To investigate which of the 2 ankylosing spondylitis (AS) disease activity instruments identifies better those patients with characteristics that have been associated with positive response to anti-TNF therapy.
MethodsData from patients with AS in the REGISPONSER registry were analyzed. Patients were categorized by disease activity using 3 different selection criteria: elevated Bath Ankylosing Spondylitis Disease Activity Index criteria (BASDAI≥4), high Ankylosing Spondylitis Disease Activity Score (ASDAS≥2.1), or very high ASDAS (ASDAS≥3.5). To determine which criterion selects for patients most likely to respond to anti-TNF therapy, the groups of patients selected with each criterion were compared on five disease characteristics that are associated with good response to anti-TNF therapy: lower age, lower function score, less enthesitis, higher C-reactive protein (CRP), and HLA-B27-positive status.
Results50.9%, 66.3%, and 24.9% of 1156 patients had elevated BASDAI, high ASDAS, or very high ASDAS, respectively. Compared to patients selected with elevated BASDAI, more patients selected with high ASDAS had characteristics associated with good response to anti-TNF therapy. Patients with very high ASDAS had higher CRP and were younger, but more frequently had enthesitis and had higher function scores when compared to those with elevated BASDAI.
ConclusionsSelection of AS patients with the ASDAS instrument results in patient sub-populations with different characteristics than those selected with the BASDAI instrument. Since some of these characteristics have been associated with response to anti-TNF therapy, further study should establish if the choice of selection instrument improves the outcome of therapy in the selected populations.
Investigar cual de 2 instrumentos actividad de la enfermedad para espondilitis anquilosante (EA) identifica mejor a los pacientes con las características que se han asociado con una respuesta positiva a la terapia anti-TNF.
MétodosSe analizaron los datos de los pacientes con EA del registro REGISPONSER. Los pacientes fueron clasificados de acuerdo a la actividad de la enfermedad utilizando 3 criterios diferentes de selección: criterios de espondilitis anquilosante, Índice de Actividad de la Enfermedad elevado (BASDAI≥4), puntuación alta de Actividad de la Enfermedad (ASDAS≥2,1) o ASDAS muy elevado (ASDAS≥3,5). Para determinar qué criterio seleccionaba a pacientes con más probabilidades de responder a terapia anti-TNF, se compararon cinco características de la enfermedad que se asocian con una buena respuesta a la terapia anti-TNF en los grupos de pacientes seleccionados con cada criterio: edad menor, calificación de la función, menorentesitis, mayor nivel de proteína C-reactiva (PCR), y la presencia de HLA-B27 positivo.
Resultados50,9%, 66,3% y 24,9% de los 1.156 pacientes tenían BASDAI elevado, ASDAS alto, o muy altos, respectivamente. En comparación con los pacientes con BASDAI elevado seleccionados, más pacientes seleccionados con ASDAS altos tenían características asociadas con una buena respuesta a la terapia anti-TNF. Los pacientes con ASDAS altos tenía PCR más elevada y eran más jóvenes, pero con mayor frecuencia tenían entesitis y calificaciones de función más altos en comparación con aquellos con niveles elevados de BASDAI.
ConclusionesLa selección de los pacientes mediante los resultados del instrumento ASDASresulta en sub-poblaciones de pacientes con características diferentes a las seleccionadas con el instrumento BASDAI. Dado que algunas de estas características se han asociado con la respuesta a la terapia anti-TNF, se requiere de mayor estudio para establecer si la elección del instrumento de selección mejora el resultado del tratamiento en las poblaciones seleccionadas.
