Rheumatoid arthritis (RA) has an indirect effect on body composition. Body mass index (BMI) is not a valid predictor of body fat in RA patients.
ObjectiveTo evaluate the accuracy of BMI in identifying obesity diagnosed according to dual energy X-ray absorptiometry (DXA) in well-controlled RA patients.
MethodsAn observational, cross-sectional, descriptive, analytical study. We used 3 different cutoffs for obesity as determined by DXA: >35% total fat, >40% total fat, and >35% central fat mass (central obesity).
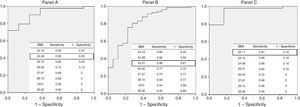
ResultsOne hundred one patients were included. We found that 35% total fat corresponded to a BMI of 24kg/m2, with a sensitivity of 90% and specificity of 75% (area under the curve [AUC] 0.917); 40% total fat to a BMI of 25kg/m2, with a sensitivity of 86% and specificity of 39% (AUC 0.822); and 35% central fat mass to a BMI of 22kg/m2, with a sensitivity of 97% and specificity of 84% (AUC 0.951).
ConclusionObesity according to DXA was underdiagnosed when the classic BMI cutoffs were used in well-controlled RA patients.
La artritis reumatoide (AR) tiene un efecto indirecto en la composición corporal. El índice de masa corporal (IMC) no se considera un predictor válido de la grasa corporal en pacientes con AR.
ObjetivoEvaluar el IMC para identificar la obesidad mediante absorciometría dual por rayos X (DEXA) en pacientes con AR bien controlados.
MétodosEstudio observacional, transversal, descriptivo y analítico. Se utilizaron 3 definiciones de obesidad por DEXA: >35% de grasa total, >40% de grasa total y obesidad central>35%.
ResultadosSe incluyó a 101 pacientes. Se encontró un IMC de 24kg/m2 para obesidad >35% con una sensibilidad del 90% y una especificidad del 75% (área bajo la curva [AUC] 0,917), un IMC de 25kg/m2 para obesidad >40% con una sensibilidad del 86% y una especificidad del 39% (AUC 0,822) y un IMC de 22kg/m2 para 35% de la grasa central con una sensibilidad de 97% y una especificidad del 84% (AUC 0,951).
ConclusiónExiste un subdiagnóstico de obesidad con el uso de los valores de tradicionales de IMC en pacientes con AR bien controlados.
Rheumatoid arthritis (RA) is a chronic, inflammatory, autoimmune disease. Among the extra-articular manifestations RA is associated with an increased risk of cardiovascular disease (CVD) and osteoporosis.
Body composition is indirectly affected in individuals with RA. The factors that influence it include the activation of proinflammatory cytokines that trigger metabolic changes, with the resulting degradation of lean body mass; the inactive lifestyle, which reduces muscle mass and increases body fat1–4; the prevalence of obesity in individuals with RA per se; and age. More than 60% of RA patients have a body mass index (BMI) over the normal value (>25kg/m2).5,6 Giles et al. found that the phenotype for obesity is overexpressed in patients with RA, especially in those whose BMI is in the normal range. Disease activity and treatment for RA are factors that can contribute to this abnormality.7
Body mass index is the anthropometric assessment most widely utilized to determine the presence of obesity.4 However, in patients who have an alteration in their body composition (as in RA), it cannot be utilized as a valid predictor of body fat nor, therefore, of CVD.4,8,9 Dual X-ray absorptiometry, also referred to as densitometry (DXA), is considered the gold standard for the measurement of body composition.10 Previously, in different studies, DXA has been used to evaluate body composition in RA patients,7,11 although the definitions of obesity according to the percentage of body fat vary depending on the population studied.
The objective of this study was to evaluate the value of BMI in identifying obesity by means of DXA in patients with well-controlled RA.
MethodsParticipantsWe performed an observational, cross-sectional, descriptive and analytical study, for which we obtained approval from the institutional ethics committee (RE 12-020). The study involved patients with RA, in accordance with the 2010 classification criteria of the American College of Rheumatology and the European League Against Rheumatism (ACR/EULAR),12 who belonged to the cohort of rheumatic diseases of Hospital Universitario Dr. José Eleuterio González, in Monterrey, Nuevo León, México. The period of evaluation was from January to August 2013.
We excluded patients with contraindications for DXA: presence of joint prosthesis, body weight greater than 135kg, pregnant patients and those who were nursing. We analyzed clinical, demographic and laboratory variables. Disease activity was evaluated using the Disease Activity Score 28-erythrocyte sedimentation rate (DAS28-ESR).
