The aim of this study was to identify the associated factors with lower self-esteem and restriction in community reintegration in SpA patients.
MethodsThis study was a cross-sectional study including SpA patients (ASAS criteria) aged 18–50 years. The level of self-esteem was assessed using the Rosenberg Self-Esteem Scale (RSES). The Reintegration to Normal Living Index (RNLI) evaluated the degree of reintegration to normal social activities. Anxiety, depression, and fibromyalgia were screened by the Hospital Anxiety and Depression Scale (HADS)-A, HADS-D, and FiRST, respectively. Statistical analysis was performed.
ResultsA total of 72 patients were enrolled (sex-ratio=1.88), with median (IQR) age of 39 years (28.25–46). Median (IQR) disease duration was 10 (6–14) years. Median (IQR) BASDAI and ASDAS were 3 (2.1–4.7) and 2.7 (1.9–3.48), respectively. Anxiety symptoms were screened in 10% of SpA patients, depression in 11%; and fibromyalgia in 10%. Median (IQR) RSES and RNLI scores were 30 (23.25–34), and 83 (53.25–93.25), respectively. Multivariate regression analysis identified the domain (work) of pain interference, VAS pain, HAD anxiety, PGA, marital status, and morning stiffness as factors associated with lower self-esteem. Restriction in the reintegration community was predicted by the presence of IBD, VAS pain, FIRST, deformity, enjoyment of life, and HAD depression.
ConclusionPain intensity and interference, deformities, extra-articular manifestations, and deterioration of mental health were associated with low self-esteem and severe restriction in community reintegration among patients with SpA rather than inflammatory parameters.
El objetivo de este estudio fue identificar el factor asociado a la baja autoestima y la restricción en la reintegración comunitaria en pacientes con espondiloartritis (EspA).
MétodosEste estudio fue un estudio transversal llevado a cabo incluyendo a pacientes con EspA (criterios ASAS) de entre 18 y 50 años de edad. El nivel de autoestima se evaluó mediante la Rosenberg Self-Esteem Scale (RSES). El Reintegration to Normal Living Index (RNLI) evaluó el grado de reintegración a las actividades sociales normales. La ansiedad, la depresión y la fibromialgia se evaluaron mediante la Hospital Anxiety and Depression Scale (HADS)-A, HADS-D y FIRST, respectivamente. Se realizó un análisis estadístico.
ResultadosSe inscribieron 72 pacientes (razón por sexo: 1,88), con una mediana (IQR) de edad de 39 años (28,25-46). La IQR de la duración de la enfermedad fue de 10 (6-14) años. La IQR de BASDAI y ASDAS fue de 3 (2,1-4,7) y 2,7 (1,9-3,48), respectivamente. Se detectaron síntomas de ansiedad en el 10% de los pacientes con EspA, depresión en el 11% y fibromialgia en el 10%. La IQR de las puntuaciones RSES y RNLI fue de 30 (23,25-34) y 83 (53,25-93,25), respectivamente. El análisis de regresión multivariante identificó el dominio (trabajo) de la interferencia del dolor, el dolor VAS, la ansiedad HAD, la PGA, el estado civil y la rigidez matinal como factores asociados a una menor autoestima. La restricción en la comunidad de reintegración se predijo por la presencia de EII, el dolor VAS, la herramienta FIRST, la deformidad, el disfrute de la vida y la depresión HAD.
ConclusionesLa intensidad y la interferencia del dolor, las deformidades, las manifestaciones extra-articulares y el deterioro de la salud mental se asociaron a una baja autoestima y de una severa restricción en la reintegración a la comunidad entre los pacientes con EspA más que los parámetros inflamatorios.
Spondyloarthritis (SpA) is a chronic inflammatory disease that encapsulates a group of conditions sharing similar clinical and radiological characteristics.1 They involve the axial skeleton and sacroiliac joints as well as peripheral joints. The course of SpA is usually progressive, characterized by chronic pain, spinal deformity, and mobility impairment, leading to disability, reduced quality of life (QoL), anxiety, and depression.2,3 SpA usually affects the young population when body image, social relationships, career, leisure, and social roles are prominent.1 Therefore, SpA patients have challenges in maintaining positive self-esteem and community reintegration.
