The purpose of the present study is to identify the extent to which it affects clinical decisions in a single-centre observational retrospective study.
MethodThe results of 801 requests and 1174 consecutive individual ultrasound examinations performed over 10 months were analysed.
ResultsThe most frequent indication was diagnostic assistance (39%) followed by assessment of inflammatory activity (34%). By topography, the hand was the most frequently studied region (51%), followed by the foot (18.1%). Of all requests, 67% had an impact on decision-making. The impact on clinical decision-making was associated with a shorter waiting time for the evaluation of the results, being the greatest in those ultrasound scans performed on demand on the same day of the request. In 73% of bilateral ultrasound studies, findings in one of the joints exemplified the overall result reported.
ConclusionsRheumatological musculoskeletal ultrasound has proven to be a useful decision-making technique, the greater the impact of which is seen the shorter the waiting time before it is performed.
El propósito del presente estudio es identificar en qué medida afecta a las decisiones clínicas mediante un estudio unicéntrico observacional retrospectivo.
MétodoSe analizaron los resultados de 801 solicitudes y 1174 ecografías individuales consecutivas realizadas a lo largo de 10 meses.
ResultadosLa indicación más frecuente fue la asistencia diagnóstica (39%) seguida de la evaluación de actividad inflamatoria (34%). Por topografía, la mano fue la región más estudiada (51%), seguida del pie (18,1%). De todas las solicitudes, en 67% se constató un impacto en la toma de decisiones. El impacto en la decisión clínica se asoció a un menor tiempo de espera hasta la evaluación de los resultados, siendo el mayor en aquellas ecografías realizadas a demanda el mismo día de su petición. En 73% de los estudios ecográficos bilaterales, los hallazgos en una de las articulaciones ejemplificaban el resultado global emitido.
ConclusionesLa ecografía reumatológica demuestra ser una técnica útil en la toma de decisiones, cuyo mayor impacto se constata cuanto menor es el tiempo de espera hasta la evaluación de los resultados.
Rheumatologic ultrasound (RU) scans have proved to be an accessible and useful technique for the diagnosis and monitoring of multiple pathologies in the field of this specialty.1 Their application to inflammatory arthropathies has spread rapidly in the last 25 years and has recently been incorporated into other areas of the specialty such as the study of large vessels (LV2 and pulmonary interstitium (PI3 and salivary gland involvement (SG).4
In our setting, training experience in RU has been positively valued, and at the national level it is considered that its use has significantly improved the competence and clinical practice of 71.7% of rheumatologists trained in this technique.5 Likewise, in the management of acute rheumatological pathologies in other settings, ultrasound has been demonstrated to have had an impact on the patient's perceived experience.6
The purpose of this study is to assess the impact of the use of RU on clinical decision-making and to detect areas for improvement, a field in which there is less documented scientific experience.
MethodsA retrospective observational study was designed at a medical centre with 3 scheduled weekly ultrasound appointments and an additional weekly agenda for ultrasound studies and unscheduled procedures. All ultrasound studies were run by, or under the supervision of, 2 rheumatologists who were experts in RU.
We included all records of studies conducted between March and December 2022, both scheduled and on-demand, with the exception of those conducted in the context of other protocolised studies.
From the electronic medical records, data was collected relating to waiting times, indication of the test, concordance of the result with clinical suspicion and impact of the result on the decision made at the surgery visit. The impact on clinical behaviour was considered positive only if involvement of the ultrasound result in decision-making was explicitly noted in the medical record.
In this study, no patients were interviewed nor were any procedures performed. For the review of medical records, the approval of our scientific research ethics committee was obtained.
ResultsA total of 801 RE requests were analysed. Of these, 355 requested the assessment of more than one anatomical region (excluding GS, GV, IP). The number of individual ultrasound scans analysed was 1,174, of which 165 were run on demand (14%).
