Sitosterolemia is an extremely rare autosomal recessive disease. The main characteristic is the absence of the routes that normally impede absorption and retention of noncholesterol sterols, like those found in plants and shellfish. The gene responsible for sitosterolemia is on chromosome 2p21, and mutations in any of the genes that comprise the locus encoding the adenosine triphosphate (ATP)-binding cassette (ABC) transporter, subfamily G (ABCG) proteins, ABCG5 or ABCG8, cause this disease.1–7
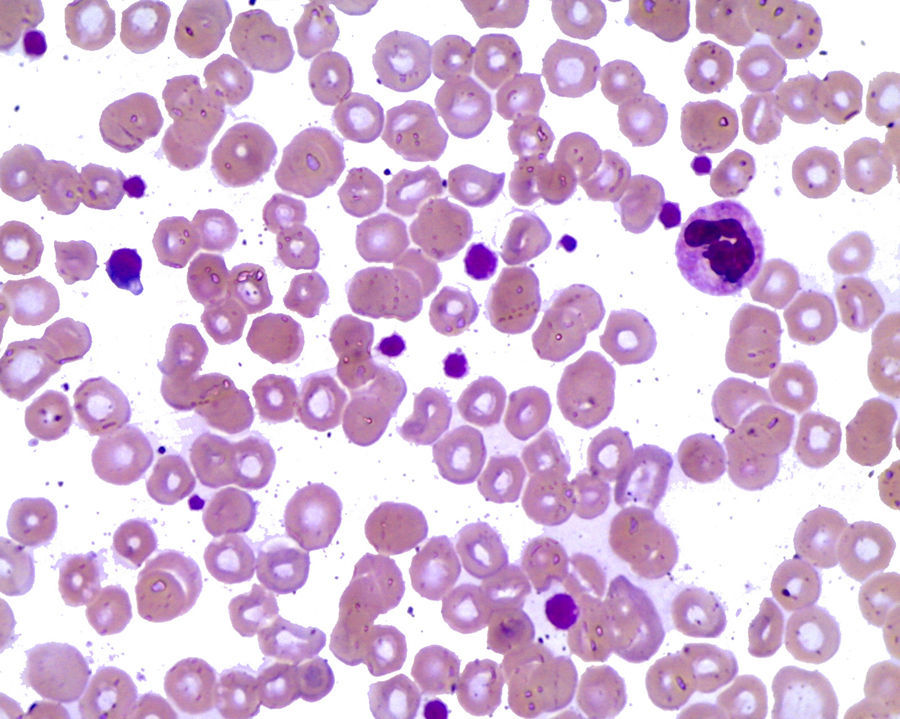
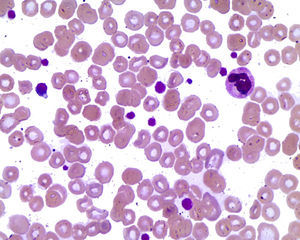
Case ReportThe patient was a 9-year-old boy who was referred to our department to be evaluated for probable juvenile idiopathic arthritis. He was the child of consanguineous parents (cousins), although the remainder of his hereditary and/or family background was unremarkable. At the age of 3 years, he began to complain of generalized arthralgia, at no predominant time of day or night, that did not change with physical activity or rest. It did not limit his daily activities, but would sometimes wake him up at night, and was relieved with massages and paracetamol. Our findings were increased volume in his knees, as well as the appearance of skin lesions on the extensor surfaces of elbows and knees and thrombocytopenia of 45,000mm3; epistaxis was ruled out. On physical examination, he was pale and had no abdominal organomegaly; there were painless nodular skin lesions of soft consistency on extensor surfaces of elbows and knees; they were not attached to deep layers of 2–3cm and thus, were suggestive of tuberous xanthomas; the Achilles tendon was enlarged due to subcutaneous nodular lesions (Fig. 1). The rest of the physical examination was unremarkable. The laboratory analyses showed leukocytes of 5270mm3, hemoglobin 11.4g/dL, reticulocytes 4.28%, peripheral blood smear with stomatocytes+schistocytes+large platelets++(Fig. 2), direct Coombs test negative, platelets 106,000mm3, mean platelet volume of 20fl, cholesterol 223mg/dL and triglycerides 132mg/dL. In Spain, the determination of serum phytosterol levels and the analysis of the ABCG5 and ABCG8 genes are not performed. Based on the presence of macrothrombocytopenia, hemolysis, elevated reticulocyte count, tuberous xanthomas and slightly elevated cholesterol and triglyceride levels, the diagnosis of sitosterolemia was established and treatment was begun with a diet low in phytosterols and ezetimibe at a dose of 10mg/day.