For patients with axial spondyloarthritis and patients with ankylosing spondylitis (AS) failing 2 or more nonsteroidal anti-inflammatory drugs (NSAIDs), recommendations for anti-tumor necrosis factor (anti-TNF) therapy require presence of elevated Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) and positive expert opinion using clinical disease characteristics.1–3 Even though clinical activity and physician judgment are still the main drivers for starting anti-TNF therapy, different studies suggest that demographic and disease characteristics, such as age, C-reactive protein (CRP), functionality, and HLA-B27 genotype may influence response to anti-TNF and therefore could help in the selection of candidates for treatment with these drugs.4–9
The reason elevated BASDAI is used for patient selection in treatment recommendations is because elevated BASDAI has also been used as a selection criterion in efficacy studies.10,11 However, because a higher BASDAI score has been associated with nonresponse and anti-TNF treatment discontinuation,5,7 selection with elevated BASDAI score may be a recipe for poor outcomes. As elevated disease activity is indispensable for patient selection, we investigated whether use of the newly developed Ankylosing Spondylitis Disease Activity Score (ASDAS) as selection instrument results in a different population of patients than those selected with BASDAI, and whether the populations could be characterized through characteristics that have been associated with response to anti-TNF therapy in published literature.9,12
MethodsDisease activity instrumentsThe BASDAI measures disease activity using six patient-reported questions pertaining to fatigue, spinal pain, joint pain/swelling, areas of localized tenderness, and morning stiffness.13 Patients have an elevated disease activity if the BASDAI score is ≥4 on a 10-point scale.
The ASDAS measures disease activity using an algorithm comprising 3 BASDAI questions (spinal pain, morning stiffness, and joint pain/swelling), the patient global assessment, and CRP.11 ASDAS≥1.3 indicates moderate, ≥2.1 indicates high, and ≥3.5 indicates very high disease activity.14
Characteristics associated with treatment outcomeLower age, lower Bath Ankylosing Spondylitis Functionality Index (BASFI), lower enthesitis score, higher CRP, and presence of HLA-B27 have been associated with good outcomes to anti-TNF therapy.3–8 Samples selected with the various disease activity measures/cutoffs were compared for their profile of these 5 characteristics.
Patient populationPatients with AS according to the modified New York criteria included in the Spanish national registry of spondyloarthropathies (REGISPONSER), who had complete data for BASDAI, ASDAS, age, CRP, BASFI, presence of enthesitis, and HLA-B27 status, were included in this analysis.15
AnalysisTwo-by-two cross-tabulation reflecting patient samples selected with BASDAI and ASDAS were created. Each sample's characteristics are reported using the following categories: BASFI≤4.5, 4.5–6.5, and >6.5; CRP
The difference between the numbers of patients selected with ASDAS versus BASDAI is reported for each subpopulation. Subpopulations that had a net increase or decrease when selected with ASDAS are presented in green and red, respectively. The proportion of patients falling into each of the 72 subpopulations, relative to the total population selected with BASDAI or ASDAS are reported.
ResultsA total of 1156 patients had complete data for all variables (mean age: 48 years [SD 13], 74.5% male and 25.5% female). Mean disease duration was 21.5 years (SD: 13), 84.9% had positive HLA-B27 and 34.6% had history of enthesitis. A total of 17.0% was being treated with anti TNF agents, 9.2% was taking steroids, 8.6% methotrexate, 14.2% suphasalazine and 0.6% leflunomide. CRP value was <0.6mg/dL in 53.2% of the sample, whilst 11.6% had ≥2.0mg/dL.
Table 1 shows the distribution of ASDAS and BASDAI values. Almost all patients had at least moderate ASDAS (Table 1A), two-thirds had at least high ASDAS (Table 1B), and one-quarter had very high ASDAS (Table 1C). Approximately half of the patients had elevated BASDAI. Among those with high ASDAS or high BASDAI, 14.3% and 15.1% were treated with anti TNF drugs respectively. Of 568 patients with a low BASDAI score, 210 patients had high disease activity as measured by ASDAS (37%, Table 1B), and only 16 had very high disease activity on ASDAS (2.8%, Table 1C). Of 390 patients with ASDAS <2.1, only 32 had elevated BASDAI (8.2%, Table 1B). There were no patients with ASDAS <1.3 and elevated BASDAI (Table 1C).
