To describe the variability of the day care hospital units (DCHUs) of Rheumatology in Spain, in terms of structural resources and operating processes.
Material and methodsMulticenter descriptive study with data from a self-completed questionnaire of DCHUs self-assessment based on DCHUs quality standards of the Spanish Society of Rheumatology. Structural resources and operating processes were analyzed and stratified by hospital complexity (regional, general, major and complex). Variability was determined using the coefficient of variation (CV) of the variable with clinical relevance that presented statistically significant differences when was compared by centers.
ResultsA total of 89 hospitals (16 autonomous regions and Melilla) were included in the analysis. 11.2% of hospitals are regional, 22.5% general, 27% major and 39.3% complex. A total of 92% of DCHUs were polyvalent. The number of treatments applied, the coordination between DCHUs and hospital pharmacy and the post graduate training process were the variables that showed statistically significant differences depending on the complexity of hospital. The highest rate of rheumatologic treatments was found in complex hospitals (2.97 per 1000 population), and the lowest in general hospitals (2.01 per 1000 population). The CV was 0.88 in major hospitals; 0.86 in regional; 0.76 in general, and 0.72 in the complex.
ConclusionsThere was variability in the number of treatments delivered in DCHUs, being greater in major hospitals and then in regional centers. Nonetheless, the variability in terms of structure and function does not seem due to differences in center complexity.
Describir la variabilidad de las unidades de hospitalización de día (UHdD) de Reumatología en España, en términos de recursos estructurales y procesos de funcionamiento.
Material y métodosEstudio descriptivo, multicéntrico, con evaluación de las UHdD mediante cuestionario autocumplimentado a partir de estándares de calidad de la Sociedad Española de Reumatología. Se analizaron recursos estructurales y procesos de las UHdD estratificados por complejidad del hospital (comarcal, general, mayor y complejo), y se determinó la variabilidad mediante el coeficiente de variación (CV) de la variable con relevancia clínica que presentara diferencias estadísticamente significativas al comparar por centros.
ResultadosUn total de 89 centros (16 comunidades autónomas y Melilla) se incluyeron en el análisis. El 11,2% de los hospitales son comarcales; el 22,5%, generales; el 27%, mayores, y el 39,3%, complejos. El 92% de las UHdD son polivalentes. El número de tratamientos aplicados, la coordinación entre las UHdD y farmacia hospitalaria y la presencia de formación posgrado fueron las variables de proceso que presentaron diferencias estadísticamente significativas en función del nivel de complejidad del hospital. La tasa de tratamientos más alta se halló en hospitales complejos (2,97 por 1.000 habitantes), y la más baja, en hospitales generales (2,01 por 1.000 habitantes). El CV fue de 0,88 en hospitales mayores, de 0,86 en comarcales, de 0,76 en generales y de 0,72 en los complejos.
ConclusionesExiste una mayor variabilidad en el número de tratamientos de UHdD en los hospitales mayores, seguido de los comarcales. Sin embargo, la variabilidad en estructura y funcionamiento no parece deberse a diferencias de complejidad de los centros.
Introduction to biological therapies (BT), which began in 2000, lead to the incorporation of a day care hospital unit (DCHU) in rheumatology departments.1,2 The possibilities offered by this health care provision, as opposed to conventional outpatient clinics, have enabled a progressive extension of the service portfolio beyond the administration of intravenous therapies, making it possible to perform diagnostic and therapeutic procedures, allowing a greater implication in clinical research and, even, the monitoring and management of all BT, even those that require subcutaneous administration.3 This guarantees a greater efficacy and continuity of care, avoiding the need to be attended to in other areas, such as the emergency department, or hospital admission, with an evident increase in patient satisfaction.4
As an independent functional unit, the DCHU requires certain specific structural and functional conditions that guarantee quality care and patient safety, as well as efficiency. However, the expansion of the DCHU in Spain has been heterogeneous, utilizing different models, depending on the needs and available local resources.5,6
Given the lack of a specific model, and with the only reference for the quality standards and recommendations for the DCHU provided by the Spanish Health Ministry,7 a working group from the Sociedad Española de Reumatología (SER) prepared, in 2012, its own document on the service portfolio and quality standards of a rheumatology DCHU.3 In accordance with these standards, the VALORA project undertook the evaluation of the structural resources and processes carried out in the DCHU of Spanish centers for the purpose of analyzing the differences in care among them.