Self-esteem is a term used in psychology to describe a person's perception of their own worth.4 It is the overall positive or negative judgment that a person makes about himself. Self-esteem has been identified as a determinant of well-being.4 In fact, positive self-esteem was found to be significantly associated with emotional stability and better QoL.5,6 Few studies investigated the relationship between rheumatic diseases and self-esteem. Jorge et al.7 demonstrated that self-esteem was significantly lower in patients with rheumatoid arthritis compared to control group. Studies on self-esteem among patients with SpA are rare.8 However, it is an important outcome to investigate in order to improve the QoL of SpA patients.
On the other side, community reintegration is defined as full participation in community. It involves social relationships, work, leisure, and daily activities. Community reintegration is a commonly used concept to evaluate participation after a debilitating illness.9–11 Patients with SpA reported more difficulties when participating in roles compared to control group.12
The aim of this study was to investigate the associated factors with lower self-esteem and restriction in community reintegration among SpA patients.
MethodsStudy designThis study was a cross-sectional study conducted over a 6-month period [September 2021–March 2022], involving patients diagnosed with SpA (either peripheral or axial) based on the criteria of the Assessment of Spondyloarthritis International Society (ASAS).13,14 The study was approved by the local hospital ethical committee. Written informed consent was obtained from participants after the aims of the research had been explicitly explained to each patient.
PatientsPatients aged 18–50 years were consecutively recruited from the rheumatology outpatient and/or daycare hospital. Non-inclusion criteria were: history of psychotic illness, alcohol and/or drug abuse, current treatment with psychotropics, comorbidities (diabetes mellitus, cardiovascular disease, active or chronic infection, and cancer), or other concomitants chronic or inflammatory diseases.
Data collectionSocio-demographic data: age, gender, marital status, number of children, educational level (illiterate, primary, secondary, university), employment status, and living arrangement (urban or rural areas) were collected. Disease-specific information including age at onset of SpA, disease duration, axial or peripheral form, coxitis, and extra-articular features were recorded. The presence of articular or axial deformity was recorded by a ‘yes’ or ‘no’ answer based on physical examination at the time of enrollment.
Patient-Reported Outcomes (PRO) were measured: duration of morning stiffness, number of nocturnal awakenings, Patient Global Assessment (PGA), and intensity of pain and fatigue. Each patient recorded the severity of pain and fatigue on a visual analog scale (VAS) from 0 to 10 (0: no pain/fatigue, 10: worst imaginable pain/fatigue). Disease activity was assessed using Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), Ankylosing Spondylitis Disease Activity Score (ASDAS), and C-Reactive Protein (CRP) level. The impact of SpA on quality of Life and functional ability were assessed using the Ankylosing Spondylitis Quality of Life (ASQoL) Scale, and the Bath Ankylosing Spondylitis Functional Index (BASFI), respectively.
Medications were determined from participants’ self-reports: non-steroidal anti-inflammatory drugs (NSAIDs), conventional disease-modifying antirheumatic drugs (csDMARDs), and tumor necrosis factor inhibitors (TNFi).
MeasurementsSelf-esteemRosenberg Self-Esteem Scale (RSES): the Arabic version of RSES was used to assess the level of self-esteem among SpA patients.4,15 Each item is rated on a 4-point scale (1: strongly disagree, 4: strongly agree).
The questionnaire consisted of 10 items, 5 of which assessed positive self-esteem and 5 assessed negative self-esteem (items 3, 5, 8, 9, and 10). The scale was computed by rescaling the negative questions (reverse scored) and then adding the ten scores. The total self-esteem score ranges from 10 to 40, with higher values indicating higher self-esteem levels.
