We read with high respect the recent publication of the Mexican Clinical Practice guidelines for the management of systemic lupus erythematosus (SLE).1 This is a much-needed reference for Mexico, a country with a high number of SLE patients. From the nephrologist perspective, lupus nephritis (LN) is also of great concern to Latin America given the high percentage of LN observed in recent renal biopsy registries from the region.2 It is known that LN affects 40–60% of patients with SLE and 10–20% will progress to end-stage renal disease within 10 years of diagnosis. These patients will receive some sort of renal replacement therapy (RRT): peritoneal dialysis (PD), hemodialysis (HD) or renal transplantation.3
In the LN management section, these new recommendations suggest “hemodialysis (HD) as the first option of renal replacement treatment in patients with chronic kidney disease (CKD) due to LN, given that peritoneal dialysis (PD) is associated with a higher number of complications and mortality due to immunosuppression (quality of evidence: moderate, strong recommendation)”.
Studies in the nephrology community comparing patient survival on hemodialysis versus peritoneal dialysis in patients with end-stage renal disease from several etiologies have yielded conflicting results. Some underlying reasons encompass the differences in the included populations (e.g. incident vs. prevalent, diabetic vs. non-diabetic), differences in the methodology used (e.g. intention to treat vs. received dialysis modality) and importantly, the unavailability of complete information of important confounders (presence or severity of comorbidities, residual kidney function, administered dialysis dose, among others). Researchers have tried to overcome these difficulties with the use of multivariate modeling, multilevel modeling or the use of propensity scores. However, confounding remains a threat to validity of most studies.
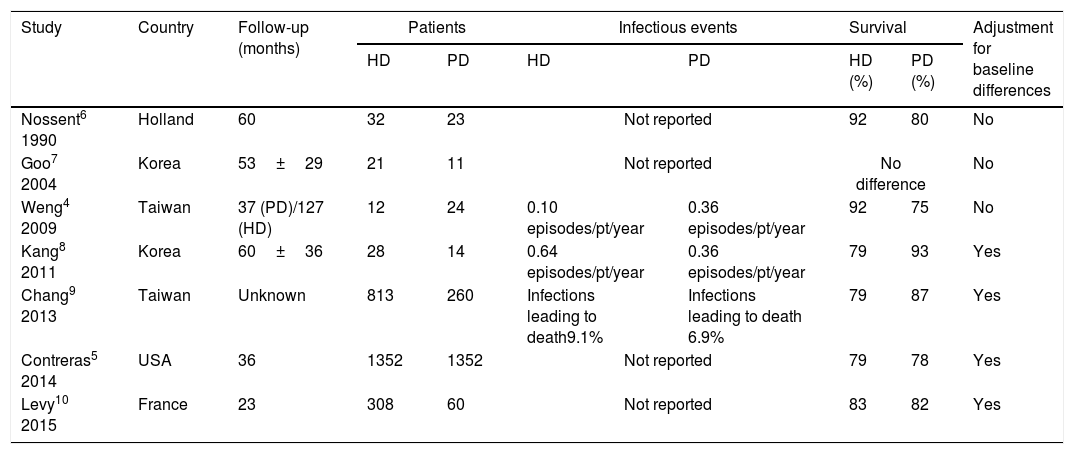
The recommendation in these new guidelines is based on the study by Weng et al. from Taiwan.4 This is a small observational report that found a higher number of infections and death among 24 SLE patients undergoing PD as compared to 12 SLE patients on HD. The study has multiple methodological limitations, the most notable being the absence of correction for the baseline differences with any of the aforementioned statistical techniques. Some other important limitations are mentioned in the manuscript's discussion, for example, the health system in Taiwan did not cover erythropoietin stimulating agents (ESAs) for PD patients as it did for the HD group. Several other studies have been performed to define the best dialytic modality for SLE patients, some of them with similar methodological limitations (Table 1).
Studies comparing hemodialysis (HD) and peritoneal dialysis (PD) modalities in systemic lupus erythematosus patients on end-stage renal disease.
| Study | Country | Follow-up (months) | Patients | Infectious events | Survival | Adjustment for baseline differences | |||
|---|---|---|---|---|---|---|---|---|---|
| HD | PD | HD | PD | HD (%) | PD (%) | ||||
| Nossent6 1990 | Holland | 60 | 32 | 23 | Not reported | 92 | 80 | No | |
| Goo7 2004 | Korea | 53±29 | 21 | 11 | Not reported | No difference | No | ||
| Weng4 2009 | Taiwan | 37 (PD)/127 (HD) | 12 | 24 | 0.10 episodes/pt/year | 0.36 episodes/pt/year | 92 | 75 | No |
| Kang8 2011 | Korea | 60±36 | 28 | 14 | 0.64 episodes/pt/year | 0.36 episodes/pt/year | 79 | 93 | Yes |
| Chang9 2013 | Taiwan | Unknown | 813 | 260 | Infections leading to death9.1% | Infections leading to death 6.9% | 79 | 87 | Yes |
| Contreras5 2014 | USA | 36 | 1352 | 1352 | Not reported | 79 | 78 | Yes | |
| Levy10 2015 | France | 23 | 308 | 60 | Not reported | 83 | 82 | Yes | |
HD, hemodialysis; PD, peritoneal dialysis; episodes/pt/year, infectious episodes per patient per year (current recommendation is <0.6 dialysis related episodes/patient/year for peritoneal dialysis).
The largest study to date that compared PD vs. HD in SLE patients was performed by Contreras et al.5 with data from the US Renal Data System. In this study, 1352 SLE patients with PD were matched with a propensity score approach to 1352 SLE patients with HD. There was a similar 3-year mortality between both modalities (21.4% vs. 22.5%), with similar cardiovascular (10.5% vs. 9.5%) and infection-related mortality (3.0% vs. 4.4%). These results were not modified in a sensitivity analysis in the unmatched population by a Cox-regression analysis that included all the appropriate predictors.
Therefore, we believe there is not enough evidence to support the preference for HD over PD in SLE patients. Renal replacement therapy selection in most CKD patients requires a case-by-case evaluation by the healthcare team keeping in mind the patient preferences. It is clear that an effort should be made to transplant these patients as soon as possible due to the lower mortality achieved with renal transplantation.