Body Mass Index and Body Composition MeasurementsHeight was measured using a wall-mounted stadiometer. Weight was evaluated with light clothing and without shoes. Body mass index was calculated with the weight (kg) divided by height in meters squared. To define obesity, we used 2 classifications: that of the World Health Organization (WHO), which categorizes a patient depending on the resulting BMI and considers low weight <18.5kg/m2, normal weight between 18.5 and 24.9kg/m2, overweight between 25 and 29kg/m2 and obesity ≥30kg/m2, and the adjusted index for patients with RA (AI-RA) establishes a cut-off point to define obesity as 28kg/m2, a finding that was validated by bioelectrical impedance.4
Body composition and the distribution of regional body fat were evaluated using a densitometer (Hologic Full Body Densitometer, Model Discovery W. APEX software 3.3.0.1, version 13.3.0.1:7). Dual X-ray absorptiometry is capable of differentiating bone, muscle and fat, and calculates the total body mass (kg), fat mass (grams), fat percentage and lean mass (grams), as well as the regional distribution of these components.
To determine the diagnostic value of BMI to establish the presence of obesity employing DEXA, it was necessary to utilize a specific definition of obesity in the Mexican population as obtained by DXA. In the absence of a validated definition, we applied different cut-off points in accordance with studies published previously. We divided the patients into 3 groups based on the results of DXA: >35% of total body fat,13 >40% total body fat15 and, in the third group, central obesity was defined by the presence of 35% or more of central fat mass (trunk),15 since visceral adiposity is considered an independent predictor of morbidity and mortality.
Statistical AnalysisWe provide a descriptive analysis of the clinical and demographic variables. For continuous variables, after a test for normality (Kolmogorov–Smirnov), we used the mean and standard deviation (SD). For the categorical studies, we used frequencies and percentages. Receiver operating characteristic (ROC) curves were utilized to determine the optimal cut-off points for each BMI, in relation to the definition of obesity by DXA employed; sensitivity and specificity analyses were performed. Moreover, we compared the values for the definition of obesity by the WHO with those proposed for DXA. We used the SPSS (version 20) software package. We considered a P value less than .05 to indicate statistical significance.
ResultsParticipantsWe included 101 RA patients, 97 (96%) of whom were women, with an overall mean age of 50.54 years (SD 12.3). The remainder of the baseline characteristics are shown in Table 1. The mean weight and height were 69.3kg (SD 13.01) and 153cm (SD 6), respectively, with a mean BMI of 29.29kg/m2 (SD 5.4).
Clinical and Demographic Variables.
| Variable | |
|---|---|
| Age in years, mean (SD) | 50.4 (12.3) |
| Female gender, n (%) | 97 (96) |
| Years since the diagnosis of RA, mean (SD) | 9.8 (8.6) |
| RFa, n (%) | 61 (71.8) |
| Anti-CCPb, n (%) | 31 (57.4) |
| DAS28-ESR, median (IQR) | 3.26 (1.29) |
| HAQ, median (IQR) | 0.62 (0.68) |
| Use of DMARD, n (%) | 98 (98) |
| Use of methotrexate, n (%) | 85 (85.9) |
| Use of prednisone, n (%) | 47 (46.5) |
| Hypertension, n (%) | 18 (18.2) |
| Dyslipidemia, n (%) | 15 (15) |
| Type 2 diabetes mellitus, n (%) | 10 (10) |
| Hypothyroidism, n (%) | 7 (7) |
CCP, cyclic citrullinated peptide; DAS28, Disease Activity Score; DMARD, disease-modifying anti-inflammatory drug; ESR, erythrocyte sedimentation rate; HAQ, Health Assessment Questionnaire; IQR, interquartile range; RA, rheumatoid arthritis; RF, rheumatoid factor; SD, standard deviation.
According to the WHO, the patients were categorized as: 24 (23.8%) with normal weight, 38 (37.6%) were overweight and 39 (38.6%) had some degree of obesity. In accordance with the AI-RA, 13 (12.9%) were normal, 34 (33.7%) were overweight and 54 (53.5%) of the patients were obese (Table 2).
Anthropometric Evaluation, in Accordance With the Different Definitions.
In body composition determined by DXA, we found a mean total body fat of 30.93kg (SD 9.12), which corresponds to a mean total body fat percentage of 44.8% (SD 6.4) and a mean fat index of 13.08kg/m2 (SD 4.01). Total lean mass was 36.96kg (SD 5.44), which corresponds to a mean lean mass index of 15.57kg/m2 (SD 1.97). Table 2 includes the distribution of the patients according to the definition of obesity by DXA.
Fig. 1 shows the ROC curves, that determined that the total diagnostic value (area under the curve [AUC]) of BMI to establish obesity in accordance with the proposed definitions were: 0.917 for >35%; 0.822 for >40%; and 0.951 for >35% abdominal fat.