Material and MethodsDesignThe VALORA project is a multicenter, cross-selective, descriptive study, within the framework of the ÍCARO plan organized by the SER, which seeks to improve clinical practice through the development and evaluation of quality criteria, indicators and standards.
The VALORA project integrates quantitative and qualitative methods. This report uses a self-administered questionnaire, employing as a reference, the quality standards selected by the SER DCHU working group.3
Center Selection and RecruitmentUsing a database provided by the SER that records information on the DCHU of Spanish institutions, 116 centers were asked to participate, following criteria according to geographic representation (Spanish autonomous communities and provinces). Sixteen autonomous communities and 99 centers participated; self-evaluation was performed between May and September of 2012.
Information Collection and Variable SelectionInformation was gathered using a self-administered questionnaire completed by physicians or nurses of the DCHU, that had been designed and approved by the scientific committee of the project, which was comprised of 20 experts. The project was coordinated methodologically by a professional from the SER research unit with training and experience in studies of this type, and the questionnaire was supervised in 3 centers.
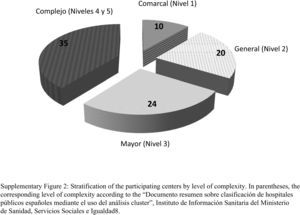
The variables are structured into 3 blocks. The first includes information on the features of the hospital and the rheumatology department. The level of complexity of the center was classified by taking as a reference a “Summary of a document on the classification of Spanish public hospitals using cluster analysis”, of the Ministry of Health, Social Services and Equal Opportunities.8 To aid in understanding, the centers were designated in descriptive terms and stratification was simplified: level 1 corresponds to regional, level 2 to general, level 3 to major, and levels 4 and 5 jointly comprise those classified as complex (Table 1).
Features of the Groups of Hospitals.
| VALORA | Cluster analysis | |
|---|---|---|
| Complex | Group 5 | Large hospitals, with a considerable physical structure and a very large work burden; more than 900 beds; more than 470 physicians and an average number of around 300 medical residents (MIR) in 36 different specialties (minimum 17). The latest technological advances, with an extensive portfolio of complex services (at least 5 complex departments) and a mean case-mix of 1618. Large campuses enter in this group. |
| Group 4 | Large hospitals, with less homogeneity than those of the preceding group. Between 500 and 1000 beds and the equivalent of 200–900 full-time physicians. With an average of 4 complex departments, characterized by a very high mean case-mix (1.84), and their emphasis on teaching: all the hospitals in the group have at least 25 accredited MIR specialties (average of 30) and more than 100 MIR. | |
| Major | Group 3 | Medium-sized hospitals with around 500 beds (although the variability is high), up to 160 MIR and between 100 and 500 physicians; certain complexity in the case-mix, average 1.39. |
| General | Group 2 | There are many hospitals in this group. Less than 500 beds, reduced teaching emphasis, although some have MIR training and up to 8 different specialties; they may have an ATM apparatus and, at most 2 complex departments. The case-mix is greater than 1, with an average of around 1.3. |
| Regional | Group 1 | Small hospitals with nearly no ATM staff and a case-mix of less than 1. Fewer than 200 physicians. |
Modified from the Spanish Institute of Health Care Information.8
The second block of variables comprises gathering information on the minimal conditions in terms of the necessary infrastructure or logistics for the effective implementation of the DCHU, and the third involves the care provided in those units. The variables and their operative definitions can be found in supplementary material.
Variability in Clinical PracticeWe analyzed the variability in those structural features or care processes that, having shown statistically significant differences (P<.05) on stratification for hospital complexity, were considered clinically relevant by the scientific committee.
Statistical AnalysesThe numerical variables with a normal distribution were expressed as means and standard deviation, and the asymmetric variables as median and interquartile range [p25–p75]. The absolute and relative frequencies were calculated for the categorical variables. The results are shown overall, as well as stratified according to hospital complexity. The nonparametric Kruskal–Wallis test was used to compare the continuous variables, and the chi-square test for the categorical variables. To determine the variation in clinical practice of the continuous variables, we estimated the adjusted risk for the reference population according to the hospital complexity, and calculated the coefficient of variation (CV), considering that variability existed when the CV was greater than 1.
