Rheumatoid arthritis (RA) is one of the most common causes of AA amyloidosis. Most patients are asymptomatic and only when there are large deposits in certain organs, functional problems arise. We report two patients with amyloidosis secondary to RA, with renal and intestinal involvement, who responded to treatment with etanercept.
La artritis reumatoide (AR) es una de las causas más frecuentes de amiloidosis tipo AA. En la mayoría de los pacientes es asintomática y sólo cuando existen grandes depósitos en determinados órganos ocasiona problemas funcionales. Presentamos 2 pacientes con amiloidosis secundaria a AR, con afectación renal e intestinal, que respondieron al tratamiento con etanercept.
Amyloidosis is characterized by the deposition of an amorphous substance (amyloid) in the extracellular spaces of various organs and tissues conditioning functional and structural alterations. In clinical practice the most common form is secondary, whose deposits contain AA protein, which is associated with infectious and chronic inflammatory processes, such as rheumatoid arthritis (RA). Here we present 2 patients with long standing RA, with an inadequate response to multiple treatments based on immunomodulators and persistence of inflammatory activity, besides presenting secondary amyloidosis, who were treated successfully with etanercept. Anti-TNFα therapy has been used in patients with inflammatory arthritis and secondary amyloidosis.
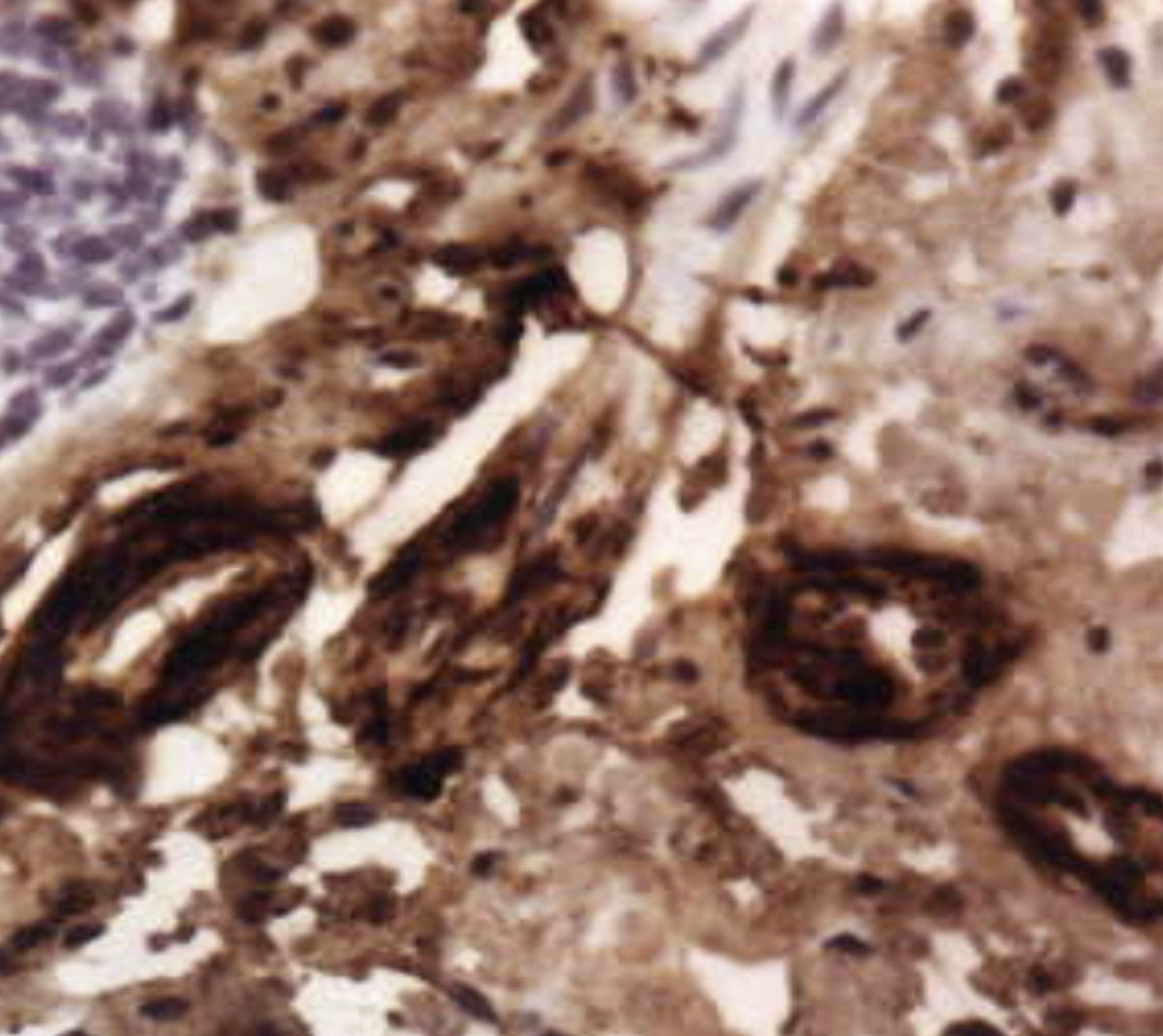
Case Report 1The patient is a 63-year-old with a history of RA of more than 15 years since onset, treated with nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, methotrexate, cyclosporine, sulfasalazine, gold salts, antimalarials and, for 3 years, with leflunomide, with mild to moderate clinical activity. Other important history includes hypertension and dyslipidemia, obstructive sleep apnea, coronary heart disease, multifactorial interstitial lung disease for 5 years and controlled through periodic respiratory function tests and radiological journals and treated with bronchodilators, and finally, a history of past infection by Pneumocystis jiroveci treated with prophylactic trimethoprim-sulfamethoxazole. At the end of 2008 the patient was admitted due to nephrotic syndrome and, on physical examination, the patient presented: 100.7kg, regular general state, eupneic at rest, 96% saturation, cushingoid aspect, blood pressure of 130/70mmHg and 37°C, normal cardiopulmonary auscultation, globular, soft and palpable abdomen, pitting edema up to the thighs, abdomen and hands, bilateral arthritis of the metacarpophalangeal joints and limitation of flexion and extension in both wrists; deformity of both ankles and feet. Among additional examinations we observed normochromic normocytic anemia, erythrocyte sedimentation rate (ESR) of 130mm/1sth, fibrinogen reactive urea of 112mg/dl, creatinine 3.8mg/dl, creatinine clearance 45, 4ml/min, uric acid of 8.2mg/dl, total protein 4.5g/dl C-reactive protein of 10.9mg/dl, serum protein fractions with increased alpha 1, alpha 2, and decreased beta globulins, gamma globulin, albumin of 1.5g/dl and the urinalysis detected proteinuria, microhematuria and abundant hyaline and granular casts, more than 11g of protein in 24h urine. The serology for hepatitis viruses B and C and HIV and Mantoux was negative. Echocardiography was normal and chest X-ray revealed signs of hyperinflation with images