Community reintegrationReintegration to Normal Living Index (RNLI): is a patient-reported outcome that measures the degree to which individuals achieve reintegration to normal social activities.16 The RNLI is an 11-item scale, with 2 areas of assessment: daily functioning (the first 8 items) and perceptions of self (the remaining 3 items represent). The RNLI assessed 8 domains: indoor mobility, community/distance mobility, self-care, daily activities (work and school), recreational and social activities, family roles, personal relationships, and presentation of self to others. Each item is rated on a 10-point VAS, with a score of 0 indicating “no reintegration” and 10 indicating “full reintegration”. The sum of the scores was normalized to 100; the minimum possible total score is 0 and the maximum is 100, indicating no or full integration, respectively. The higher the score, the better the patient-perceived community reintegration was. RNLI score <60 reflected severe restrictions in self-perceived community reintegration. The RNLI has been recommended for use in measuring participation restriction among people with different illnesses, and has demonstrated excellent validities and reliabilities with high utility.17,18
Anxiety and depressionAnxiety and depression were screened using the two subscales of Hospital Anxiety and Depression Scale (HADS): HADS-A and HADS-D, respectively.19 Each subscale contains seven items on a four-point Likert scale (ranging from 0 to 3) to assess anxiety and depression. The total score ranges from 0 to 21 points for each subscale, and a score of 11 or higher indicates the presence of anxious or depressive disorders.
Pain interferenceBrief Pain Inventory (BPI) was used to assess the level of pain interference (PI) in the past week on the following 7 domains: general activity, mood, walking, work, relations with others, sleep, and enjoyment of life.20 Pain interference (PI) describes the influence of pain on daily living and is distinct from pain severity and other characteristics of pain.
FibromyalgiaFibromyalgia Rapid Screening Test (FiRST): is a self-report questionnaire containing six questions. A score≥5/6 indicates positive screening test for fibromyalgia.21
Statistical analysisData were analyzed using the Statistical Software for the Social Sciences (SPSS) version 25. Baseline descriptive of the SpA cohort was expressed as frequencies, percentages, median with interquartile range between the 25th and 75th percentiles (IQR). Mann–Whitney U test and Kruskal–Wallis H test were used to compare two variables, and more than 3 variables, respectively. Correlation between patients/disease-related parameters and RLNI/self-esteem was assessed using Spearman's correlation. Multiple linear regression was performed to identify the associated factors with low scores of self-esteem and community reintegration among our SpA-patients sample. We used the “Enter” method; variables with a significance level of p<0.2 in univariate linear regression were selected into the multiple linear regression model. The final model was selected on the basis of a good quality of the regression model (a good R2 with significant p-values), and after checking the collinearity between variables. Model validation was conducted with the Durbin–Watson residual study. The confidence interval was estimated at 95% and statistical significance was indicated by a p value<0.05.
ResultsA total of 72 patients (sex-ratio=1.88) participated in the present study, with a median (IQR) age was 39 years (28.25–46). The Median (IQR) number of children was 0 (0–2). Table 1 illustrates patients’ baseline socio-demographic characteristics. Median (IQR) disease duration was 10 (6–14) years. Among enrolled patients, 27.3% and 65% had active disease according to BASDAI and ASDAS-CRP, respectively. Disease characteristics are detailed in Tables 1 and 2.
Patient and disease parameters (categorical data).
| Variable | Class | N | % |
|---|---|---|---|
| Gender | Female | 25 | 34.7 |
| Male | 47 | 65.3 | |
| Marital status | Single | 24 | 37.5 |
| Married | 39 | 60.9 | |
| Divorced | 1 | 1.6 | |
| Occupation | Student | 4 | 5.9 |
| Unemployed | 11 | 16.2 | |
| Housekeeper | 16 | 23.5 | |
| Civil/private sector | 33 | 48.5 | |
| Self-employed | 4 | 5.9 | |
| Location | Rural | 10 | 15.2 |
| Urban | 56 | 84.8 | |
| Educational level | Illiterate | 6 | 9.2 |
| Primary | 18 | 27.7 | |
| Secondary | 34 | 52.3 | |
| University | 7 | 10.8 | |
| Spondyloarthritis form | Axial | 35 | 48.6 |
| Axial and peripheral | 34 | 47.2 | |
| Peripheral | 3 | 4.2 | |
| Deformity articular/axial | No | 56 | 77.8 |
| Yes | 16 | 22.2 | |
| Psoriasis | No | 66 | 91.7 |
| Yes | 6 | 8.3 | |
| Inflammatory Bowel disease | No | 65 | 90.3 |
| Yes | 7 | 9.7 | |
| Coxitis | No | 34 | 47.2 |
| Yes | 38 | 52.8 | |
| Treatment | NSAIDs | 52 | 72.2 |
| TNFi | 37 | 51.4 | |
Patient and disease parameters (quantitative data).