Data management and statistical analyses were carried out by the SER research unit. The analysis were performed using the SPSS 21.0 statistical software package, assuming a level of statistical significance less than .05.
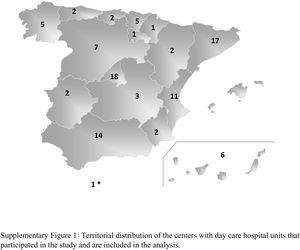
ResultsCharacteristics of the Participating CentersOf the 99 centers to which the questionnaire was sent, 89 completed the self-evaluation and were analyzed. Their geographic distribution is shown in Fig. 1, in the supplementary material, and the features of the centers and the department to which the DCHU belonged appear in Table 2. In all, 11.2% of the hospitals were regional, 22.5% were general, 27% were major hospitals and 39.3% were complexes (Fig. 2, in the supplementary material). The questions were responded to by 71 rheumatologists and 28 nurses.
Features of the Center and the Rheumatology Department.
| Total (n=89) | Regional (n=10) | General (n=20) | Major (n=24) | Complex (n=35) | P | |
|---|---|---|---|---|---|---|
| Population covered, mean (SD) | 337,339 (188.83) | 175,284.2 (156,768.5) | 241,076.4 (118,970) | 352,074 (236,550.6) | 412,970 (156,355.5) | .002 |
| Hospital beds, mean (SD) | 632.5 (354.2) | 146.8 (44.4) | 380.3 (162.1) | 595.7 (218.7) | 936.7 (284.5) | <.001 |
| Rheumatology beds, median [p25–p75] | 4 [0–6] | 0 [0] | 1 [0–4] | 4 [1–5] | 4.5 [4–6] | <.001 |
| First visits to rheumatology, median [p25–p75] | 3438.5 [1841.8–6268.0] | 1171.50 [813.3–1403.5] | 2475.00 [2248.8–3158.0] | 3205.0 [1809.0–5455.75] | 3438.5 [1738.2–4213.0] | .01 |
| Successive visits to rheumatology, median [p25–p75] | 8209.5 [5313.3–15,838.0] | 2991.5 [2083.5–4581.0] | 5630.0 [4581.5–7331.0] | 9314.5 [6495.2–5455.7] | 11,000 [7913.0–13,500.0] | <.001 |
| Rheumatology hospital admissions, median [p25–p75] | 61.5 [20.2–142.2] | 0 [0–10] | 42.5 [18–97.8] | 68 [9.5–120.5] | 100 [55–164] | .213 |
| Rheumatologists, median [p25–p75] | 5 [3–8] | 2 [2.3] | 3.5 [2.25–5] | 5 [4.25–8] | 7.5 [5–9] | <.001 |
| Nursing staff, median [p25–p75] | 1 [1.2] | 0 [0–1] | 1 [0–2] | 1 [1.2] | 1 [1.2] | .278 |
| Undergraduate education, % (n) | 61.8 (55) | 10(1) | 40 (8) | 75 (18) | 80 (28) | <.001 |
| Postgraduate education, % (n) | 44 (37) | 0 (0) | 11.1 (2) | 50 (11) | 70.6 (24) | <.001 |
| Rheumatology clinical discussion sessions, % (n) | 89.9 (80) | 50 (5) | 90 (18) | 100 (24) | 94.3 (33) | <.001 |
| Multidisciplinary appointments, % (n) | 57.3 (51) | 30 (3) | 30 (6) | 66.7 (16) | 74.3 (26) | .003 |
| Single-specialty appointments, % (n) | 73 (65) | 10 (1) | 65 (13) | 87.5 (21) | 85.7 (30) | <.001 |
| Nursing appointments, % (n) | 51.7 (46) | 50 (5) | 35 (7) | 41.7 (10) | 68.6 (24) | .066 |
| Clinical research (CT), % (n) | 89.9 (80) | 50 (5) | 80 (16) | 100 (24) | 100 (35) | <.001 |
| Publicly-funded research, % (n) | 61.8 (55) | 40 (4) | 40 (8) | 70.8 (17) | 74.3 (26) | .027 |
CT, clinical trials; SD, standard deviation.