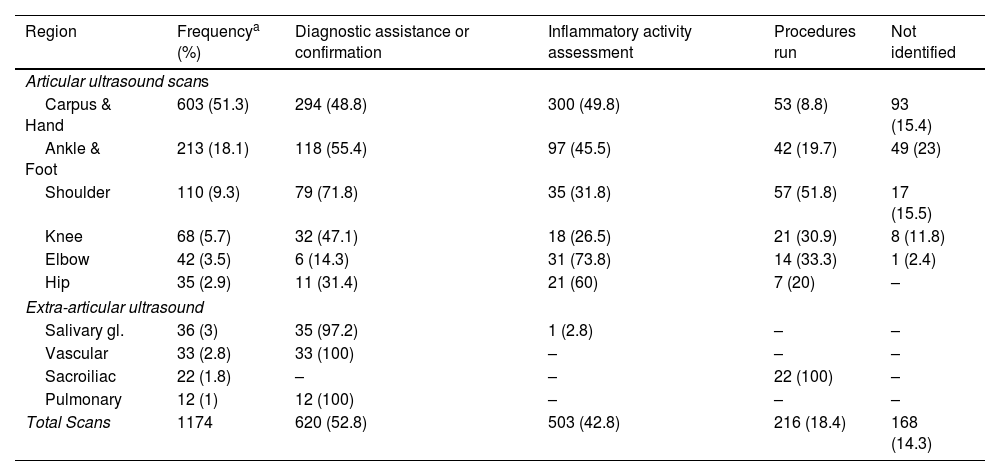
The indications for RU were: diagnostic assistance or confirmation (456, 39%), evaluation of inflammatory activity (398, 34%), performance of procedures (304, 26%) and unidentified, or no identified indication (168, 14%). Table 1 summarises the topographic distribution of the studies carried out and the purposes of the indications.
Topographic distribution of requests for ultrasound studies and purpose or reason for indication.
| Region | Frequencya (%) | Diagnostic assistance or confirmation | Inflammatory activity assessment | Procedures run | Not identified |
|---|---|---|---|---|---|
| Articular ultrasound scans | |||||
| Carpus & Hand | 603 (51.3) | 294 (48.8) | 300 (49.8) | 53 (8.8) | 93 (15.4) |
| Ankle & Foot | 213 (18.1) | 118 (55.4) | 97 (45.5) | 42 (19.7) | 49 (23) |
| Shoulder | 110 (9.3) | 79 (71.8) | 35 (31.8) | 57 (51.8) | 17 (15.5) |
| Knee | 68 (5.7) | 32 (47.1) | 18 (26.5) | 21 (30.9) | 8 (11.8) |
| Elbow | 42 (3.5) | 6 (14.3) | 31 (73.8) | 14 (33.3) | 1 (2.4) |
| Hip | 35 (2.9) | 11 (31.4) | 21 (60) | 7 (20) | – |
| Extra-articular ultrasound | |||||
| Salivary gl. | 36 (3) | 35 (97.2) | 1 (2.8) | – | – |
| Vascular | 33 (2.8) | 33 (100) | – | – | – |
| Sacroiliac | 22 (1.8) | – | – | 22 (100) | – |
| Pulmonary | 12 (1) | 12 (100) | – | – | – |
| Total Scans | 1174 | 620 (52.8) | 503 (42.8) | 216 (18.4) | 168 (14.3) |
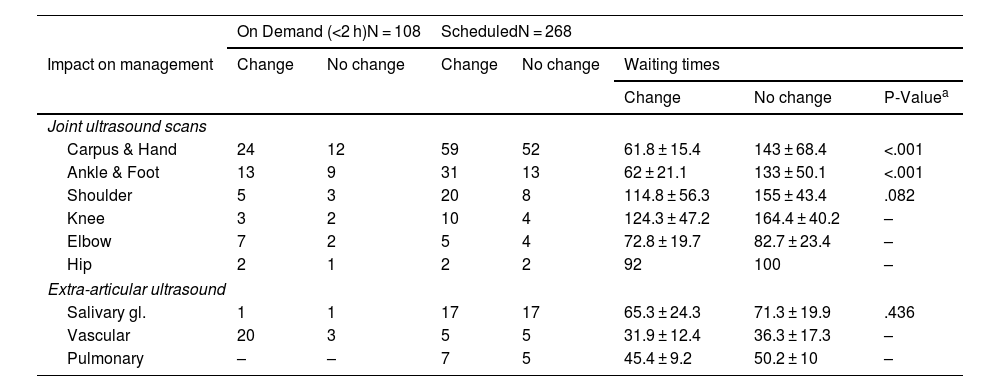
In 376 of the 456 diagnostic studies (diagnostic assistance or confirmation), the original clinical suspicion was confirmed (82%). In 109 of them, with diagnostic confirmation between only two possibilities (e.g., osteoarthritis vs. psoriatic arthritis), the ultrasound study coincided with the clinical diagnostic presumption in 97 cases and there were discrepancies in 12 (good agreement; kappa = 0.748). In 266 of the studies evaluating inflammatory activity, a change in clinical behaviour was found (67%). In the group of diagnostic studies, 108 were conducted on demand, on the same day of the application, and 268 were scheduled. The proportion of changes in management after ultrasound results was found in 75 on-demand scans (69.4%) and 156 scheduled scans (58.2%) (p = .042). Table 2 shows the waiting times and the impact of the outcome on decision-making. Overall, the mean waiting time for scans that gave rise to a change in the clinical decision was shorter than for those that did not. This difference was statistically significant in the carpus and hand (61.8 ± 15.4 vs. 143.4 ± 68.4 days, p < .001) and ankle and foot (62 ± 21.1 vs. 133 ± 50.1 days, p < .001 studies).