| Variable | Median (IQR 25–75%) | Min | Max |
|---|---|---|---|
| Age at onset of SpA (years) | 21 (18–34) | 0 | 47 |
| Disease duration (years) | 10 (6–14) | 1 | 34 |
| VAS pain | 5 (3.5–6.5) | 1.00 | 9 |
| PGA | 5 (4–7) | 0 | 9 |
| VAS fatigue | 4 (2–6) | 0 | 9 |
| Morning stiffness (minutes) | 10 (1–20) | 0 | 180 |
| Number of nocturnal awakenings | 0 (0–2) | 0 | 10 |
| BASDAI | 3 (2.1–4.7) | 0.2 | 7 |
| ASDAS CRP | 2.7 (1.9–3.48) | 0.32 | 7 |
| BASFI | 3.5 (1.8–5.1) | 0.4 | 9.2 |
| ASQoL | 6 (3–10) | 0 | 18 |
| CRP (mg/l) | 11.5 (3.18–25) | 0 | 257 |
| HADS anxiety | 3 (2–8) | 0 | 15 |
| HADS depression | 5 (3–8) | 0 | 13 |
| BPI pain interference | |||
| General activity | 4 (2–6) | 0 | 8 |
| Mood | 4 (2–6) | 0 | 8 |
| Walking | 3 (2–5) | 0 | 9 |
| Work | 3 (2–5) | 0 | 10 |
| Relations with others | 2.5 (1–5) | 0 | 8 |
| Sleep | 3 (2–5) | 0 | 9 |
| Enjoyment of life | 3 (2–5) | 0 | 8 |
| FiRST | 2 (1–3) | 0 | 6 |
| RSES | 30 (23.25–34) | 10 | 40 |
| RLNI | 83 (53.25–93.25) | 0 | 110 |
ASDAS: Ankylosing Spondylitis Disease Activity Score; BASDAI: Bath Ankylosing Spondylitis Disease Activity index; BASFI: Bath Ankylosing Spondylitis functional index; CRP: C reactive protein; Max: maximum; Min: minimum; PGA: patient global assessment; VAS: visual analog scale; SpA: spondyloarthritis; ASQoL: Ankylosing Spondylitis Quality of Life Scale; RSES: Rosenberg Self-Esteem Scale; RLNI: The Reintegration to Normal Living Index; HADS: Hospital Anxiety and Depression Scale; BPI: The Brief Pain Inventory; FiRST: Fibromyalgia Rapid Screening Test.
Median (IQR) HAD-A and HAD-D were 3 (2–8) and 5 (3–8), respectively. According to HAD, 10% of SpA patients presented anxiety disorders and 11% presented depression. Ten percent had positive screening for fibromyalgia. Median (IQR) total self-esteem score was 30 (23.25–34). Median (IQR) RNLI score was 83 (53.25–93.25) (Table 2) and 15.5% of patients indicated severe restrictions in self-perceived community reintegration.
Bivariate analysis (Tables 3 and 4)Self-esteemCorrelation between RSES and patient-related parameters revealed negative correlation with marital status (p=0.021; r=−0.287), number of children (p=0.039; r=−0.259), HAD anxiety (p=0.001; r=−0.379) and HAD depression (p<0.0001; r=−0.46). Single patients had higher RSES scores. Regarding disease related parameters, RSES was negatively correlated with VAS pain (p=0.048; r=−0.239), BASDAI (p=0.034; r=−0.254), ASQoL (p=0.002; r=−0.363) and BASFI (p=0.035; r=−0.258). Median RSES was higher among SpA patients treated with TNFi compared with those who were treated with NSAIDs (p=0.044).