The nonparametric Kruskal–Wallis test was used to compare continuous variables and the chi-square test for categorical variables.
Overall, 73% of the departments had dedicated units and 51.7%, had nurses’ offices; 61.8% gave college classes and 44% gave postgraduate courses; 89.9% participated in clinical trials and, 62%, in research projects with public funding.
Structural Resources of the Day Care Hospital UnitsThe variables analyzed appear in Table 3. We should mention that 92.1% of the DCHU were multipurpose. The average number of working days was 5.1 (0.3) per week, with no significant differences from one hospital level to another. In contrast, working both mornings and afternoons depended on the hospital, and was more frequent in general (70%) and major (54.2%) hospitals.
Structural Resources in the Day Care Hospital Units.
| Total (n=89) | Regional (n=10) | General (n=20) | Major (n=24) | Complex (n=35) | P | |
|---|---|---|---|---|---|---|
| Type (multipurpose), % (n) | 92.1 (82) | 100 (10) | 100 (20) | 95.8 (23) | 82.9 (29) | .067 |
| Suitable access and location, % (n) | 94.4 (84) | 100 (10) | 95 (19) | 95.8 (23) | 91.4 (32) | .734 |
| Reception area, % (n) | 80.9 (72) | 80 (8) | 80 (16) | 83.3 (20) | 80 (28) | .989 |
| Treatment administration area, % (n) | 14 (8.8–23) | 10.5 (7.8–13.3) | 20 (11–27) | 12 (8–20.8) | 14 (9.8–21.3) | .055 |
| Privacy in the office/room, % (n) | 69.7 (62) | 80 (8) | 60 (12) | 67.7 (16) | 74.3 (26) | .605 |
| Nursing monitoring area, % (n) | 94.4 (84) | 100 (10) | 95 (19) | 100 (24) | 88.6 (31) | .234 |
| Availability of a telephone consultation service, % (n) | ||||||
| Call registry | 31.5 (28) | 20 (2) | 15 (3) | 45.8 (11) | 34.3 (12) | .136 |
| Personal identification | 68.1 (55) | 50 (5) | 60 (12) | 62.5 (15) | 65.7 (23) | .838 |
| Hours for phone service | 43.8 (39) | 30 (3) | 20 (4) | 50 (12) | 51.7 (12) | .041 |
| Availability of centralized cubicles, % (n) | 61.8 (55) | 60 (6) | 70 (14) | 50 (12) | 55.7 (23) | .527 |
| Availability of resuscitation trolley, % (n) | 95.5 (85) | 100 (10) | 95 (19) | 95.8 (23) | 94.3 (33) | .894 |
| Air conditioning, % (n) | 98.9 (88) | 100 (10) | 100 (20) | 95.88 (23) | 100 (35) | .434 |
| Hours (morning and afternoon), % (n) | 49.4 (44) | 20 (2) | 70 (14) | 54.2 (13) | 42.9 (15) | .053 |
| Days open during the week, mean (SD) | 5.1 (0.3) | 5.1 (0.3) | 5.1 (0.2) | 5 (0.2) | 5.1 (0.3) | .664 |
| Electronic format connected to the hospital information systems, % (n) | 92.1 (82) | 90 (9) | 95 (19) | 87.5 (21) | 94.3 (33) | .747 |
| Specific electronic agenda for appointments, % (n) | 78.7 (70) | 90 (9) | 70 (14) | 75 (18) | 82.9 (29) | .528 |
| Electronic medical records, % (n) | 73 (65) | 80 (8) | 65 (13) | 79.2 (19) | 71.4 (25) | .974 |
| Minimum data set, % (n) | 61.5 (61) | 50 (5) | 65 (13) | 67.7 (13) | 61.1 (17) | .399 |
| Physician assigned to the DCHU, % (n) | 42.7 (38) | 30 (3) | 30 (6) | 41.7 (10) | 54.3 (19) | .272 |
| Nursing staff, mean (SD) | 2 (1.7–4) | 2 (1.8–3.3) | 2.5 (1–4.8) | 2 (1–6) | 2 (2–4) | .746 |
| Nursing staff with training in rheumatology, % (n) | 47.2 (42) | 30 (3) | 35 (7) | 37.5 (9) | 65.7 (23) | .044 |
| Ancillary staff, mean (SD) | 2 (1–2) | 1 (1–2) | 2 (1–2.3) | 2 (1–3.5) | 2 (1–2) | .613 |
| Administrative staff, % (n) | 65.2 (58) | 60 (6) | 40 (8) | 70.8 (17) | 67.1 (27) | .041 |
| Coordinator, % (n) | ||||||
| Non-rheumatology physician | 13.6 (12) | 22.2 (2) | 20 (4) | 12.5 (3) | 8.6 (3) | .403 |
| Rheumatologist | 28.4 (25) | 11.1 (1) | 15 (3) | 29.2 (7) | 40 (14) | |
| Nursing staff | 58 (51) | 66.7 (6) | 65 (13) | 58.3 (14) | 51.4 (18) | |
| Availability of key documents, % (n) | 100 (89) | 100 (10) | 100 (20) | 100 (24) | 100 (35) | |
DCHU, day care hospital unit; SD, standard deviation.