of predominantly peripheral cortical and basal fibrosis and advanced erosive involvement on radiographs of hands and feet. The patient underwent a renal biopsy with findings consistent with AA amyloidosis (Fig. 1). Among the therapeutic possibilities used were high-dose glucocorticoids and cyclophosphamide, but given the patient's clinical condition and medical history, the decision was made to start treatment and intravenous albumin depletion, associated to biologic therapy (etanercept 50mg weekly) and low-dose glucocorticoids. Since the patient had dyslipidemia and hypertension, statin treatment was continued, replacing calcium antagonists with antagonists of angiotensin II receptors. At 4 weeks after the initiation of etanercept, a decrease in proteinuria of more than 50% (5g in 24h) was seen and now, after more than a year of treatment, the patient is in clinical remission from the joint point of view and maintains normal renal function with creatinine of 1.5mg/dl and residual proteinuria of less than 1g in 24h.
Renal biopsy: there is extracellular deposition of a homogeneous filamentous PAS+ acellular, Congo red+ material, with an eosinophilic glaze histological appearance described as “amyloid”. The Congo red-stained kidney is seen as a homogeneous substance amyloid tinged with a reddish-orange color that appeared as renal interstitial thickening and obliterating the glomerular capillary lumens, replacing the glomerulus (200×).
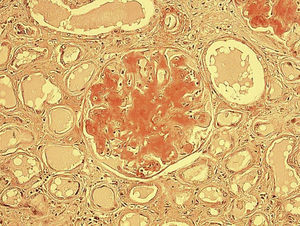
We report the case of a 68-year-old woman with a history of RA of 20 years since onset, treated with NSAIDs, low doses of corticosteroids (5mg per day of prednisone), methotrexate and leflunomide; prosthetic hip and bilateral knee surgeries, hypertension, myelodysplastic syndrome treated with erythropoietin and mild chronic renal failure. She presented diarrhea for 8 weeks, weight loss of 20kg and edema in the lower limbs. On physical examination: weight 45kg, regular general condition, blood pressure of 110/60mmHg and a temperature of 36°C, normal cardiopulmonary auscultation, abdominal tenderness and palpable, pitting edema of the legs and hands. Musculoskeletal: arthritis of bilateral metacarpophalangeal and limitation of flexion and extension of both wrists. Laboratory analysis highlighted normochromic normocytic anemia, ESR of 110mm/1sth, urea 46mg/dl, creatinine of 1.3mg/dl, normal urinalysis, 24h urine protein negative, serum protein with increased alpha 1, alpha 2, beta and gamma globulin fractions and decreased albumin. The serology of hepatitis B and C virus, and Booster Mantoux was negative. She underwent a complete digestive study (ultrasound, endoscopy, oral barium examination, and stool cultures), the results were normal, and colonoscopy was performed with biopsy of the colon, with findings consistent with AA amyloid deposition (Fig. 2). Symptomatic treatment was initiated with diuretics and intravenous albumin. Given the history of myelodysplastic syndrome, cyclophosphamide therapy was suspended due to the possibility of bone marrow toxicity and, due to the existence of active joint activity; we decided to initiate biological therapy with etanercept (50mg weekly) associated with low-dose oral corticosteroids. Currently, after 6 months of treatment, the patient is virtually asymptomatic from the joint and digestive standpoints, with disappearance of diarrhea and presenting normal analytical controls.
