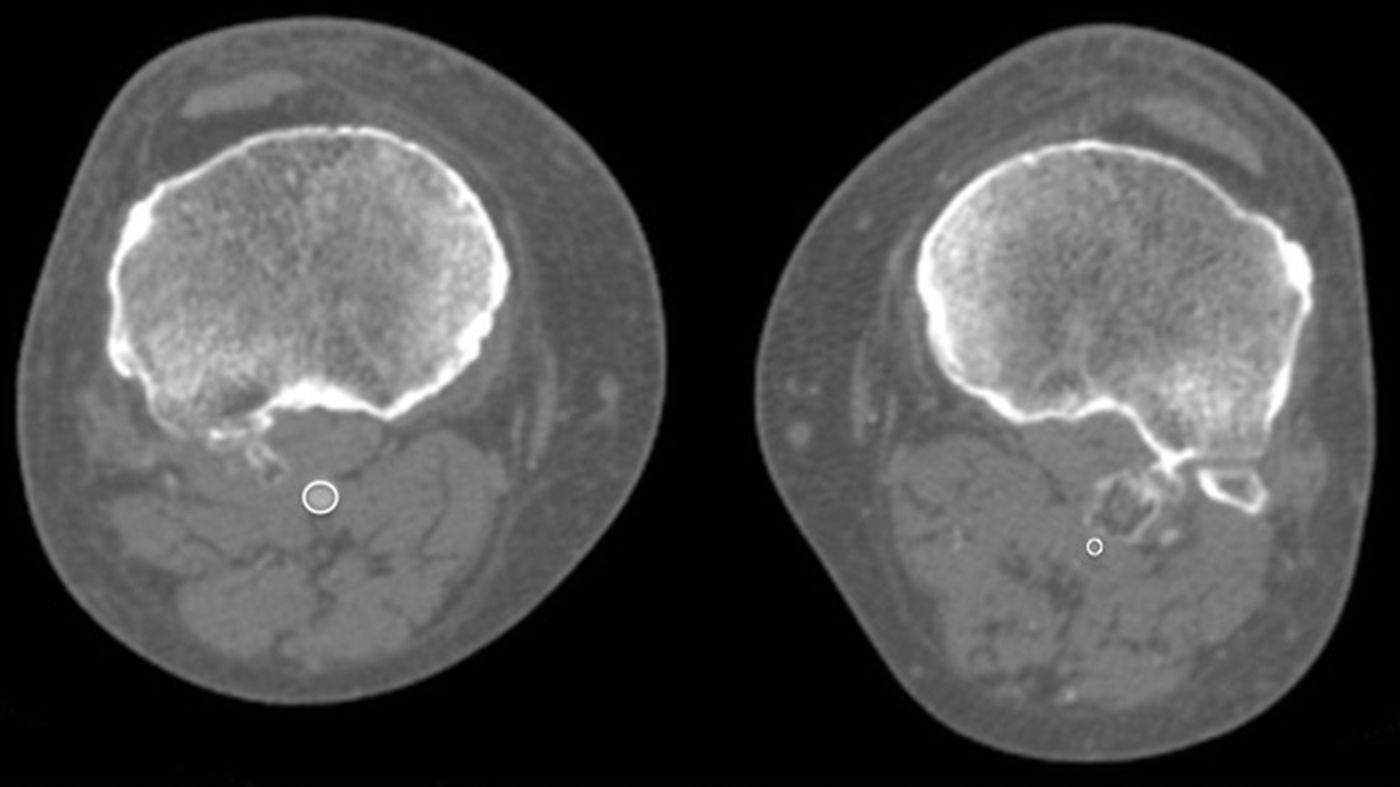
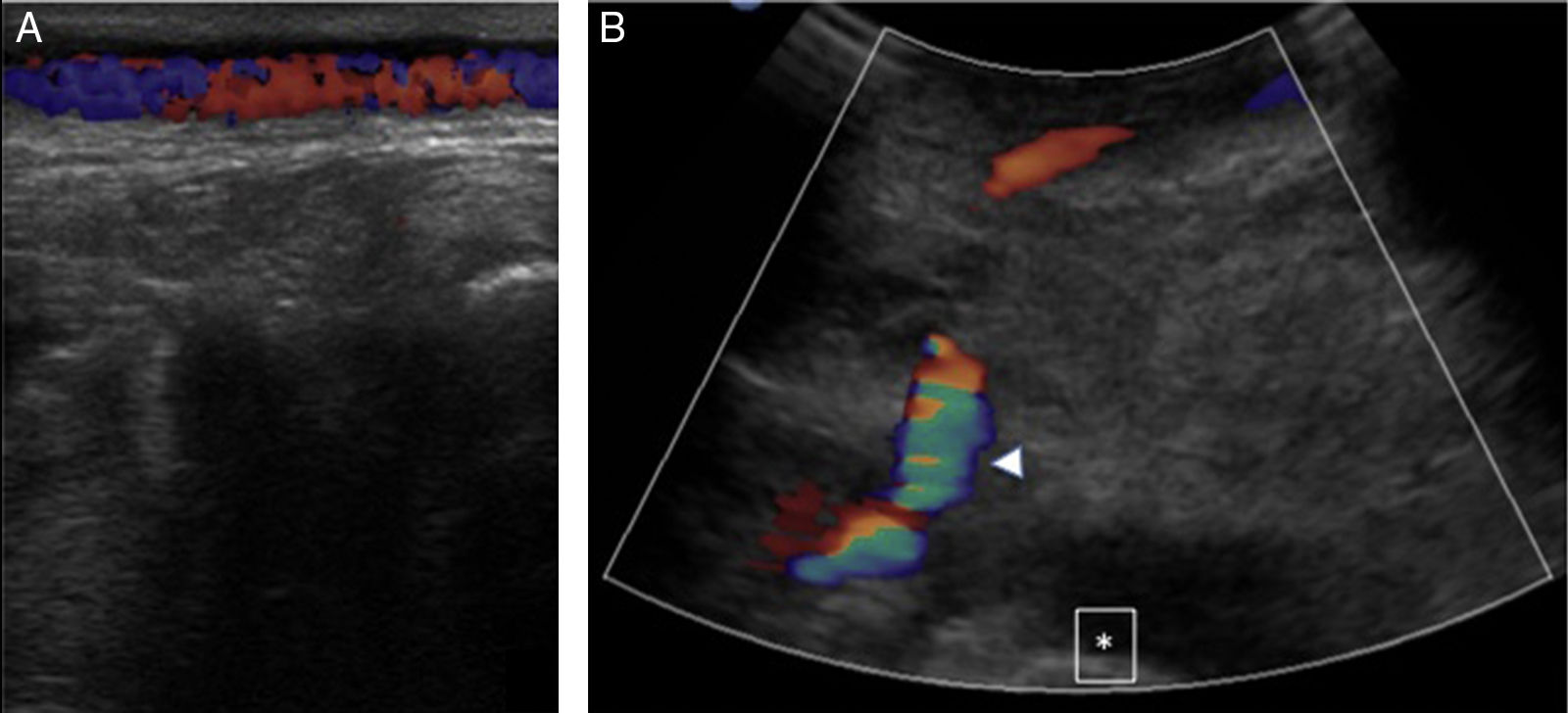
A male, 67 years of age, obese, with high blood pressure and dyslipidemia presented at the emergency department due to pain, cold and functional impairment of his lower left limb of 24-h onset. During anamnesis, the patient stated he had had a chronic intermittent pain in his left knee for a long time. A previous simple knee X-ray showed an osteochondroma (Fig. 1). The patient presented with a femoral pulse but with no popliteal and distal pulses. Artery examination was normal in the contralateral extremity. A CT angiogram was requested for the lower limbs which showed thrombosis of the popliteal artery adjacent to the osteochondroma (Figs. 2 and 3). We decided to perform in situ revascularization with femoro-popliteal saphenous vein graft (Fig. 4) avoiding the tunneling technique for anatomical positioning. To date, after 3 years of follow-up with eco-Doppler, the bypass continues maintaining permeability with ankle-arm index of 0.9, and no signs of popliteal vein injury.
Osteochondroma is the most common pseudotumoral bone lesion. The radiologic pathognomonic characteristic of this tumor is the cortical and medullar continuity of the lesions with the bone from which they protrude.1 They may be single or multiple.2 Some of the most common complications are the presence of bone deformity, fractures,1 vascular compromise3 and neurological compromise,4 formation of a bursa5 and malignant degeneration.6 Diagnosis may be made with an X-ray, although other imaging methods such as a scan, CT and MR may be used in suspected cases when symptoms occur or are in unusual locations.1 Vascular compromise may be caused by displacement of blood vessels (arteries and veins), by stenosis, occlusion and the formation of pseudoaneurisms, with the latter being more frequent at knee level,7 involving the popliteal artery or being presented as arterial thrombosis,8,9 as in this clinical case. Its presentation as thoracic outlet syndrome in the case of rib lesions has been described.10
Familiarity with the spectrum of radiological findings leads to an accurate diagnosis which is helpful in managing the patient toward appropriate treatment.
Ethical LiabilitiesProtection of people and animalsThe authors declare that no experiments using human beings or animals have been carried out for this research study.
Data confidentialityThe authors declare that they have followed the protocols of their center of work on patient data publication.
Right to privacy and informed consentThe authors declare that they obtained the informed consent from the patients and/or subjects referred to in this article.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Alonso-Gómez N, Cuesta-de Diego M, Martínez-Izquierdo A, Sáinz-González F. Complicación clínica inusual: isquemia aguda de miembro inferior causada por osteocondroma tibial. Reumatol Clin. 2019;15:182–184.