The nonparametric Kruskal–Wallis test was used to compare continuous variables and the chi-square test for categorical variables.
With respect to infrastructures and implementation, 78.7% had an electronic agenda for patient appointments and 73% had electronic medical records. Overall, 71% had administrative support and 69% gathered data according to a protocol.
Despite the predominance of multipurpose DCHU, 47.2% of the nurses were trained in rheumatology, and up to 65.7% (P<.044) in complex centers. The coordinator of the DCHU was most frequently from the nursing staff (58%), followed by a rheumatologist (28.4%). However, the presence of a rheumatologist as coordinator became more common as the complexity of the institution increased (Table 3). In all, 38% of the units had a specific rheumatologist assigned to said position.
With respect to the availability of key documents, 92% of the DCHU had no clinical practice guidelines/protocols for rheumatology, and only 52% could provide standardized work procedures. Overall, 63% maintained they had an organization manual; 52% had an admission plan and, nearly half, had a quality plan.
Processes Treated in Day Care Hospital UnitsThe processes analyzed are summarized in Table 4. In all, 91% of the DCHU provided integrated visits (clinical evaluation, analysis and procedure), and coordination with pharmacy was considered efficient in 87.6% of the centers. This perception decreased to 60% in regional centers (P=.028).
Processes Carried out in Day Care Hospital Units.
| Total (n=89) | Regional (n=10) | General (n=20) | Major (n=24) | Complex (n=35) | P | |
|---|---|---|---|---|---|---|
| Treatments/procedures in the last year, mean (SD) | 748.83 (551.7) | 229 (125.65) | 420.82 (246.95) | 701.83 (451.16) | 1126.73 (574.30) | .001 |
| Admission and information to the patient, % (n) | 43.8 (39) | 30 (3) | 45 (9) | 50 (12) | 42.9 (15) | .76 |
| Patient registry, % (n) | 92.1 (82) | 90 (9) | 80 (16) | 91.7 (22) | 100 (35) | .068 |
| Integrated medical visit, % (n) | 91 (81) | 100 (10) | 80 (16) | 100 (24) | 88.6 (31) | .087 |
| Adequate coordination DCHU and hospital pharmacy, % (n) | 87.6 (78) | 60 (6) | 85 (17) | 95.8 (23) | 91.4 (32) | .028 |
| Updated medical protocols, % (n) | 69.7 (62) | 80 (8) | 55 (11) | 83.3 (20) | 65.7 (23) | .178 |
| Updated nursing protocols, % (n) | 78.7 (70) | 70 (7) | 85 (17) | 75 (18) | 80 (28) | .764 |
| Updated pharmacy protocols, % (n) | 57.3 (51) | 60 (6) | 60 (12) | 58.3 (14) | 54.3 (19) | .973 |
| Checklist, % (n) | 53.9 (48) | 40 (4) | 40 (8) | 62.5 (15) | 60 (21) | .312 |
| Health care and self-care education, % (n) | 85.4 (76) | 70 (7) | 80 (16) | 91.7 (22) | 88.6 (31) | .333 |
| Evaluation of care received, % (n) | 21.3 (19) | 10 (1) | 15 (3) | 29.2 (7) | 22.9 (8) | .538 |
| Undergraduate training in DCHU, % (n) | 24.7 (22) | 10 (1) | 10 (2) | 25 (6) | 37.1 (13) | .094 |
| Postgraduate training in DCHU, % (n) | 44.9 (40) | 10 (1) | 25 (5) | 33.8 (8) | 74.3 (26) | <.001 |
| Rheumatology sessions in which the DCHU is a topic, %a (n) | 61.3 (49) | 40 (2) | 38.9 (7) | 66.7 (16) | 72.7 (24) | .076 |
| Health and social care coordination, % (n) | 20.2 (18) | 0 (0) | 25 (5) | 16.7 (4) | 25.7 (9) | .301 |
| Preparation of discharge report, % (n) | 50.6 (45) | 40 (4) | 40 (8) | 58.3 (14) | 54.3 (19) | .549 |
| Coding DCHU discharge, % (n) | 23.6 (21) | 30 (3) | 15 (3) | 33.3 (8) | 20 (7) | .464 |
| Continuity with primary health care, % (n) | 61.8 (55) | 40 (4) | 50 (10) | 75 (18) | 65.7 (23) | .158 |
| Recording adverse events, % (n) | 57.3 (51) | 50 (5) | 35 (7) | 62.5 (15) | 68.6 (24) | .095 |