Bivariate analysis of quantitative variables with RLNI & RSES.
| RSES | RLNI | |||
|---|---|---|---|---|
| Continuous variables | r | p | r | p |
| Age | 0.010 | 0.933 | 0.152 | 0.246 |
| Educational level | −0.045 | 0.720 | 0.025 | 0.855 |
| Marital status | −0.287 | 0.021 | 0.088 | 0.521 |
| Location | 0.112 | 0.369 | 0.249 | 0.062 |
| Occupation | 0.021 | 0.866 | 0.081 | 0.541 |
| Number of children | −0.259 | 0.039 | −0.041 | 0.766 |
| HADS anxiety | −0.379 | 0.001 | −0.377 | 0.003 |
| HADS depression | −0.460 | <0.0001 | −0.588 | <0.0001 |
| Age at onset of SpA | 0.012 | 0.923 | 0.140 | 0.300 |
| Disease duration | −0.206 | 0.085 | 0.171 | 0.191 |
| BASDAI | −0.254 | 0.034 | −0.182 | 0.172 |
| ASDAS CRP | −0.005 | 0.969 | −0.095 | 0.493 |
| CRP | 0.031 | 0.805 | −0.027 | 0.846 |
| ASQoL | −0.363 | 0.002 | −0.464 | <0.0001 |
| BASFI | −0.258 | 0.035 | −0.191 | 0.158 |
| VAS pain | −0.239 | 0.048 | −0.120 | 0.369 |
| VAS Fatigue | −0.234 | 0.069 | 0.038 | 0.784 |
| BPI pain interference | ||||
| General activity | −0.194 | 0.108 | −0.377 | 0.004 |
| Mood | −0.271 | 0.024 | −0.380 | 0.004 |
| Walking | −0.178 | 0.140 | −0.233 | 0.079 |
| Working | −0.351 | 0.003 | −0.211 | 0.115 |
| Relations with others | −0.231 | 0.054 | −0.276 | 0.036 |
| Sleep | −0.205 | 0.089 | −0.442 | 0.001 |
| Enjoyment of life | −0.139 | 0.251 | −0.354 | 0.006 |
| FiRST | −0.214 | 0.073 | 0.271 | <0.0001 |
ASDAS: Ankylosing Spondylitis Disease Activity Score; BASDAI: Bath Ankylosing Spondylitis Disease Activity index; BASFI: Bath Ankylosing Spondylitis functional index; CRP: C reactive protein; VAS: visual analog scale; SpA: spondyloarthritis; ASQoL: Ankylosing Spondylitis Quality of Life Scale; RSES: Rosenberg Self-Esteem Scale; RLNI: The Reintegration to Normal Living Index; HADS: Hospital Anxiety and Depression Scale; BPI: The Brief Pain Inventory; FiRST: Fibromyalgia Rapid Screening Test.
Bivariate analysis of categorical variables with RLNI & RSES.
| RLNI | RSES | |||
|---|---|---|---|---|
| Median | p | Median | p | |
| Gender | 0.842 | 0.056 | ||
| Male | 81 | 32 | ||
| Female | 87 | 24 | ||
| SpAform | ||||
| Axial | 86 | 0.377 | 28 | 0.481 |
| Axial and peripheral | 79 | 32 | ||
| Peripheral | 87 | 30 | ||
| Coxitis | 0.830 | 0.928 | ||
| No | 86 | 30 | ||
| Yes | 80 | 31 | ||
| Psoriasis | 0.119 | 0.450 | ||
| No | 85 | 30 | ||
| Yes | 0 | 33 | ||
| IBD | 0.014 | 0.121 | ||
| No | 86 | 30 | ||
| Yes | 0 | 34 | ||
| TNFi | 0.379 | 0.044 | ||
| No | 86 | 29 | ||
| Yes | 79 | 32 | ||
IBD: inflammatory Bowel disease; TNFi: Tumor Necrosis Factor inhibitor; SpA: spondyloarthritis; RSES: Rosenberg Self-Esteem Scale; RLNI: The Reintegration to Normal Living Index.
Among the pain interference items, mood and ability to work normally items were negatively correlated with RSES (p=0.024; r=−0.271, and p=0.003; r=−0.351, respectively).
Community reintegration (Tables 3 and 4)Concerning disease-related parameters, RNLI score was significantly lower in SpA with inflammatory bowel disease (IBD) (p=0.014).
