, which was confirmed after adjusting for potential confounders. This profile differs from that classically observed in patients with IPF, a disease in which there is a predominance of men, advanced age and rapid functional deterioration.12 One datum to point out with respect to our results is the fact that there were significant clinical and radiological differences between the cohorts. Although we do not have a definitive explanation for this finding, it could be that the differences are related to the moment at which the patients are evaluated (during a hospital stay in the INER and in the outpatient clinic in HMF).
During the baseline evaluation of a patient with ILD, the presence of clinical manifestations related to a CTD or a positive test for autoantibodies represents a dilemma for a physician, who should decide whether to consider the patient a carrier of idiopathic ILD (IPF) and utilize antifibrotic agents, or consider the case of a ILD associated with a CTD and administer immunosuppressive therapy.19,20 The detection of clinical manifestations that can contribute to the differentiation of these phenotypes appears to be a relevant finding.
Our results support the proposals of other authors in terms of the impact of clinical manifestations on the course of this group of patients.5 The intersociety consensus recently published includes proposals for new classification criteria (not yet validated) in which the clinical manifestations occupy a specific domain (together with a serological and a morphological domain).11 This consensus eliminates certain clinical manifestations included in previous criteria (for example, symptoms of gastroesophageal reflux, weight loss) and includes others with greater specificity, such as Raynaud's phenomenon and arthritis. The patients who meet the proposed criteria and do not satisfy those of a defined CTD have an “interstitial lung disease with autoimmune features”. We believe that the objective of the results of our study are along the lines of that proposed in this consensus, in the attempt to exclude highly sensitive manifestations that can mean the erroneous inclusion of individuals with IPF in the group of patients with ILD associated with CTD.
With respect to the serological data, neither the presence of high ANA titers nor the specific patterns according to IIF were helpful in differentiating between the groups presented in the hypothesis of this study. This contrasts with findings reported by other groups, which stress the role of the detection of autoantibodies in the evaluation of these patients.4,21 We consider that the information provided by the immunology laboratory may be useful, although we know that it can lead to false positives and negatives (even more so in the use of techniques like IIF that depend on the observer) and should be interpreted in accordance with the clinical setting in which it is obtained.
In a recent article that involved patients with a diagnosis of “interstitial lung disease with autoimmune features” according to the abovementioned consensus,11 it was observed that survival was better in those with a pattern not specific for UIP. The authors stressed the importance of the tomographic and histological pattern.22 In our study, the HRCT pattern did not differ among the subgroups evaluated. We found no association with a better functional outcome when a “pattern inconsistent with UIP” was included as a covariate in the multivariate analysis of the change in FVC over time. We point out the low prevalence in our cohort of the typical pattern of UIP according to HRCT findings in comparison with other reports.4,22,23 It could be that there has been a decrease in the strength of the study for detecting differences in the HRCT pattern when compared to the clinical manifestations, immunology laboratory and functional outcome. Our cohort came from 2 centers specialized in respiratory diseases, with physicians who have extensive experience in the evaluation of patients with ILD and numbers of patients similar to those of other cohorts previously reported. Thus, we consider that our findings are representative and comparable to those of other articles.
Our study has certain limitations. The patients were included on the basis of the medical records documented during hospital stays in one center (INER) and from an outpatient clinic in the other (HMF). This may constitute an important difference regarding the severity of the cases in the 2 centers, which implies possible selection bias. On the other hand, as this is a retrospective study with data taken directly from the medical records, the examination concerning the symptoms linked to CTD was not standardized, leading to possible information bias. The study also has limitations with respect to the evaluation of the features of autoimmune disease. The clinical and serological variables taken into account were those proposed in the Kinder criteria. Thus, they exclude manifestations and serological findings specific for CTD, such as mechanic's hands, palmar telangiectasias, Gottron's papules, antisynthetase antibodies other than Jo-1 or anti-cyclic citrullinated peptide antibodies. Many of these variables are now incorporated into the latest intersociety consensus and are valuable in the identification of patients with UCTD.11 Again, we did not analyze the role of capillaroscopy or minor salivary gland biopsy in the evaluation of patients with ILD associated with UCTD, as they are not included in the diagnostic criteria utilized.24,25 Finally, to evaluate the functional outcome, we chose to study the change in FVC% over time, in the knowledge that it is not the best method in patients who have different follow-up periods. The analysis of the time to event would have been a more accurate approach, but we did not have access to the data necessary to carry it out. While we consider that our study provides useful information, and that it is in keeping with the latest intersociety consensus, we believe that there is a need for prospective studies that evaluate survival and involve a larger number of patients to respond more conclusively to the question being proposed.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingThe present report has not received any type of funding.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Andrea, Werbach.
Please cite this article as: Alberti ML, Paulin F, Toledo HM, Fernández ME, Caro FM, Rojas-Serrano J, et al. Enfermedad indiferenciada del tejido conectivo y enfermedad pulmonar intersticial: intentando definir patrones. Reumatol Clin. 2018;14:75–80.