| Evaluation of patient satisfaction, % (n) | 21.3 (19) | 0 (0) | 15 (3) | 16.7 (4) | 34.3 (12) | .072 |
| Cost evaluation, % (n) | 42.7 (38) | 30 (3) | 40 (8) | 29.2 (7) | 57.1 (20) | .139 |
| Quality certification, % (n) | 15.7 (14) | 10 (1) | 10 (2) | 16.7 (4) | 20 (7) | .743 |
DCHU, day care hospital unit; SD, standard deviation.
The nonparametric Kruskal–Wallis test was used to compare continuous variables and the chi-square test for categorical variables.
Overall, 85.4% of the DCHU carried out health care education and had self-care activities. However, only 21.3% performed a key process like evaluating the care received through satisfaction surveys, and, in this, there were no differences with respect to the complexity of the hospital.
With regard to continuity of care, we should mention that 80% had a phone service, mostly attended to by nurses (81%), although the hours were not provided in more than half of the cases.
A DCHU was included in the postgraduate information in those hospitals whose complexity allowed it, reaching 75% in complex hospitals. However, this figure decreased in undergraduate training (37.1%), a finding that did not significantly differentiate them from the other 3 levels of complexity.
With regard to the processes of recording and evaluating their activity, almost all the DCHU maintained reports on their activity (94%), patients (90%) and treatment (97%). However, only 57.3% registered adverse events, and 36% had discharge coding. There was nearly no reporting on the evaluation of the health care professionals (21% in nursing) or on patient satisfaction (21%). The evaluation of the costs of the procedures was done in 42.7% of the units. Finally, only 15.7% of the DCHU had quality certification.
Variabilities Among Day Care Hospital UnitsUpon stratifying the structural resources of the DCHU according to hospital complexity, the variables that showed statistically significant differences were the presence of nursing staff with training in rheumatology (P=.044) and administrative personnel (P=.041), both of which were more common in hospitals with a higher level of complexity. With respect to processes performed in the DCHU, the number of treatments delivered, the coordination between the DCHU and the hospital pharmacy, and the presence of postgraduate training were the variables that showed statistically significant differences depending on the hospital complexity. We analyzed the variability in the treatments/procedures carried out in the DCHU, which were the variables with the highest clinical relevance that displayed statistically significant differences after stratifying for hospital type.
The average number of treatments in the DCHU, the year before this study, was 748.83 (551.7), and it grew progressively with the level of the center, as is demonstrated in Table 5. Thus, regional hospitals had an average of 229 (125.65) treatments per year, whereas in complex hospitals, it was 1126.73 (574.3) per year. Standardizing the number of treatments performed in the DCHU to the reference population covered by the center, the mean rate was 2.53 per 1000 population. If we stratified according to hospital complexity, the lowest rate was that of the general hospitals (2.01 per 1000 population), followed by the regional hospitals (2.29 per 1000 population), the major hospitals (2.44 per 1000 population) and, finally, the complex institutions (2.97 per 1000 population). The CV of the number of treatments was 0.74 and that of the rate of treatments, 0.79. On stratifying according to the complexity of the center, the greatest variability was observed in those classified as major (0.88) and regional hospitals (CV=0.86).