Distribution of the impact of the ultrasound result on clinicians’ conduct, depending on the type of ultrasound requested (on-demand or scheduled).
| On Demand (<2 h)N = 108 | ScheduledN = 268 | ||||||
|---|---|---|---|---|---|---|---|
| Impact on management | Change | No change | Change | No change | Waiting times | ||
| Change | No change | P-Valuea | |||||
| Joint ultrasound scans | |||||||
| Carpus & Hand | 24 | 12 | 59 | 52 | 61.8 ± 15.4 | 143 ± 68.4 | <.001 |
| Ankle & Foot | 13 | 9 | 31 | 13 | 62 ± 21.1 | 133 ± 50.1 | <.001 |
| Shoulder | 5 | 3 | 20 | 8 | 114.8 ± 56.3 | 155 ± 43.4 | .082 |
| Knee | 3 | 2 | 10 | 4 | 124.3 ± 47.2 | 164.4 ± 40.2 | – |
| Elbow | 7 | 2 | 5 | 4 | 72.8 ± 19.7 | 82.7 ± 23.4 | – |
| Hip | 2 | 1 | 2 | 2 | 92 | 100 | – |
| Extra-articular ultrasound | |||||||
| Salivary gl. | 1 | 1 | 17 | 17 | 65.3 ± 24.3 | 71.3 ± 19.9 | .436 |
| Vascular | 20 | 3 | 5 | 5 | 31.9 ± 12.4 | 36.3 ± 17.3 | – |
| Pulmonary | – | – | 7 | 5 | 45.4 ± 9.2 | 50.2 ± 10 | – |
In the group of scheduled studies, the waiting time for outcome assessment is distinguished according to the impact on clinical behaviour.
Of the 355 studies with a request for more than one region, 325 were bilateral studies (hands, 293, 82.5%). A review of the observed findings identified that in 261 studies (73.5%), the findings of a single study (unilateral) provided clinically relevant information.
DiscussionRU contributes to clinical decision-making and endorses the criteria of diagnostic suspicion. In addition, there is a significant demand for ultrasound-guided procedures. On the other hand, we observed that the greatest value of the result of RU is obtained from a rapid assessment, especially those performed at the clinician's request.
The main limitation of our study is its single-centric nature, although, on the other hand, our service has a long school tradition of RU and healthcare practice. The greatest strength lies in the large amount of cases reviewed that provide a varied representation of all ultrasound scans run in clinical practice, excluding those that are carried out in the context of scientific studies.
Based on our observations, long waiting times reduce the clinical usefulness of RUs. In this sense, it would be advisable to consider reducing the indication for bilateral studies, reserving more space for on-demand studies and, most importantly, ensuring training in ultrasound for all medical personnel, also providing more equipment to undertake the scans.
ConclusionRU is proven to be a useful technique in decision-making, thus backing up clinical opinion. The greatest impact on clinical decisions was identified in ultrasound scans with shorter waiting times, especially in hand and foot studies.
FundingNo internal or external funding was received for this study.
Conflict of interestThe authors declare no conflict of interest.