Two-by-two cross-tabulations of disease activity state as determined by the BASDAI criterion for elevated disease activity versus ASDAS criteria for moderate (A), high (B), and very high disease activity (C).
| BASDAI<4 | BASDAI≥4 (elevated activity) | Total | |
| (A) | |||
| ASDAS<1.3 | 142 | 0 | 142 (12.3%) |
| ASDAS≥1.3 (moderate activity) | 426 | 588 | 1014 (87.7%) |
| Total | 568 (49.1%) | 588 (50.9%) | 1156 (100%) |
| (B) | |||
| ASDAS<2.1 | 358 | 32 | 390 (33.7%) |
| ASDAS≥2.1 (high activity) | 210 | 556 | 766 (66.3%) |
| Total | 568 (49.1%) | 588 (50.9%) | 1156 (100%) |
| (C) | |||
| ASDAS<3.5 | 552 | 316 | 868 (75.1%) |
| ASDAS≥3.5 (very high activity) | 16 | 272 | 288 (24.9%) |
| Total | 568 (49.1%) | 588 (50.9%) | 1156 (100%) |
Table 2 shows that more patients selected with high ASDAS have disease characteristics that have been associated with positive outcomes of anti-TNF treatment in reported literature (markedly higher CRP and lower BASFI; slightly lower age, fewer patients with enthesitis, and more patients with HLA-B27 positive status) when compared to patients selected with elevated BASDAI. Patients with very high ASDAS had much higher CRP levels and were younger (both associated with positive outcomes in literature), but more frequently had enthesitis and had markedly higher BASFI scores (inversely associated with positive outcomes) when compared to those with elevated BASDAI. Characteristics of patients with moderate ASDAS were nearly identical to the total cohort (not shown).
Percentage of patients who had each characteristic that has been associated with positive anti-TNF treatment outcomes, by patient groups selected with ASDAS or BASDAI criteria.
| All patients (n=1156) | Patients with high disease activity, as determined by each selection criterion | |||
| ASDAS≥2.1 (n=766) | ASDAS≥3.5 (n=288) | BASDAI≥4 (n=588) | ||
| Age≤40 years | 28.6% | 26.4% | 24.0% | 23.1% |
| HLA-B27-positive | 84.9% | 85.1% | 83.0% | 83.5% |
| Never had enthesitis | 65.4% | 61.7% | 53.3% | 58.2% |
| BASFI | ||||
| ≥6.5 | 19.8% | 27.3% | 44.4% | 34.2% |
| 4.5–6.5 | 20.0% | 26.1% | 26.4% | 28.7% |
| <4.5 | 60.2% | 46.6% | 29.2% | 37.1% |
| CRP (mg/dL) | ||||
| ≥2 | 11.6% | 17.4% | 30.2% | 12.9% |
| 0.6–2 | 34.9% | 45.0% | 54.9% | 41.5% |
| <0.6 | 53.2% | 37.6% | 14.9% | 45.6% |
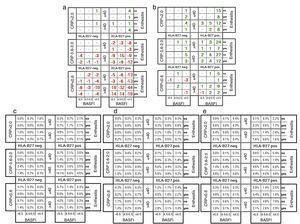
Relative to the total population included in this analysis, the proportion of patients in subpopulations identified with characteristics that have been associated with positive outcomes (i.e. expected to respond well and located to the right and top of the matrix grid) increases when selection is done with high ASDAS instead of BASDAI (Fig. 1B, D, and E). At the same time, few sub-populations are numerically decreasing when BASDAI is replaced by high ASDAS. These sub-populations are located at the bottom left of the matrix grid (i.e., associated with worse outcomes related to anti-TNF therapy) and the size of these subgroups relative to the total population goes down. If BASDAI is replaced by very high ASDAS, few subpopulations in the highest CRP category have a small increase, whereas most subpopulations show decreases in population size (Fig. 1A, C, and D).