Clinical Variability in Treatments in the Day Care Hospital Unit According to Hospital Complexity.
| Number of treatments according to level of hospital complexity | Rates of treatments per 1000 population according to hospital complexitya | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | Regional | General | Major | Complex | Total | Regional | General | Major | Complex | |
| Mean | 748.83 | 229 | 420.82 | 701.83 | 1126.73 | 2.53 | 2.29 | 2.01 | 2.44 | 2.97 |
| SD | 551.7 | 125.65 | 246.95 | 451.16 | 574.30 | 2 | 1.97 | 1.52 | 2.15 | 2.13 |
| CV | 0.74 | 0.55 | 0.59 | 0.64 | 0.51 | 0.79 | 0.86 | 0.76 | 0.88 | 0.72 |
CV, coefficient of variation; SD, standard deviation.
The present study offers an image of the structural situation and implementation of the Spanish DCHU as a new model of health care provision that has adapted to the changes in the specialty of rheumatology. In this respect, the report includes the largest sample of rheumatology DCHU in Spain, with an extensive geographic representation and a diversity of institutions. It is the first to analyze the variability according to the level of complexity of each center. These features are some of the strengths of the study, which examines the findings from a perspective different from evaluations published earlier, with other objectives and methodologies.
Previous studies had smaller samples, either because they were restricted to the dedicated DCHU,2 because of its regional nature5 or because of the unique inclusion of hospitals we refer to as major and complex.6 On the other hand, an earlier study by Roman Ivorra et al.6 in 2008–2009 was not a variability study, but was based on an anonymous comparison exercise among 21 hospitals using 19 quality criteria. The present analysis, stratified in terms of the complexity of the centers, demonstrates that the structural resources and processes in a DCHU do not differ significantly according to the hospital complexity. A possible explanation is the fact that more than 90% correspond to multipurpose DCHU and reflect shared infrastructures and processes that any center offers when it has a DCHU. In this respect, we have seen a lower percentage of dedicated DCHU (8%) versus the study published in 2004, which focused on 24 dedicated DCHU, 27% of the total of 90 centers that had a DCHU at that time.2 The greater availability of subcutaneous biological therapies and the progressive incorporation into rheumatology departments of nursing offices may be the reasons for this change. In diseases like rheumatoid arthritis, expert care in a nursing office shows the same efficacy as multidisciplinary care in a DCHU.9 In our study, we found that more than half of the centers had nursing offices, possibly as the result of the promotion of their creation in the last decade.10 Finally, we must not forget the adaptation of the budget cuts of recent years in which, for greater efficiency, service provision and management should be centralized in a multipurpose DCHU.
Not every variability implies a deficiency or an uneven provision of health services. On occasion, it responds to an adjustment of the available resources, but it can also be subject to different preferences and alternatives of the circumstances to cover those needs. The results of the VALORA study show us that very few differences in the structure and implementation of the DCHU are due to the complexity of the centers. The self-evaluation of the DCHU using a comprehensive questionnaire based on previously established standards has enabled us to discover that certain structural resources or operative processes are nearly universal, where others are found in half of the DCHU or fewer.
Among the first we could mention suitable access, nearly generalized electronic format, availability of clinical practice protocols and other key documents (described by García-Vicuña et al.3), the existence of an electronic agenda and confirmation of the appointment, or the registration of patients and DCHU activity. A great majority of these units provide processes involving patient education and self-care, a phone service, suitable coordination with the hospital pharmacy and the possibility of having an integrated visit. Many of these processes are now being offered in more than 85% of the DCHU, as they constitute recommendations pointed out in previous studies.11 However, we have found that there is still a low percentage of compliance with certain key processes, that had previously been identified as areas in which to improve6,11: less than half maintain that they perform the process of patient admission, and only 21% carry out evaluations of the care received; undergraduate training reaches only a third of the teaching centers, and postgraduate instruction should be available in 100% of the centers that train Spanish medical residents (MIR). The procedures for discharge (reporting and coding) are still deficient, when they are central processes for health care continuity and permanence in the registry, not only of the activity, but of its complexity. Likewise, we consider insufficient the evaluation of the costs, which, together with other records (like adverse events, procedure coding), would enable us to justify an efficient and safe use of the resources, which less than half of the centers maintain they implement.