DiscussionRA is one of the most common causes of AA amyloidosis. In a study of 121 patients with RA who underwent abdominal fat aspirate, there was a prevalence of amyloid deposits of up to 29%, related to longer duration of disease and the introduction of treatment with immunomodulating drugs.1 Most amyloidosis patients are asymptomatic and only when there are large deposits in certain organs, does it lead to specific functional problems: thus, in the renal there is progressive proteinuria, microhematuria or a severe decrease in renal function, the deposits will cause gastrointestinal bleeding or malabsorption, location in small vessels can cause neuropathy or ischemic events and restrictive cardiac dysfunction or conduction disturbances, which may result from amyloid deposits in the myocardium or pericardium. The easiest way to confirm the diagnosis is by abdominal subcutaneous fat, gingiva or rectal biopsies, with Congo red staining and showing the typical yellow and green birefringence under polarized light microscopy. AA amyloidosis is a disease with high morbidity and mortality due to end stage renal disease, infectious processes, heart failure, intestinal perforation, or digestive hemorrhage.2 Poor prognostic factors are decrease in albumin and serum creatinine and proteinuria higher in urine of 24h.3 It may lead to terminal renal failure, especially in patients whose serum amyloid A levels are found persistently above 10mg/l.4 That is why the primary treatment of this entity is the correct treatment of the underlying inflammatory process (either with cytostatic agents in RA or antibiotics in chronic infections), which can result in the stabilization and improvement in renal function as well as reducing urinary protein excretion and the partial resolution of amyloid deposits. There is no specific treatment to dissolve amyloid deposits and prevent them from accumulating in tissues, but it is estimated that in addition to symptomatic treatment, it is necessary to strictly control the activity of the rheumatic inflammatory process, with consequent reduced formation of acute phase protein and the reduction of amyloid deposits. Treatments that have been shown to be effective are azathioprine, methotrexate, cyclophosphamide, chlorambucil, and colchicine (especially in the treatment of familial Mediterranean fever and in preventing the development of amyloidosis in this disease).5 In the two cases presented, we decided not to start cyclophosphamide, because of possible drug toxicity, in terms of myelosuppression and infection, in addition, the clinical response, both of joint and target organs affected in each case, may have been slower and lower than with other recently tested therapeutic alternatives. Thus, in recent years it has been suggested that blocking TNF may reduce proteinuria and improve renal function in renal amyloidosis secondary to RA.6 We used the 3 anti-TNF drugs currently available, either as monotherapy or in combination with methotrexate7 showing, in repeated biopsies of gastroduodenal mucosa, a significant reduction of amyloid deposits after initiation of biologic treatment.8 There are several studies of treatment with etanercept, aimed at decreasing proteinuria, maintenance and even improvement of renal function and disappearance of malabsorption due to decreased amyloid deposits.9,10 Other studies have found that both the duration of amyloidosis as well as the level of proteinuria were independent predictors of treatment failure with anti-TNF and that proteinuria was critical as a predictor of mortality, and infections were more common in patients treated with biologic11 therapy. We must not forget that although this new therapy directed against TNF therapy has opened new expectations in these patients, it can have significant side effects (infections, myelotoxicity) and, since clinical evidence is still scarce, we must be cautious in deciding the initiation of these treatments, assessing the benefits and the risks in the individual patient. In conclusion, experience in recent years using anti-TNF treatments in different inflammatory rheumatic diseases makes us consider this therapy as a reasonable option in secondary amyloidosis, although more long-term monitoring studies are needed.
Please cite this article as: Macías Fernández I, et al. Uso de etanercept en amiloidosis secundarias a artritis reumatoide: a propósito de dos casos. Reumatol Clin. 2011;7(6):397–400.