Matrix representation of characteristics of patients selected with each criterion. Net numeric increase (green) or decrease (red) within each of the various subpopulations when the measure of disease activity used to select patients changes from elevated Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) to (A) Ankylosing Spondylitis Disease Activity Score (ASDAS) very high disease activity and (B) ASDAS high disease activity. Size of each of the 72 subpopulations, relative to the total population selected with the following disease activity measure: (C) very high ASDAS, (D) elevated BASDAI, and (E) high ASDAS. BASFI, Bath Ankylosing Spondylitis Functionality Index; CRP, C-reactive protein.
This analysis of cross-sectionally evaluated patients with AS in daily clinical practice describes the profile of patients who would be selected for anti-TNF therapy if different disease activity instruments were used. The purpose of this hypothesis-generating research was to evaluate which disease activity measure and threshold criterion would select the population that is most likely to have characteristics that have been associated with response to anti-TNF treatment in the literature. The data show that more patients have high ASDAS than elevated BASDAI, and compared to those selected with high BASDAI, patients selected with high ASDAS more frequently have disease characteristics that have a documented association to good response to anti-TNF therapy.9
The selection of patients for anti-TNF therapy is not an easy decision. The BASDAI instrument is currently the main driver to select candidates to receive anti-TNF therapy in AS, but positive expert opinion clinical based in clinical judgment based on disease characteristics is also very important.1–3 In this study, we highlight that the BASDAI instrument may exclude a certain proportion of patients that (1) have high disease activity according to another instrument (i.e. the ASDAS activity index), (2) show characteristics that have been associated to good outcome to anti-TNF therapy in the literature, and (3) may correspond with a patient profile that a clinician may think is appropriate for anti-TNF treatment (e.g., a young patient with high disease activity, high CRP, and HLA-B27-positive status). In the current study, 37% of patients who had low disease activity according to the BASDAI criterion had high disease activity according to the ASDAS; if BASDAI was used as a strict criterion for determining eligibility for treatment, none of these patients would be eligible for anti-TNF treatment. The use of high ASDAS as a selection criterion instead of elevated BASDAI would increase the number of treatment candidates. Patients selected with elevated ASDAS but not elevated BASDAI had a combination of disease characteristics that are associated with positive outcomes in published studies (represented in green in Fig. 1B).4–9 Very few patients had high BASDAI and low ASDAS and would not be selected with the high ASDAS criterion (represented in red in Fig. 1B); these patients tend to have characteristics that may not be associated with good outcomes. Good selection criteria for treatment in clinical practice would ideally select future responders as treatment candidates, and select against patients who are not likely to respond to treatment.
Whether selection is based on elevated BASDAI or high ASDAS, a number of patients who would be selected have combined characteristics that are associated with low probability of response. This indicates that the recommendation to use clinical characteristics (in addition to a disease activity criterion) to guide choice of therapy remains important. Predictors of response such as the ones described can be helpful tools to complement the elevated ASDAS criterion for patient selection. In clinical practice, a rheumatologist may wonder whether there is a good reason to use anti-TNF treatment in an older HLA-B27-negative patient who reports poor function and high disease activity, despite absence of objective signs of inflammation (i.e., CRP<0.6mg/dL); this profile corresponds with that of 24/1156 REGISPONSER patients. From a societal perspective, payers may want to evaluate whether it is worth excluding patients with such characteristics to allow treating a group of HLA-B27-positive patients younger than 40 years of age with high disease activity and CRP greater than 2mg/dL who still have preserved function (this profile corresponds with 23/1156 REGISPONSER patients). Thus, using BASDAI as the only criterion to decide anti-TNF treatment could exclude the latter group to be treated with anti-TNF therapy in many European countries, and this is why expert opinion and clinical judgment based on patient's characteristics and biochemical markers like CRP levels or HLA-B27 status is critical in the decision.