With respect to the variables involving processes that show significant differences, some are associated with the complexity of the center, some like the presence of a DCHU during postgraduate training, limited to teaching hospitals or those with a certain attribution profile. Specific training of the nursing staff in rheumatology also shows the differences among centers, and reaches only one third of the professionals, except in complex hospitals. This need, detected in earlier studies, was identified as an area in which improvement was a priority,5,6,11 particularly since the merit of nursing with all its advanced skills for the rheumatology setting, has been demonstrated in terms of patient safety12,13 and efficacy.12 Another variable that shows differences upon stratifying according to the level of hospital complexity is a suitable coordination between the hospital pharmacy and the DCHU, a key process that should be more implicated in regional hospitals. However, there do not appear to be structural differences in terms of personnel, the electronic communication system or the area in which medications are prepared (data not shown), or in processes like electronic prescription, to explain it.
Taking it into account that most of the procedures of the service portfolio of the rheumatology DCHU are directed toward the most complex patients, with a predominance of biological therapies, we selected a number of procedures performed in a DCHU to analyze the variability. In this respect, variations in medical practice have been defined as systematic—not random—variations in the standardized rates of a procedure (preventive, diagnostic, therapeutic, medical or surgical, etc.) in a certain level of incorporation of the population.14 Our results demonstrate certain variability in major hospitals and in less complex (regional) centers. The variability observed in the latter may be due to the fact that this study includes regional centers with special interest in questions of management and quality in the DCHU and that, thus, have been able to develop more in this area.5,11
Among the limitations of the present study we could point out self-evaluation. However, the report was not designed to evaluate the introduction of quality standards, and all the participants had received a manual with the definition of each variable.
Activity in the DCHU is essential to the specialty of rheumatology. Part of the viability and survival of our specialty in the hospital setting is based on the specialized care provided in the DCHU, without overlooking its contribution to research and training. It would be interesting to understand the impact of this activity on the patients and on professionals, and even to evaluate its efficiency. However, the availability of this information will probably be restricted to just a few DCHU and will not be explored in the present study. After this extensive descriptive analysis, we would like to design tools to facilitate the implementation of the standards we consider necessary and undertake their evaluation using indicators that enable us to determine their progress.15 Only in that way, in an intended future study, will we be able to be sure that we continue to advance.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe Spanish Foundation of Rheumatology (FER) with a grant awarded by Roche to finance the ÍCARO plan. The company did not participate in the design of the project or was involved in writing the conclusions or in the findings of the final report of this manuscript.
Conflicts of InterestThe authors declare they have no conflicts of interest with regard to the present manuscript.
The authors of this article wish to express their appreciation, in the first place, to the members of the Scientific Committee (Pilar Plana Macarulla, Esther Álvarez, Jennifer de la Torre, Pilar Pérez Ayuso, Laura Cano García, Sagrario Bustabad, Héctor Corominas i Macías, María Victoria Hernández, José Andrés Román Ivorra, José Luis Marenco, Carlos Fernández López, María Montero, Federico Navarro Sarabia, Laura Nuño, Eva Pérez Pampín, Joaquín Belzunegui, Carlos Marras, Concha Delgado and Javier Ballina), whose participation in the VALORA Project was crucial for its conception and implementation. In second place, to the nursing staff and physicians of the rheumatology departments who have participated in this work, for their interest and implication in the study subject, as was demonstrated by the high rate of participation.
We also wish to thank Estibaliz Loza Santamaría for her participation in the design of the study, and the statistician of the research unit of the SER, Fernando Sánchez Alonso, for his contribution in the data analysis.
Please cite this article as: Hernández Miguel MV, Martín Martínez MA, Corominas H, Sanchez-Piedra C, Sanmartí R, Fernandez Martinez C, et al. Variabilidad en los hospitales de día de Reumatología en España: proyecto VALORA. Reumatol Clin. 2017;13:10–16.