DiscussionIn 1974, Bhattacharyya and Connor reported a new disease in 2 Caucasian sisters who had been referred to them because of the presence of tendon xanthomas since their childhood. Surprisingly, the plasma cholesterol in these patients was within normal ranges, but they found elevations of the phytosterols (specifically β-sitosterol) and, thus, named the new disease β-sitosterolemia.4
Sitosterolemia is a rare autosomal recessive disease, characterized by markedly high levels of phytosterols, with a slight increase in the plasma cholesterol. It is caused by mutations in the ABCG5 or ABCG8 genes (adenosine triphosphate-binding cassette [ABC] transporter), located on chromosome 2p21, which helps to prevent sterol absorption and promote the excretion of phytosterols (sitosterol, campesterol and stigmasterol), preventing their accumulation in blood and tissues.1–4 The exact prevalence of sitosterolemia is unknown, but there are 80–100 cases worldwide.4–8
Plant sterols include the phytosterols and the phytostanols. Phytosterols are closely related to cholesterol, the main difference being the configuration of the side chain. The phytosterols most widely found are sitosterol, campesterol and stigmasterol. As humans are incapable of synthetizing phytosterols, their only source is the diet. Usually less than 5% of the phytosterols in the foods we consume is absorbed, in contrast to 55% of the cholesterol. The liver, rapidly and preferentially, excretes phytosterols into the bile. This leads to a low level of retention of noncholesterol sterols. In 1998, Patel mapped the locus of sitosterolemia, STSL, to chromosome 2p21. This locus is comprised of 2 adjacent genes, ABCG5 and ABCG8, which encode 2 intestinal sterol transporters, sterolin-1 and sterolin-2. Mutations in either of them lead to the development of sitosterolemia. These transporters are found in the apical membrane of enterocytes and in the biliary tract. ABCG5 and ABCG8 regulate the network of absorption and excretion of phytosterols and cholesterol. In enterocytes, they promote the flow of phytosterols back into the intestinal lumen and, in the liver, they promote the excretion of sterols into bile.4,6,7,9,10
The clinical signs vary, and can include the presence of tendon xanthomas, premature atherosclerosis, early myocardial infarction, arthritis, arthralgia, hemolysis, thrombocytopenia and hypersplenism. Sitosterolemia differs from familial hypercholesterolemia in that the cholesterol levels are normal.4–6,11
Macrothrombocytopenia associated with the absence of ABCG5 is caused by the increase in plasma phytosterol levels, not by any intrinsic defect of the megakaryocytes. Hemolysis is secondary to an increase in the osmotic fragility of the erythrocytes. As the ABCG5 and ABCG8 proteins are not present in platelets or erythrocytes, the accumulation of plant sterols in plasma and their insertion into the blood cell membranes is a better explanation for the abnormalities in morphology and function in patients with sitosterolemia. The xanthomas in the patellar, plantar and Achilles tendons and in the extensor tendons of the hands are present in all the cases that present during childhood. There can be recurrent arthralgia or arthritis in knees and ankles, which are due to sitosterol deposits.7,12,13
Blood tests show plasma cholesterol levels ranging from normal to slightly elevated, thrombocytopenia, chronic hemolytic anemia with a negative Coombs test and high liver enzyme levels.8 A peripheral blood smear aids in the diagnosis of sitosterolemia and is characterized by the presence of stomatocyte hemolysis, thrombocytopenia and macrothrombocytes.2,12
The plasma phytosterol levels in normal individuals do not surpass 1mg/dL, whereas the concentration in patients with sitosterolemia can be over 20–30mg/dL. Enzymatic methods or colorimetry are usually employed to quantify sterols, but they do not differentiate between cholesterol and plant sterols. The latter are detected using gas chromatography or high-performance liquid chromatography.4,9
The disease should be suspected in patients with tendon or tuberous xanthomas, early cardiovascular disease associated with normal cholesterol levels, or inexplicable hemolysis.4,6,9,11
The treatment of sitosterolemia includes a diet that avoids foods that are high in phytosterols (vegetable oils, margarine, olives, nuts, avocado, chocolate and shellfish).8,9,13 Improving the intestinal and hepatic routes of elimination of phytosterols in patients with sitosterolemia reduces the levels of plant sterols. Ezetimibe binds to NPC1L1, which is a sterol transporter in the small intestine, and blocks sterol absorption and reabsorption, resulting in low cholesterol and phytosterol levels.1,4,5,8 A recent study in 8 patients with sitosterolemia indicates that ezetimibe is effective, as it reduces the phytosterol levels in plasma and erythrocytes and improves the platelet count. The combination of ezetimibe with bile acid sequestrant resins, statins or diets low in phytosterols promotes a decrease in the plasma campesterol and sitosterol levels. Ezetimibe leads to a marked improvement in plasma sterol concentration, regression of the xanthomas and resolution of the cardiovascular disease.4,7,9,13 Liver transplantation was recently performed in a patient with sitosterolemia in whom the normalization of the plasma phytosterol levels were completely normalized.4
It was not possible to determine the phytosterol concentrations, but the clinical signs and peripheral blood smear led us to the diagnosis. Sitosterolemia should be considered in patients with xanthomas and thrombocytopenia, and the peripheral blood smear must be examined specifically to establish the presence or absence of macrothrombocytes and stomatocytes.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Please cite this article as: Torres-Jiménez AR, Solís-Vallejo E, Sanchez-Jara B, Cespedes-Cruz AI, Zeferino-Cruz M. Xantomas y macrotrombocitopenia: sitosterolemia es la respuesta. Reumatol Clin. 2016;12:164–166.