RLNI was negatively correlated with ASQoL (p<0.0001; r=−0.464), HAD anxiety (p=0.003; r=−0.377), HAD depression (p<0.0001; r=−0.588), First test (p<0.0001; r=−0.479), and the following domains of PI: general activity (p=0.004; r=−0.377), mood (p=0.004; r=−0.38), relations with others (p=0.036; r=−0.276), sleep (p=0.001; r=−0.442), and enjoyment of life (p=0.006; r=−0.354).
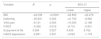
Multivariate analysis (Tables 5 and 6)Multivariate regression showed that the combination of the domain “work” of PI, VAS pain, HAD anxiety, PGA, marital status, and morning stiffness explained 47.7% of the variance of RSES.
Multivariate analysis of self-esteem in spondyloarthritis.
| Factor | B | p | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Work domain | −1.411 | <0.0001 | −2.155 | −0.667 |
| VAS pain | 1.820 | 0.001 | 0.810 | 2.829 |
| HADS anxiety | −0.685 | 0.001 | −1.076 | −0.293 |
| PGA | −1.218 | 0.005 | −2.041 | −0.395 |
| Marital status | −3.258 | 0.021 | −6.002 | −0.515 |
| Morning stiffness | 0.056 | 0.031 | 0.005 | 0.107 |
VAS: visual analog scale; HADS: Hospital Anxiety and Depression Scale; PGA: patient global assessment.
Multivariate analysis of community reintegration in spondyloarthritis.
| Variable | B | p | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| IBD | −43.039 | <0.0001 | −63.800 | −22.279 |
| Deformity | −25.831 | 0.002 | −41.700 | −9.962 |
| VAS pain | −6.121 | 0.003 | −10.053 | −2.188 |
| FiRST | −5.306 | 0.019 | −9.710 | −0.901 |
| Enjoyment of life | 3.594 | 0.027 | 0.435 | 6.752 |
| HADS depression | −2.851 | 0.001 | −4.523 | −1.179 |
IBD: inflammatory bowel disease; VAS: visual analog scale; HADS: Hospital Anxiety and Depression Scale; FiRST: Fibromyalgia Rapid Screening Test.
Reintegration community variance could be explained in 64.8% by the following associated factors: IBD, VAS pain, FIRST, deformity, enjoyment of life, and HAD depression. The presence of IBD was the strongest associated factor with severe restriction in community reintegration.
DiscussionIn the present study, median (IQR) RSES and RNLI scores were 30 (23.25–34), and 83 (53.25–93.25), respectively. Severe restrictions in self perceived community reintegration were seen in 15.5%. Associated factors with decreased self-esteem and restrictions in community reintegration were disease-related parameters (prolonged morning stiffness, the presence of articular/axial deformity, and IBD), psychological factors (anxiety and depressive disorders, fibromyalgia), severe pain intensity and interference (enjoyment of life, pain in work), and social factors (divorced status).
Studies on self-esteem among patients with SpA are sparse. In line with our results, Solmaz et al. and Durmus D et al.8,22 observed lower self-esteem score in ankylosing spondylitis group compared to control group. In fact, patients with chronic rheumatic disease face challenges in maintaining positive self-esteem.7,23
Concerning perceived participation, different self-reported questionnaires can be used. The RLNI is a brief questionnaire developed for assessing reintegration to normal living after a disabling illness. The concept of reintegration was used to evaluate perceived participation.24 Studies in the literature used the social role participation questionnaire (SRPQ) to evaluate social role participation among patients with SpA across two dimensions (experienced physical difficulties and satisfaction with performance).12,25–29 Van Genderen et al.12 noted that patients with SpA were less satisfied with their performance in roles and had more difficulties when participating in roles compared to control group.