Receiver operating characteristic curves for the 3 definitions proposed for obesity in accordance with DXA. Panel A: Value of BMI for determining obesity in accordance with the DXA definition of >35% total body fat. Area under the curve: 0.917. Panel B: Value of BMI for determining obesity in accordance with the DXA definition of >40% total body fat. Area under the curve: 0.822. Panel C: Value of BMI for determining obesity in accordance with the DXA definition of >35% abdominal fat. Area under the curve: 0.951. BMI, body mass unit; DXA, dual X-ray absorptiometry.
To establish the best cut-off point for BMI to define obesity according to the different proposals, with their respective sensitivity and specificity values, we found that: DXA-measured obesity >35% total body fat, a BMI of 24kg/m2 with a sensitivity of 90% and a specificity of 75%; DXA-measured obesity >40% total body fat, a BMI of 25kg/m2 with a sensitivity of 86% and a specificity of 39%; and obesity >35% abdominal fat, a BMI of 22kg/m2 with a sensitivity of 97% and a specificity of 84%. These findings contrast with the standard cut-off points for BMI proposed by the WHO to define obesity, where a cut-off point for BMI>30kg/m2 has a sensitivity and specificity of 43% and 100% for >35% of total body fat, 45.5% and 89% for >40% total body fat, and 42% and 100% for >35% abdominal fat, respectively (see Fig. 1).
DiscussionWe observed that the detection of obesity using DEXA (with any definition) was higher in comparison with the BMI determined by the WHO and by the AI-RA. The cut-off point of the clinical BMI most widely used to detect or classify an obese patient is not sufficient to classify this group of patients. We found different BMI values in accordance with their better yield, in comparison with the definitions utilized for DEXA. The BMI for 35% of the total body fat was 24kg/m2, with a sensitivity of 90% and a specificity of 75% (AUC 0.917), for 40% of body fat it was 25kg/m2, with a sensibility of 86% and a specificity of 39% (AUC 0.822) and for 35% of the abdominal fat it was 22kg/m2, with a sensitivity of 97% and a specificity of 84% (AUC 0.951).
The AI-RA was created to improve the detection of obesity in RA patients using bioelectrical impedance. Its definition estimates a reduction of 2kg/m2 of the BMI for each classification and, thus, obesity is defined as a BMI of 28mg/kg.2,4 We observed that this cut-off point was not as sensitive or specific as the definitions proposed for DEXA (see Fig. 1). We consider that the value of this index is related to the use of bioelectrical impedance as a reference standard for the measurement of fat mass.
In our study population, there were other variables that could interfere with body composition that were not evaluated. The patients with RA had a low disease activity and, moreover, these individuals were younger than those of other body composition studies.7,11
As a result of these observations, we used different definitions of DXA-measured obesity because none of them has been established and validated for the Mexican population. The definition of obesity based on 35% of total body fat was obtained from the work of Velázquez-Alva et al. The authors evaluated 175 young Mexican women with an average BMI of 23.1 (SD 4.2). They found a mean total body fat of 35.36% (SD 7.0) using DXA.13 In contrast, the use of the definition involving 40% total body fat was obtained from a study by Cesari et al. in a non-Hispanic population.14
The main objective of the BMI is that it be used as a clinical tool to predict the risk of CVD on the basis of the body composition. We know that central obesity is one of its best predictors. Thus, we decided to add the third definition of DXA-measured obesity (>35% of trunk fat).15 We observed that this definition showed the best AUC (Fig. 1), with the best value at the BMI cut-off point of 22kg/m2.
Among the limitations of the study, there is no healthy control group to compare the results. Moreover, we consider that the arbitrary choice of the DEXA-measured fat mass percentage is a bias for the study.
The results obtained in the study include a high percentage of women; therefore, these observations cannot be applied to male RA patients.
In conclusion, we observe an underestimated detection of obesity with the BMI cut-off points most widely used, comparing them with DEXA in well-controlled RA patients. We propose that a BMI cut-off value of 22kg/m2 could help in the detection of abdominal obesity and, thus, a better definition of the risk of CVD. These results should be evaluated in a prospective study to determine the future clinical implications.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
The authors wish to express their appreciation to the following persons for their contribution to this article: Octavio Ilizaliturri-Guerra, Jorge Rodríguez-Olivo. And to the members of the CEAR Group: Diana Flores-Alvarado, Cassandra Skinner-Taylor, Lorena Pérez-Barbosa, Jannet Riega-Torres, Dionicio Galarza-Delgado, Miguel Villarreal-Alarcón, Daniel Treviño-Montes, Iris Colunga-Pedraza, Lorenia de la Cruz-Becerra, Karina Silva-Luna.
Please cite this article as: Tello-Winniczuk N, Vega-Morales D, García-Hernandez PA, Esquivel-Valerio JA, Garza-Elizondo MA, Arana-Guajardo AC. Desempeño del índice de masa corporal para el diagnóstico de obesidad por medio de absorciometría de rayos X de energía dual (DEXA) en pacientes con artritis reumatoide. Reumatol Clin. 2017;13:17–20.