Compared to selection with BASDAI, more patients are selected for anti-TNF treatment when high ASDAS is used and fewer patients are selected when very high ASDAS is the selection criterion. Because BASDAI and BASFI are highly correlated, selection with high BASDAI automatically leads to a selection of patients who fall in the higher categories for BASFI. Replacing BASDAI with ASDAS leads to an increase of the proportion of patients in the lower BASFI category, which is associated with better response. The advantageous CRP profile (higher CRP is associated with better response) that is seen for a population with very high ASDAS is largely offset by the disadvantageous BASFI profile (higher BASFI is associated with worse response). The data show that patients with very high ASDAS also have a higher likelihood of enthesitis, which is associated with slightly worse outcomes.9 In addition to leading to a more favorable CRP and BASFI profile, selection with high and very high ASDAS also results in a younger population, even though age is not an explicit component of the ASDAS. Because younger patients tend to respond better, this finding is relevant for patient selection in practice. The overall decrease in number of patients who can be treated and the profile of patients no longer selected if BASDAI is replaced by very high ASDAS indicates that the latter selection criterion may not be an improvement over the former. However, replacing BASDAI with high ASDAS may need to be considered for future recommendations. In fact, in a recent study, a small group of patients with high ASDAS and normal BASDAI (n=48) have shown to respond to anti-TNF therapy,16 and these patients would have been excluded from anti-TNF therapy if high BASDAI would have been used as strict selection criterion.
The main limitation of the study is its cross-sectional design with no follow-up, which precludes validating the findings of the study by assessing the response to anti-TNF therapy in groups of patients with the abovementioned characteristics. We did not get specific information on individual components of BASDAI and ASAS indexes; thus, we cannot display BASDAI and ASAS component-per-component values to check which items contribute to the discordance in the high ASAS/low BASDAI group. Another limitation is that some 15% of patients were already treated with anti-TNF agents, and this may have had an influence on BASDAI and ASDAS as well as some of the relevant disease characteristics (e.g. CRP and BASFI). It is difficult to say how this has an influence on the results. Although higher ASDAS has been associated with better outcomes,8 it is important to emphasize that the database did not allow confirmation of whether the response was indeed higher in patients selected with ASDAS versus BASDAI. Because the efficacy of anti-TNF treatment in patients with high ASDAS and BASDAI less than 4 has never been studied, except in a small group of patients,16 it is not certain whether the favorable disease characteristic profile described here is also related to better outcomes in that patient group. Further investigation on the response to anti-TNF in a larger population with high ASDAS/low BASDAI is needed.
In conclusion, in this cross-sectional study, selection of AS patients with the ASDAS instrument results in patient sub-populations that have different characteristics than those selected with the BASDAI instrument. Since some of these characteristics have been associated with good outcome to anti-TNF therapy, the hypothesis generated through this research is that replacing the disease activity measure in anti-TNF treatment recommendations from BASDAI to ASDAS may lead to better outcomes of therapy. This hypothesis should be tested in prospective studies.
Ethical responsibilitiesProtection of people and animalsThe authors declare that no experiments were performed on humans or animals for this investigation.
Data confidentialityThe authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consentThe authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Funding statementREGISPONSER was funded by an unrestricted grant by the Spanish Foundation of Rheumatology (FER) thanks to the financial collaboration of Abbott, Schering-Plough, and Wyeth. The funding for the analysis reported here was provided by Merck.
ContributorsAll authors participated in the analysis and interpretation of data and manuscript preparation and approved the final manuscript for submission.
Conflict of interest statementNathan Vastesaeger is employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc. All other authors have declared no conflicts of interest.
The authors thank all the REGISPONSER patients and investigators. The authors thank all the REGISPONSER patients and investigators. Ellen Stoltzfus, PhD, JK Associates, Inc., Conshohocken, Pennsylvania, USA, provided editorial support in the preparation of this manuscript. This support was funded by Merck. We thank Luis Cea-Calvo, MD, from Medical Affairs, Merck Sharp & Dohme, Spain, for comments to the final version of the manuscript.