When looking at associated factors with declined self-esteem and severe restriction in community reintegration identified in our study, mental health symptoms appeared to explain low self-acceptance. Anxiety and depression are frequent psychological disorders in SpA patients.30,31
As previously reported in the literature, depression was correlated with low satisfaction in participation.25,27,28 Both experienced physical difficulties and satisfaction with role performance were significantly associated with the mental health item of the Short Form-36 Health Survey (SF-36).27,28
Moreover, studies that have focused on body image among patients with SpA demonstrated a strong link between a positive body image and a high self-esteem.8,23,32 A Chinese study showed a significant association between self-esteem and anxiety through the impact of body image disturbance on anxiety.33 Best predictors for impaired health-related QoL in the dimension self-esteem were social isolation and depression/anxiety in children and adolescents with juvenile idiopathic arthritis and reactive arthritis.34
To our knowledge, this is the first study to identify a high FiRST score as an associated factor with restricted community reintegration. In a recent meta-analysis, the prevalence of fibromyalgia was 16.4% among a total of 5214 SpA patients.35 It has been proven that fibromyalgia among SpA patients negatively affects disease activity, functional status, pain level, QoL and mental health.36–38 Thus, fibromyalgia may impact community reintegration through mental health symptoms.
Regarding pain, severe pain intensity and interference were associated factors with low self-esteem and restriction in community reintegration. This was consistent with the literature findings.23,39 Bagcivan et al.39 confirmed the negative impact of chronic pain on restricted participation including daily life activities, family responsibilities, and work in SpA patients. Patients living with chronic pain are more likely to suffer from anxiety, depression, emotional distress and low self-esteem.39
Work item of PI was an associated factor with lower self-esteem, which can be explained by the decline of work productivity due to the impact of chronic pain. Self-esteem may be disrupted in the context of lost employment, as showed Barlow JH et al. that work disability was associated with anxious and depressed mood and lower self-esteem in SpA.40 In fact, SpA can be the cause of low work productivity and impairment leading to limitation in career progress in some patients and therefore to low self-esteem.41–43 Work productivity and impairment were correlated to disease status, QoL, and intensity of pain.41,42
When looking at disease-related parameters, prolonged morning stiffness, axial/peripheral deformity, and IBD were the associated factors with a low self-esteem and community reintegration. The presence of IBD was the strongest associated factor with severe restriction in community reintegration. IBD are characterized by the occurrence of abdominal pain with diarrhea and a relapsing clinical course. In a recent systematic review and meta-analysis, QoL scores were lower in patients with IBD compared to control group.44 Patients with IBD presented as well high rates of anxiety and depression.45
Physical deformity may affect the patient's self-esteem and community participation through its impact on body image and mental health symptoms. These finding was reported in RA patients.46 Patients with physical deformity (axial skeleton or peripheral joint) tried to conceal their deformity especially in work and social situations. Masking and concealing illness from others produced negative feelings as of shame and guilt around various aspects of self-managing the condition. Self-confidence may be reduced when the person compares their current and past functioning or participation, his social activity progressively decreases, which alters their community reintegration. Therefore, social and emotional learning must be an important part of the work of self-management for patients with rheumatic inflammatory diseases.
In concordance with our results, Bode et al.23 noted a significant correlation of self-esteem with functional impairment among patients with rheumatic diseases including SpA and rheumatoid arthritis.
RSES was significantly higher among patients with TNFi. In fact, TNFi are very effective and lead to improvement in pain, disease activity, spinal mobility, and thus the QoL of patients with SpA.47,48
This is the first study to investigate the associated factors with self-esteem and community reintegration among patients with SpA. However, this study has some limitations. The single-center study design may not be representative of SpA in our country. A multi-centric study is required to generalize our findings. The cross-sectional design of the study and the lack of a control group do not allow to prove the causality. Besides, despite being significative, some correlations were quite poor.
ConclusionIn summary, pain intensity and interference, deformities, extra-articular manifestations (IBD) and deterioration of mental health were associated with low self-esteem and severe restriction in community reintegration among patients with SpA rather than inflammatory parameters. These results suggest a relevant role of psychosocial aspects in SpA patient outcome, which should alert physicians to the need of a holistic approach of the patient. Specific management of different pain components is required to improve health-related quality of life. Screening of mental health symptoms enables us to refer SpA patients for a personalized personal development program with social and emotional learning to enhance self-esteem, self-acceptance and promote community reintegration.
FundingNone to declare.
Conflict of interestThe authors declare that they have no conflict of interest.